J Korean Med Sci.
2021 Jan;36(1):e3. 10.3346/jkms.2021.36.e3.
Microbiological Features and Clinical Factors Associated with Empirical Antibiotic Resistance in Febrile Patients with Upper Urinary Tract Calculi
- Affiliations
-
- 1Department of Urology, Inje University Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea
- 2Department of Urology, Inje University Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea
- 3Department of Urology, Dongguk University Ilsan Hospital, Dongguk University College of Medicine, Goyang, Korea
- KMID: 2510383
- DOI: http://doi.org/10.3346/jkms.2021.36.e3
Abstract
- Background
To investigate the clinical and microbiological features of febrile patients with upper urinary tract calculi and factors that affect empirical antibiotic resistance.
Methods
A retrospective analysis was performed on 203 febrile patients hospitalized between January 2011 and December 2016 with antibiotic treatment for urinary tract infections and upper urinary tract calculi at three institutions. We collected and analyzed data, including patients' age, sex, body mass index, underlying diseases, stone-related factors, and the results of urine and blood culture examinations and antibiotic sensitivity tests.
Results
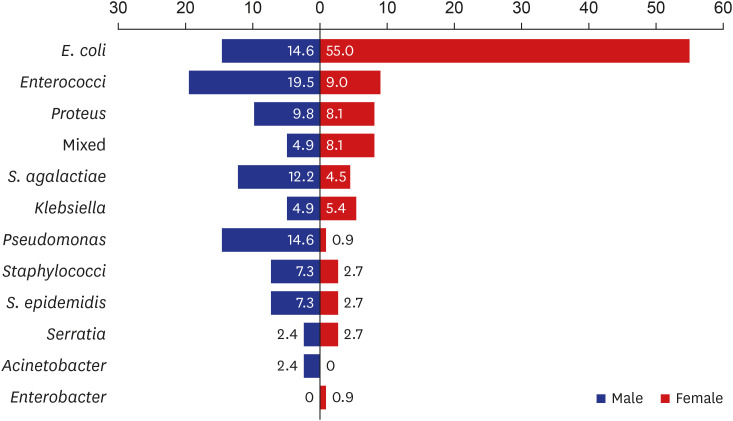
The male-to-female ratio was 1:2.3. Bacteria were identified in 152 of the 203 patients (74.9%). The most commonly cultured microorganisms included Escherichia coli (44.1%), followed by Enterococci spp. (11.8%), Proteus spp. (8.6%), Streptococcus agalactiae (6.6%), Klebsiella spp. (5.3%), Pseudomonas spp. (4.6%), coagulase-negative Staphylococcus (4.0%), Staphylococcus epidermidis (4.0%), Serratia spp. (2.6%), Enterobacter spp. (0.7%), Acinetobacter spp. (0.7%), and mixed infections (7.2%). Cultured bacterial species showed sex-specific differences. Multivariate analysis revealed that calculi's multiplicity was an independent predictive factor for quinolone resistance (P = 0.008). Recurrent infections were a significant predictor of cefotaxime resistance during multivariable analysis (P = 0.041).
Conclusion
Based on the present study results, quinolone was not recommended as the empirical treatment in febrile patients with upper urinary tract calculi. Combination antibiotic therapy is recommended in cases of recurrent infections due to the possible occurrence of cefotaxime resistance.
Figure
Reference
-
1. Patton JP, Nash DB, Abrutyn E. Urinary tract infection: economic considerations. Med Clin North Am. 1991; 75(2):495–513. PMID: 1996046.
Article2. Foxman B. Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Am J Med. 2002; 113(Suppl 1A):5S–13S.
Article3. Kennedy RP, Plorde JJ, Petersdorf RG. Studies on the epidemiology of Escherichia coli infections. IV. Evidence for a nosocomial flora. J Clin Invest. 1965; 44(2):193–201. PMID: 14260161.4. Kang CI, Kim J, Park DW, Kim BN, Ha US, Lee SJ, et al. Clinical practice guidelines for the antibiotic treatment of community-acquired urinary tract infections. Infect Chemother. 2018; 50(1):67–100. PMID: 29637759.
Article5. Bouchillon SK, Badal RE, Hoban DJ, Hawser SP. Antimicrobial susceptibility of inpatient urinary tract isolates of gram-negative bacilli in the United States: results from the study for monitoring antimicrobial resistance trends (SMART) program: 2009-2011. Clin Ther. 2013; 35(6):872–877. PMID: 23623624.
Article6. Edvardsson VO, Indridason OS, Haraldsson G, Kjartansson O, Palsson R. Temporal trends in the incidence of kidney stone disease. Kidney Int. 2013; 83(1):146–152. PMID: 22992468.
Article7. Beeson PB, Guze LB. Experimental pyelonephritis. I. Effect of ureteral ligation on the course of bacterial infection in the kidney of the rat. J Exp Med. 1956; 104(6):803–815. PMID: 13376805.8. Marien T, Mass AY, Shah O. Antimicrobial resistance patterns in cases of obstructive pyelonephritis secondary to stones. Urology. 2015; 85(1):64–68. PMID: 25530365.
Article9. Hooton TM. Clinical practice. Uncomplicated urinary tract infection. N Engl J Med. 2012; 366(11):1028–1037. PMID: 22417256.10. Levey AS, de Jong PE, Coresh J, El Nahas M, Astor BC, Matsushita K, et al. The definition, classification, and prognosis of chronic kidney disease: a KDIGO Controversies Conference report. Kidney Int. 2011; 80(1):17–28. PMID: 21150873.
Article11. Foxman B. Recurring urinary tract infection: incidence and risk factors. Am J Public Health. 1990; 80(3):331–333. PMID: 2305919.
Article12. Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, et al. Health care--associated bloodstream infections in adults: a reason to change the accepted definition of community-acquired infections. Ann Intern Med. 2002; 137(10):791–797. PMID: 12435215.
Article13. Kittanamongkolchai W, Vaughan LE, Enders FT, Dhondup T, Mehta RA, Krambeck AE, et al. The changing incidence and presentation of urinary stones over 3 decades. Mayo Clin Proc. 2018; 93(3):291–299. PMID: 29452705.
Article14. Liu Y, Chen Y, Liao B, Luo D, Wang K, Li H, et al. Epidemiology of urolithiasis in Asia. Asian J Urol. 2018; 5(4):205–214. PMID: 30364478.
Article15. Tae BS, Balpukov U, Cho SY, Jeong CW. Eleven-year cumulative incidence and estimated lifetime prevalence of urolithiasis in Korea: a National Health Insurance Service-national sample cohort based study. J Korean Med Sci. 2018; 33(2):e13. PMID: 29215822.
Article16. Hamasuna R, Takahashi S, Nagae H, Kubo T, Yamamoto S, Arakawa S, et al. Obstructive pyelonephritis as a result of urolithiasis in Japan: diagnosis, treatment and prognosis. Int J Urol. 2015; 22(3):294–300. PMID: 25400222.
Article17. Ronald A. The etiology of urinary tract infection: traditional and emerging pathogens. Am J Med. 2002; 113(Suppl 1A):14S–19S. PMID: 12113867.
Article18. Buonaiuto VA, Marquez I, De Toro I, Joya C, Ruiz-Mesa JD, Seara R, et al. Clinical and epidemiological features and prognosis of complicated pyelonephritis: a prospective observational single hospital-based study. BMC Infect Dis. 2014; 14(1):639. PMID: 25492862.
Article19. Pricop C, Dorobăt C, Puia D, Orsolya M. Antibiotic prophylaxis in retrograde ureteroscopy: what strategy should we adopt? Germs. 2013; 3(4):115–121. PMID: 24432295.
Article20. Talan DA, Krishnadasan A, Abrahamian FM, Stamm WE, Moran GJ. EMERGEncy ID NET Study Group. Prevalence and risk factor analysis of trimethoprim-sulfamethoxazole- and fluoroquinolone-resistant Escherichia coli infection among emergency department patients with pyelonephritis. Clin Infect Dis. 2008; 47(9):1150–1158. PMID: 18808361.21. Aguilar-Duran S, Horcajada JP, Sorlí L, Montero M, Salvadó M, Grau S, et al. Community-onset healthcare-related urinary tract infections: comparison with community and hospital-acquired urinary tract infections. J Infect. 2012; 64(5):478–483. PMID: 22285591.
Article22. Gupta K, Hooton TM, Naber KG, Wullt B, Colgan R, Miller LG, et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis. 2011; 52(5):e103–20. PMID: 21292654.
Article23. Rodríguez-Baño J, Alcalá JC, Cisneros JM, Grill F, Oliver A, Horcajada JP, et al. Community infections caused by extended-spectrum beta-lactamase-producing Escherichia coli . Arch Intern Med. 2008; 168(17):1897–1902. PMID: 18809817.24. Azap OK, Arslan H, Serefhanoğlu K, Colakoğlu S, Erdoğan H, Timurkaynak F, et al. Risk factors for extended-spectrum beta-lactamase positivity in uropathogenic Escherichia coli isolated from community-acquired urinary tract infections. Clin Microbiol Infect. 2010; 16(2):147–151. PMID: 19689464.25. Bader MS, Loeb M, Brooks AA. An update on the management of urinary tract infections in the era of antimicrobial resistance. Postgrad Med. 2017; 129(2):242–258. PMID: 27712137.
Article26. Geerlings S, van Nieuwkoop C, van Haarst E, van Buren M, Knotterus BJ, Stobberingh EE, et al. SWAB Guidelines for Antimicrobial Therapy of Complicated Urinary Tract Infections in Adults. place unknown: Stichting Werkgroep AntibioticaBeleid (SWAB);2013.27. Buehrle DJ, Shields RK, Chen L, Hao B, Press EG, Alkrouk A, et al. Evaluation of the in vitro activity of ceftazidime-avibactam and ceftolozane-tazobactam against meropenem-resistant pseudomonas aeruginosa isolates. Antimicrob Agents Chemother. 2016; 60(5):3227–3231. PMID: 26976862.28. Pfaller MA, Bassetti M, Duncan LR, Castanheira M. Ceftolozane/tazobactam activity against drug-resistant Enterobacteriaceae and Pseudomonas aeruginosa causing urinary tract and intraabdominal infections in Europe: report from an antimicrobial surveillance programme (2012-15). J Antimicrob Chemother. 2017; 72(5):1386–1395. PMID: 28165526.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The inter-relationship between the pain and urinary tract calculi
- Chemical Analysis on Urinary Calculi
- A Statistical Observation on Urolithiasis
- Dorsovertical Lumbotomy for Surgery of Upper Urinary Tract Calculi
- Clinical Characteristics and Antibiotic Resistance of Urinary Tract Infections in Children: Escherichia. coli Versus Non-E. coli