Korean J Women Health Nurs.
2020 Dec;26(4):300-317. 10.4069/kjwhn.2020.12.13.
The effects of diagnostic hysteroscopy on the reproductive outcomes of infertile women without intrauterine pathologies: a systematic review and meta-analysis
- Affiliations
-
- 1Department of Medical Device Management and Research and Samsung Advanced Institute for Health Sciences & Technology, Sungkyunkwan University, Seoul, Korea
- 2Department of Obstetrics and Gynecology, Gachon University Gil Hospital, Gachon University of Medicine and Science, Incheon, Korea
- 3Department of Nursing Science, College of Nursing, Gachon University, Incheon, Korea
- KMID: 2510367
- DOI: http://doi.org/10.4069/kjwhn.2020.12.13
Abstract
- Purpose
Hysteroscopy can be used both to diagnose and to treat intrauterine pathologies. It is well known that hysteroscopy helps to improve reproductive outcomes by treating intrauterine pathologies. However, it is uncertain whether hysteroscopy is helpful in the absence of intrauterine pathologies. This study aimed to confirm whether hysteroscopy improves the reproductive outcomes of infertile women without intrauterine pathologies.
Methods
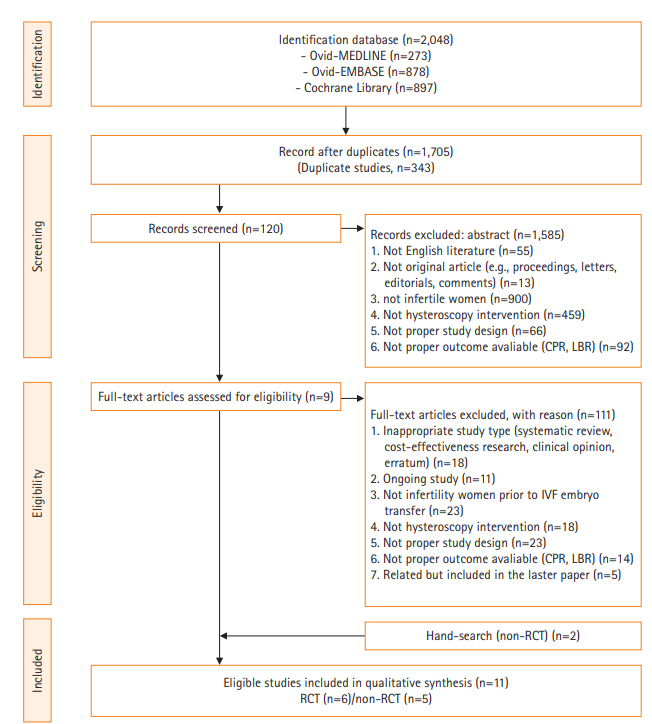
We conducted a systematic review of 11 studies retrieved from Ovid-MEDLINE, Ovid-Embase, and the Cochrane Library. Two independent investigators extracted the data and used risk-of-bias tools (RoB 2.0 and ROBINS-I) to assess their quality.
Results
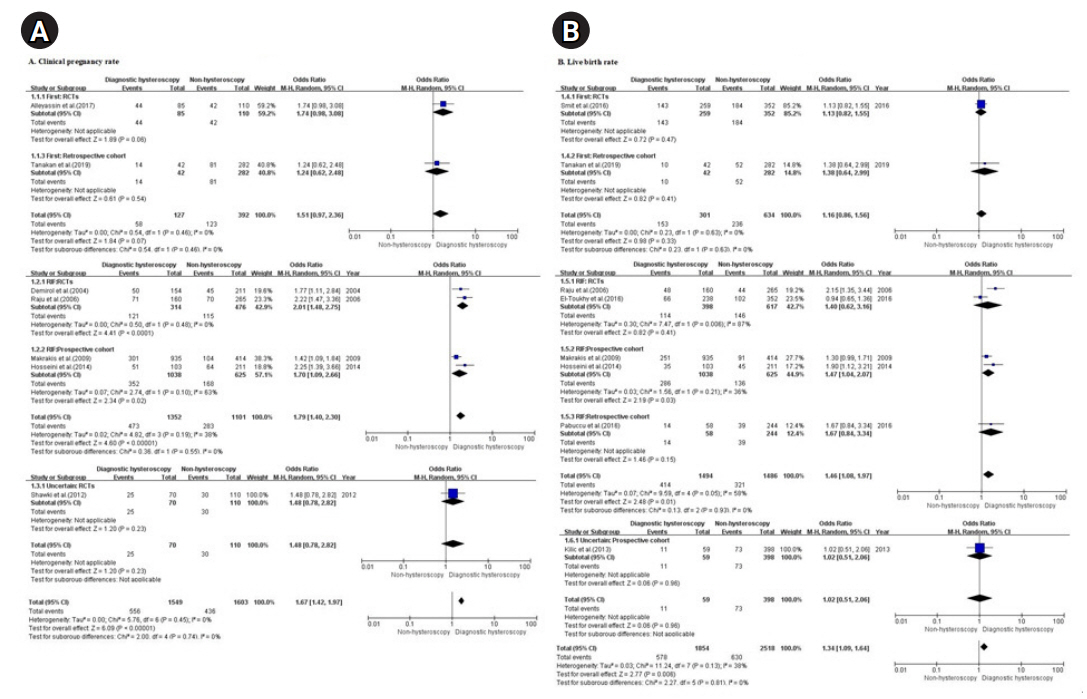
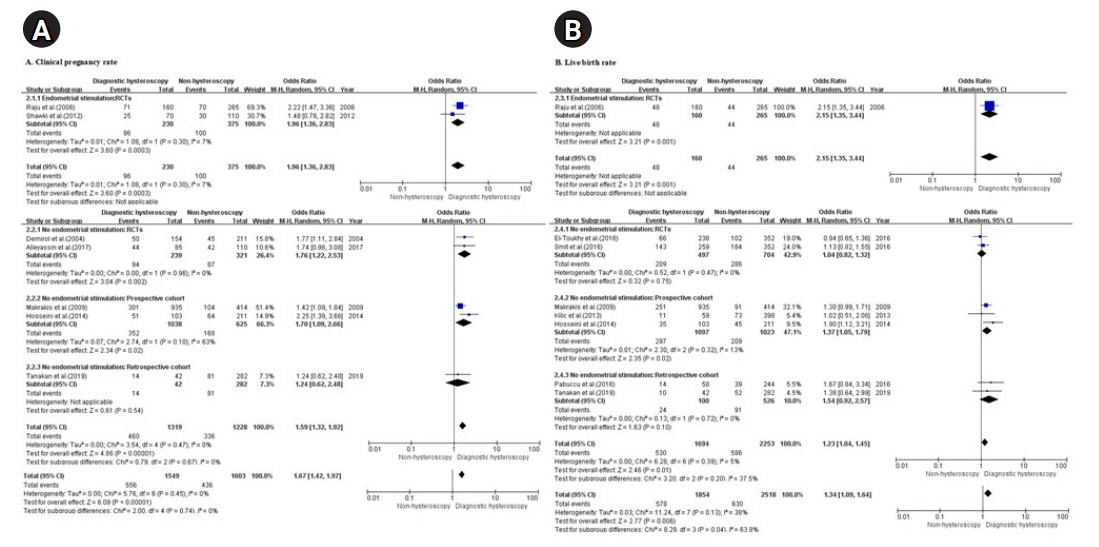
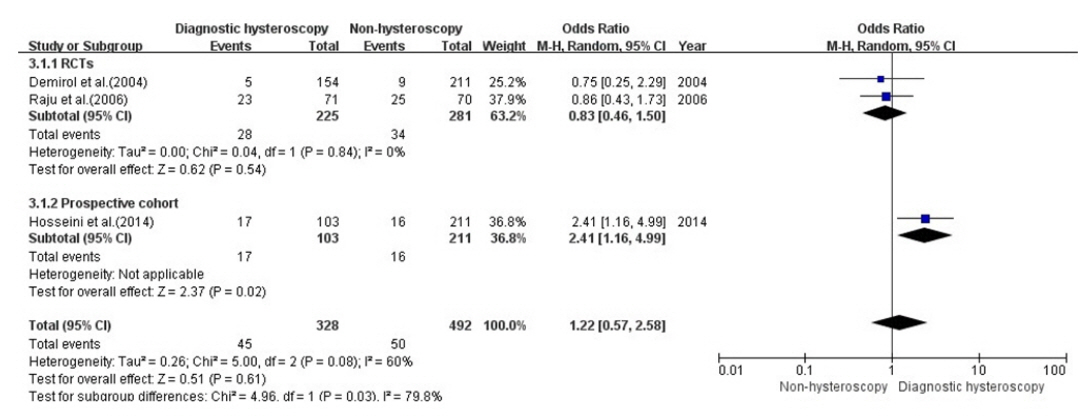
Diagnostic hysteroscopy prior to in vitro fertilization (IVF)/intracytoplasmic sperm injection (ICSI) was associated with a higher clinical pregnancy rate (CPR) and live birth rate (LBR) than non-hysteroscopy in patients with recurrent implantation failure (RIF) (odds ratio, 1.79 and 1.46; 95% confidence interval, 1.40–2.30 and 1.08–1.97 for CPR and LBR, respectively) while hysteroscopy prior to first IVF was ineffective. The overall meta-analysis of LBR showed statistically significant findings for RIF, but a subgroup analysis showed effects only in prospective cohorts (odds ratio, 1.40 and 1.47; 95% confidence interval, 0.86–1.56 and 1.04–2.07 for randomized controlled trials and prospective cohorts, respectively). Therefore, the LBR should be interpreted carefully and further research is needed.
Conclusion
Although further research is warranted, hysteroscopy may be considered as a diagnostic and treatment option for infertile women who have experienced RIF regardless of intrauterine pathologies. This finding enables nurses to educate and support infertile women with RIF prior to IVF/ICSI.
Figure
Reference
-
References
1. Zegers-Hochschild F, Adamson GD, Dyer S, Racowsky C, de Mouzon J, Sokol R, et al. The International Glossary on Infertility and Fertility Care, 2017. Hum Reprod. 2017; 32(9):1786–1801. https://doi.org/10.1093/humrep/dex234.
Article2. Kamel RM. Management of the infertile couple: an evidence-based protocol. Reprod Biol Endocrinol. 2010; 8:21. https://doi.org/10.1186/1477-7827-8-21.
Article3. Sun H, Gong TT, Jiang YT, Zhang S, Zhao YH, Wu QJ. Global, regional, and national prevalence and disability-adjusted life-years for infertility in 195 countries and territories, 1990-2017: results from a global burden of disease study, 2017. Aging (Albany NY). 2019; 11(23):10952–10991. https://doi.org/10.18632/aging.102497.
Article4. Sadeghi MR. Low success rate of ART, an illusion, a reality or simply a too high expectation? J Reprod Infertil. 2012; 13(3):123.5. Centers for Disease Control and Prevention. 2017 assisted reproductive technology fertility clinic success rates report. Atlanta (GA): US Dept of Health and Human Services,;2019.6. Timeva T, Shterev A, Kyurkchiev S. Recurrent implantation failure: the role of the endometrium. J Reprod Infertil. 2014; 15(4):173–183.7. Toth B, Würfel W, Germeyer A, Hirv K, Makrigiannakis A, Strowitzki T. Disorders of implantation--are there diagnostic and therapeutic options? J Reprod Immunol. 2011; 90(1):117–123. https://doi.org/10.1016/j.jri.2011.05.002.
Article8. Moini A, Kiani K, Ghaffari F, Hosseini F. Hysteroscopic findings in patients with a history of two implantation failures following in vitro fertilization. Int J Fertil Steril. 2012; 6(1):27–30.9. Pundir J, El Toukhy T. Uterine cavity assessment prior to IVF. Womens Health (Lond). 2010; 6(6):841–848. https://doi.org/10.2217/whe.10.61.
Article10. Pundir J, Pundir V, Omanwa K, Khalaf Y, El-Toukhy T. Hysteroscopy prior to the first IVF cycle: a systematic review and meta-analysis. Reprod Biomed Online. 2014; 28(2):151–161. https://doi.org/10.1016/j.rbmo.2013.09.025.
Article11. Chiofalo B, Palmara V, Vilos GA, Pacheco LA, Lasmar RB, Shawki O, et al. Reproductive outcomes of infertile women undergoing “see and treat” office hysteroscopy: a retrospective observational study. Minim Invasive Ther Allied Technol. 2019 Dec 19 [Epub]. https://doi.org/10.1080/13645706.2019.1705352.
Article12. Rudic Biljic-Erski I, Vasiljevic V, Rakic S, Mihajlovic S, Smiljkovic OD. The impact of hysteroscopic myomectomy on fertility and pregnancy outcomes of infertile women according characteristics of submucous fibroids. Clin Exp Obstet Gynecol. 2019; 46(2):235–240. https://doi.org/10.12891/ceog4509.2019.
Article13. Wang X, Hou H, Yu Q. Fertility and pregnancy outcomes following hysteroscopic metroplasty of different sized uterine septa: a retrospective cohort study protocol. Medicine (Baltimore). 2019; 98(30):e16623. https://doi.org/10.1097/MD.0000000000016623.
Article14. Di Spiezio Sardo A, Di Carlo C, Minozzi S, Spinelli M, Pistotti V, Alviggi C, et al. Efficacy of hysteroscopy in improving reproductive outcomes of infertile couples: a systematic review and meta-analysis. Hum Reprod Update. 2016; 22(4):479–496. https://doi.org/10.1093/humupd/dmw008.
Article15. Cao H, You D, Yuan M, Xi M. Hysteroscopy after repeated implantation failure of assisted reproductive technology: a meta-analysis. J Obstet Gynaecol Res. 2018; 44(3):365–373. https://doi.org/10.1111/jog.13571.
Article16. Kamath MS, Bosteels J, D’Hooghe TM, Seshadri S, Weyers S, Mol BW, et al. Screening hysteroscopy in subfertile women and women undergoing assisted reproduction. Cochrane Database Syst Rev. 2019; 4(4):CD012856. https://doi.org/10.1002/14651858.CD012856.pub2.
Article17. Mao X, Wu L, Chen Q, Kuang Y, Zhang S. Effect of hysteroscopy before starting in-vitro fertilization for women with recurrent implantation failure: a meta-analysis and systematic review. Medicine (Baltimore). 2019; 98(7):e14075. https://doi.org/10.1097/MD.0000000000014075.
Article18. El-Toukhy T, Sunkara SK, Coomarasamy A, Grace J, Khalaf Y. Outpatient hysteroscopy and subsequent IVF cycle outcome: a systematic review and meta-analysis. Reprod Biomed Online. 2008; 16(5):712–719. https://doi.org/10.1016/s1472-6483(10)60486-5.
Article19. Pabuccu R, Ceyhan ST, Onalan G, Goktolga U, Ercan CM, Selam B. Successful treatment of cervical stenosis with hysteroscopic canalization before embryo transfer in patients undergoing IVF: a case series. J Minim Invasive Gynecol. 2005; 12(5):436–438. https://doi.org/10.1016/j.jmig.2005.06.003.
Article20. Gnainsky Y, Granot I, Aldo P, Barash A, Or Y, Mor G, et al. Biopsy-induced inflammatory conditions improve endometrial receptivity: the mechanism of action. Reproduction. 2015; 149(1):75–85. https://doi.org/10.1530/REP-14-0395.
Article21. Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2.0: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019; 366:14898. https://doi.org/10.1136/bmj.l4898.
Article22. Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016; 355:i4919. https://doi.org/10.1136/bmj.i4919.
Article23. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. 2000; 283(15):2008–2012. https://doi.org/10.1001/jama.283.15.2008.
Article24. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986; 7(3):177–188. https://doi.org/10.1016/0197-2456(86)90046-2.
Article25. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002; 21(11):1539–1558. https://doi.org/10.1002/sim.1186.
Article26. Demirol A, Gurgan T. Effect of treatment of intrauterine pathologies with office hysteroscopy in patients with recurrent IVF failure. Reprod Biomed Online. 2004; 8(5):590–594. https://doi.org/10.1016/s1472-6483(10)61108-x.
Article27. Rama Raju GA, Shashi Kumari G, Krishna KM, Prakash GJ, Madan K. Assessment of uterine cavity by hysteroscopy in assisted reproduction programme and its influence on pregnancy outcome. Arch Gynecol Obstet. 2006; 274(3):160–164. https://doi.org/10.1007/s00404-006-0174-7.
Article28. Makrakis E, Hassiakos D, Stathis D, Vaxevanoglou T, Orfanoudaki E, Pantos K. Hysteroscopy in women with implantation failures after in vitro fertilization: findings and effect on subsequent pregnancy rates. J Minim Invasive Gynecol. 2009; 16(2):181–187. https://doi.org/10.1016/j.jmig.2008.12.016.
Article29. Shawki HE, Elmorsy M, Eissa MK. Routine office hysteroscopy prior to ICSI and its impact on assisted reproduction program outcome: a randomized controlled trial. Middle East Fertil Soc J. 2012; 17(1):14–21. https://doi.org/10.1016/j.mefs.2011.04.005.
Article30. Kilic Y, Bastu E, Ergun B. Validity and efficacy of office hysteroscopy before in vitro fertilization treatment. Arch Gynecol Obstet. 2013; 287(3):577–581. https://doi.org/10.1007/s00404-012-2584-z.
Article31. Hosseini MA, Ebrahimi N, Mahdavi A, Aleyasin A, Safdarian L, Fallahi P, et al. Hysteroscopy in patients with repeated implantation failure improves the outcome of assisted reproductive technology in fresh and frozen cycles. J Obstet Gynaecol Res. 2014; 40(5):1324–1330. https://doi.org/10.1111/jog.12315.
Article32. El-Toukhy T, Campo R, Khalaf Y, Tabanelli C, Gianaroli L, Gordts SS, et al. Hysteroscopy in recurrent in-vitro fertilisation failure (TROPHY): a multicentre, randomised controlled trial. Lancet. 2016; 387(10038):2614–2621. https://doi.org/10.1016/S0140-6736(16)00258-0.
Article33. Pabuçcu EG, Yalçın İ, Bodur T, Çağlar GS, Pabuçcu R. Impact of office hysteroscopy in repeated implantation failure: experience of a single center. J Turk Ger Gynecol Assoc. 2016; 17(4):197–200. https://doi.org/10.5152/jtgga.2016.16166.
Article34. Smit JG, Kasius JC, Eijkemans MJ, Koks CA, van Golde R, Nap AW, et al. Hysteroscopy before in-vitro fertilisation (inSIGHT): a multicentre, randomised controlled trial. Lancet. 2016; 387(10038):2622–2629. https://doi.org/10.1016/S0140-6736(16)00231-2.
Article35. Alleyassin A, Abiri A, Agha-Hosseini M, Sarvi F. The value of routine hysteroscopy before the first intracytoplasmic sperm injection treatment cycle. Gynecol Obstet Invest. 2017; 82(2):125–130. https://doi.org/10.1159/000445801.
Article36. Tanacan A, Mumusoglu S, Yarali H, Bozdag G. The effect of performing hysteroscopy prior to the first in vitro fertilization (IVF) cycle on live birth rate. Gynecol Endocrinol. 2019; 35(5):443–447. https://doi.org/10.1080/09513590.2018.1534953.
Article37. El-Toukhy T, Sunkara S, Khalaf Y. Local endometrial injury and IVF outcome: a systematic review and meta-analysis. Reprod Biomed Online. 2012; 25(4):345–354. https://doi.org/10.1016/j.rbmo.2012.06.012.
Article38. Saleh DM, El Ashal G, Elsherif S, Awad SS, Mahmoud MM, Gohar MS, et al. Routine use of hysteroscopy before in-vitro fertilization: Systematic review and meta-analysis of randomized controlled trials. EBWHJ. 2019; 9(4):533–541. https://doi.org/10.21608/ebwhj.2019.64356.
Article39. Aghahosseini M, Ebrahimi N, Mahdavi A, Aleyasin A, Safdarian L, Sina S. Hysteroscopy prior to assisted reproductive technique in women with recurrent implantation failure improves pregnancy likelihood. Fertil Steril. 2012; 98(3 Suppl 1):S4. https://doi.org/10.1016/j.fertnstert.2012.07.015.
Article40. Vitagliano A, Saccardi C, Noventa M, Di Spiezio Sardo A, Laganà AS, Litta PS. Does endometrial scratching really improve intrauterine insemination outcome? Injury timing can make a huge difference. J Gynecol Obstet Hum Reprod. 2018; 47(1):33–34. https://doi.org/10.1016/j.jogoh.2017.11.001.
Article41. Mirkin S, Arslan M, Churikov D, Corica A, Diaz JI, Williams S, et al. In search of candidate genes critically expressed in the human endometrium during the window of implantation. Hum Reprod. 2005; 20(8):2104–2117. https://doi.org/10.1093/humrep/dei051.
Article42. Almog B, Shalom-Paz E, Dufort D, Tulandi T. Promoting implantation by local injury to the endometrium. Fertil Steril. 2010; 94(6):2026–2029. https://doi.org/10.1016/j.fertnstert.2009.12.075.
Article43. Barash A, Dekel N, Fieldust S, Segal I, Schechtman E, Granot I. Local injury to the endometrium doubles the incidence of successful pregnancies in patients undergoing in vitro fertilization. Fertil Steril. 2003; 79(6):1317–1322. https://doi.org/10.1016/s0015-0282(03)00345-5.
Article44. Shohayeb A, El-Khayat W. Does a single endometrial biopsy regimen (S-EBR) improve ICSI outcome in patients with repeated implantation failure? A randomised controlled trial. Eur J Obstet Gynecol Reprod Biol. 2012; 164(2):176–179. https://doi.org/10.1016/j.ejogrb.2012.06.029.
Article45. Ubaldi F, Bourgain C, Tournaye H, Smitz J, Van Steirteghem A, Devroey P. Endometrial evaluation by aspiration biopsy on the day of oocyte retrieval in the embryo transfer cycles in patients with serum progesterone rise during the follicular phase. Fertil Steril. 1997; 67(3):521–526. https://doi.org/10.1016/s0015-0282(97)80080-5.
Article46. Li R, Wang R, Zhou L, Hongyang W. Local injury of the proliferative phase endometrium substantially increase the ER expression in following secretory phase endometrium. Fertil Steril. 2008; 90 Suppl:S162–S163. https://doi.org/10.1016/j.fertnstert.2008.07.374.
Article47. Li R, Hao G. Local injury to the endometrium: its effect on implantation. Curr Opin Obstet Gynecol. 2009; 21(3):236–239. https://doi.org/10.1097/GCO.0b013e32832a0654.
Article48. Finn CA, Pope M. Vascular and cellular changes in the decidualized endometrium of the ovariectomized mouse following cessation of hormone treatment: a possible model for menstruation. J Endocrinol. 1984; 100(3):295–300. https://doi.org/10.1677/joe.0.1000295.
Article49. Simón C, Bellver J. Scratching beneath ‘The Scratching Case’: systematic reviews and meta-analyses, the back door for evidence-based medicine. Hum Reprod. 2014; 29(8):1618–1621. https://doi.org/10.1093/humrep/deu126.
Article50. Takahashi K, Mukaida T, Tomiyama T, Oka C. High pregnancy rate after hysteroscopy with irrigation in uterine cavity prior to blastocyst transfer in patients who have failed to conceive after blastocyst transfer. Fertil Steril. 2000; 74(3 Suppl 1):S206. https://doi.org/10.1016/S0015-0282(00)01328-5.
Article51. Mansour RT, Aboulghar MA. Optimizing the embryo transfer technique. Hum Reprod. 2002; 17(5):1149–1153. https://doi.org/10.1093/humrep/17.5.1149.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Use of Sonohysterography in Infertile Patients
- Effects of First Assisted Reproductive Technologies on Anxiety and Depression among InfertileWomen: A Systematic Review and Meta-Analysis
- Impact of Varicocele Repair on Assisted Reproductive Technique Outcomes in Infertile Men: A Systematic Review and Meta-Analysis
- Effects of Mind–Body Programs on Infertile Women: A Systematic Review and Meta-analysis of Randomized Controlled Trials
- A Clinical Usefulness of Office Hysteroscopy