Korean J healthc assoc Infect Control Prev.
2020 Dec;25(2):146-153. 10.14192/kjicp.2020.25.2.146.
The Seroprevalence and Vaccination Status for Infectious Diseases in Nursing Students before Clinical Practice
- Affiliations
-
- 1College of Nursing, Woosuk University, Wanju, Korea
- 2College of Nursing, Jeonbuk National University, Jeonju, Korea
- KMID: 2510140
- DOI: http://doi.org/10.14192/kjicp.2020.25.2.146
Abstract
- Background
This study aimed to investigate the seroprevalence of anti-Hepatitis B virus, anti-Hepatitis A virus, and chickenpox in nursing students before the initiation of their clinical practice, nursing students in medical institutions, the current immunization status of those without antibodies for measles-mumps-rubella and influenza.
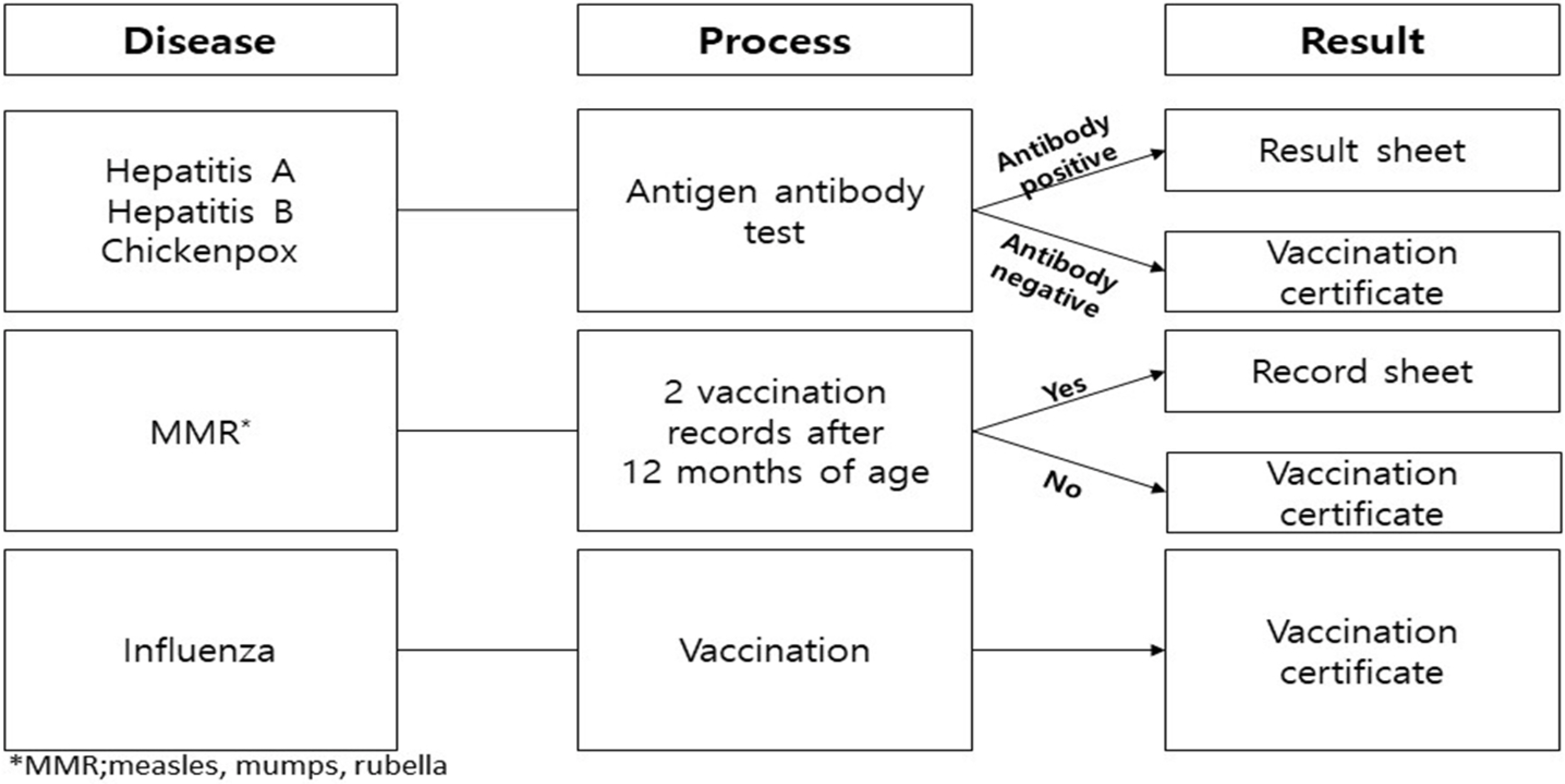
Methods
The data was collected using the result sheet and vaccination certificate. This study investigated the seroprevalence of hepatitis B, hepatitis A, chickenpox, vaccination status of those who have not formed antibodies, and vaccination status of measles, mumps, rubella, and influenza before the clinical practice of second-year nursing college students in the Jeonbuk region from 2014 to 2018.
Results
A total of 461 students were included in this study. The results indicated that seroprevalence was 25.8-35.6% for hepatitis B, 10.3-34.4% for hepatitis A, and 54.0-73.0% for chickenpox. Those who have not formed antibodies received the 1st and 2nd vaccination, but it did not confirm whether they received complete immunization. Vaccination of measles, mumps, rubella, and influenza was 100%.
Conclusion
Nursing students got vaccination after checking whether antibodies of preventable infectious diseases were formed before clinical practice. Therefore, this is expected to have a preventive effect against these diseases during the clinical practice period.
Figure
Reference
-
1. Choi JR, Ko IS, Yim YY. 2016; Factors influencing nursing students' performance of infection control. J Korean Acad Fundam Nurs. 23:136–48. DOI: 10.7739/jkafn.2016.23.2.136.
Article2. Kuhar DT, Carrico R, Cox K, de Perio MA, Irwin KL, Lundstrom T, et al. 2019; Infection control in healthcare personnel: infrastructure and routine practices for occupational infection prevention and control services. Antlanta; Centers for Disease Control and Prevention. 31–3.3. Jeong MH. 2015; Survey of exposure to blood and body fluids, knowledge, awareness and performance on standard precautions of infection control in nursing students. J Korea Contents Assoc. 15:316–29. DOI: 10.5392/JKCA.2015.15.04.316.
Article4. Park JH, Chon HK, Jeong SH, Hwang JH, Lee CS, Lee HB. 2010; Nursing students' exposure to blood and body fluids in clinical practicum. J East-West Nurs Res. 16:70–5.5. Katsevman GA, Sedney CL, Braca Iii JA, Hatchett L. 2020; Interdisciplinary differences in needlestick injuries among healthcare professionals in training: improving situational awareness to prevent high-risk injuries. Work. 65:635–45. DOI: 10.3233/WOR-203118. PMID: 32116282.
Article6. Veronesi L, Giudice L, Agodi A, Arrigoni C, Baldovin T, Barchitta M, et al. 2018; A multicentre study on epidemiology and prevention of needle stick injuries among students of nursing schools. Ann Ig. 30(5 Supple 2):99–110.7. Zhang X, Chen Y, Li Y, Hu J, Zhang C, Li Z, et al. 2018; Needlestick and sharps injuries among nursing students in Nanjing, China. Workplace Health Saf. 66:276–84. DOI: 10.1177/2165079917732799. PMID: 29073827.
Article8. Kim YC, Choi YH. 2019; Current and prospect on measles outbreak. Korean J Med. 94:237–45. DOI: 10.3904/kjm.2019.94.3.237.
Article9. Korea Disease Control and Prevention Agency. Dynamics and management of infectious diseases subject to immunization. http://www.kdca.go.kr/npt/biz/npp/portal/nppLwcrIcdMain.do . Updated on 9 December 2020.10. Ödemiş Í, Köse Ş, Akbulut Í, Albayrak H. 2019; Seroprevalence of measles, mumps, rubella, and varicella zoster virus antibodies among healthcare students: analysis of vaccine efficacy and cost-effectiveness. Rev Esp Quimioter. 32:525–31.11. Arunkumar G, Vandana KE, Sathiakumar N. 2013; Prevalence of measles, mumps, rubella, and varicella susceptibility among health science students in a University in India. Am J Ind Med. 56:58–64. DOI: 10.1002/ajim.22046. PMID: 22467356. PMCID: PMC3415600.
Article12. Park JH, Shon JA. 2016; Seroprevalence of anti-hepatitis B virus, anti-hepatitis A virus, and anti-varicella zoster virus antibodies in nursing students from 2009 to 2013. Korean J Nosocomial Infect Control. 21:31–6. DOI: 10.14192/kjnic.2016.21.1.31.
Article13. Ji SK, Jang SH, Park MH, Lee JE, Jeong HS, Park J, et al. 2020; A study on seroprevalence of hepatitis A virus among healthcare workers at a university-affiliated hospital in Deajeon, Korea. Korean J Healthc Assoc Infect Control Prev. 25:54–9. DOI: 10.14192/kjicp.2020.25.1.54.
Article14. Korea Disease Control and Prevention Agency. Guidelines for adult immunization 2018. http://www.kdca.go.kr/board.es?.mid=a20507020000&bid=0019&act=view&list_no=142157 . Updated on 18 November 2019.15. Korean Accreditation Board of Nursing Education. 2019. College manual for nursing education certification evaluation in the first half of 2019. Korean Accreditation Board of Nursing Education;Seoul: 71.16. Lindley MC, Lorick SA, Spinner JR, Krull AR, Mootrey GT, Ahmed F, et al. 2011; Student vaccination requirements of U.S. health professional schools: a survey. Ann Intern Med. 154:391–400. DOI: 10.7326/0003-4819-154-6-201103150-00004. PMID: 21403075.
Article17. Miller BL, Lindley MC, Ahmed F, Wortley PM. 2011; Student immunity requirements of health professional schools: vaccination and other means of fulfillment-United States, 2008. Infect Control Hosp Epidemiol. 32:908–11. DOI: 10.1086/661785. PMID: 21828972.
Article18. Loulergue P, Fonteneau L, Armengaud JB, Momcilovic S, Levy-Brühl D, Launay O, et al. 2013; Vaccine coverage of healthcare students in hospitals of the Paris region in 2009: the Studyvax survey. Vaccine. 31:2835–8. DOI: 10.1016/j.vaccine.2013.04.004. PMID: 23623864.
Article19. Shin YY. Incheon: Incheon Catholic University; 2020.20. Korean Society for Nosocomial Infection Control. 2017. Infection control and prevention in healthcare facilities. 5th ed. Hanmi Medical Publishing;Seoul: p. 873–4.21. Korea Disease Control and Prevention Agency. Guidelines for the management of influenza national vaccination support projects. https://nip.cdc.go.kr/irgd/reference.do?.service=getGuideView&strNum=155&GUISEQNUM=155 . Updated on 9 September 2019.22. Kim JR, Lee KT, Chong MS. 2020; A convergence study on the positive rate of hepatitis B surface antibody by age before and after HBV vaccination. J Korea Converg Soc. 11:77–82.23. Korea Disease Control and Prevention Agency. Infectious disease portal. https://nip.cdc.go.kr/irgd/index.html . Updated on 9 December 2020.24. Lee JS. Gwangju: Chonnam National University; 2020.25. Kellie SM, Makvandi M, Muller ML. 2011; Management and outcome of a varicella exposure in a neonatal intensive care unit: lessons for the vaccine era. Am J Infect Control. 39:844–8. DOI: 10.1016/j.ajic.2011.02.006. PMID: 21600672.
Article26. Korea Disease Control and Prevention. 2008. Effective management of vaccination registration data and development of quality improvement measures. http://www.kdca.go.kr/board.es?mid=a40801000000&bid=0050&act=view&list_no=1401. Updated on 1 December 2020.27. Korea Disease Control and Prevention Agency. Vaccination certificate. https://nip.cdc.go.kr/irgd/index.html . Updated on 9 December 2020.28. Kim OS. 2019; Convergence study on the influence of vaccination encouragement and perception of influenza preventability on influenza vaccination practice among university students. J Converg Inf Technol. 9:74–82.29. Chang SJ, Park JH. 2018; Knowledge, attitudes and compliance regarding infection preventive behaviors for MERS among staff in long-term care hospitals. J Korea Acad Ind Cooper Soc. 19:334–44.30. Cheong HJ, Sohn JW, Choi SJ, Eom JS, Woo HJ, Chun BC, et al. 2004; Factors influencing decision regarding influenza vaccination: a survey of healthcare workers in one hospital. Infect Chemother. 36:213–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Seroprevalence of Anti-hepatitis B Virus, Anti-hepatitis A Virus, and Anti-varicella Zoster Virus Antibodies in Nursing Students from 2009 to 2013
- Factors Influencing University Nursing Students' Measles Vaccination Rate During a Community Measles Outbreak
- Factors Affecting Nursing Students' Activeness in Clinical Education
- Awareness, Knowledge, and Vaccination Status of Meningococcal Meningitis Vaccination: A Comparative Study on International and Korean University Students
- Status of and Factors Influencing Vaccination against the Pandemic (H1N1) 2009 Virus among University Students from the Fields of Nursing and Allied Health