Blood Res.
2020 Dec;55(4):225-245. 10.5045/br.2020.2020255.
Changing the frequency and spectra of chromosomal aberrations in Korean patients with acute leukemia in a tertiary care hospital
- Affiliations
-
- 1Department of Laboratory Medicine, Chonnam National University Medical School and Chonnam National University Hwasun Hospital, Korea
- 2Brain Korea 21 Plus program, Chonnam National University Medical School and Chonnam National University Hwasun Hospital, Hwasun, Korea
- 3Department of Laboratory Medicine, GwangYang Sarang General Hospital, Gwangyang, Korea
- 4College of Korean Medicine, Dongshin University, Naju, Korea
- KMID: 2509962
- DOI: http://doi.org/10.5045/br.2020.2020255
Abstract
- Background
Chromosomal analysis is essential for the diagnosis and risk stratification of all leukemia patients. Not surprisingly, racial differences in chromosomal aberrations (CA) in hematological malignancies could be found, and CA incidence in leukemia might change over time, possibly due to environmental and lifestyle changes. Thus, we compared the frequency and range of CA in patients with acute leukemia (AL) during two time periods (2006‒2009 vs. 2010‒2015) and compared them with other prior studies.
Methods
We enrolled 717 patients with AL during a six-year period (2010‒2015). We compared the results to those of our earlier study (2006‒2009) [1]. Conventional cytogenetics, a multiplex reverse transcriptase (RT)-PCR system, and fluorescence in situ hybridization were employed to assess bone marrow specimens or peripheral blood at the diagnostic stage in AL patients to detect CA.
Results
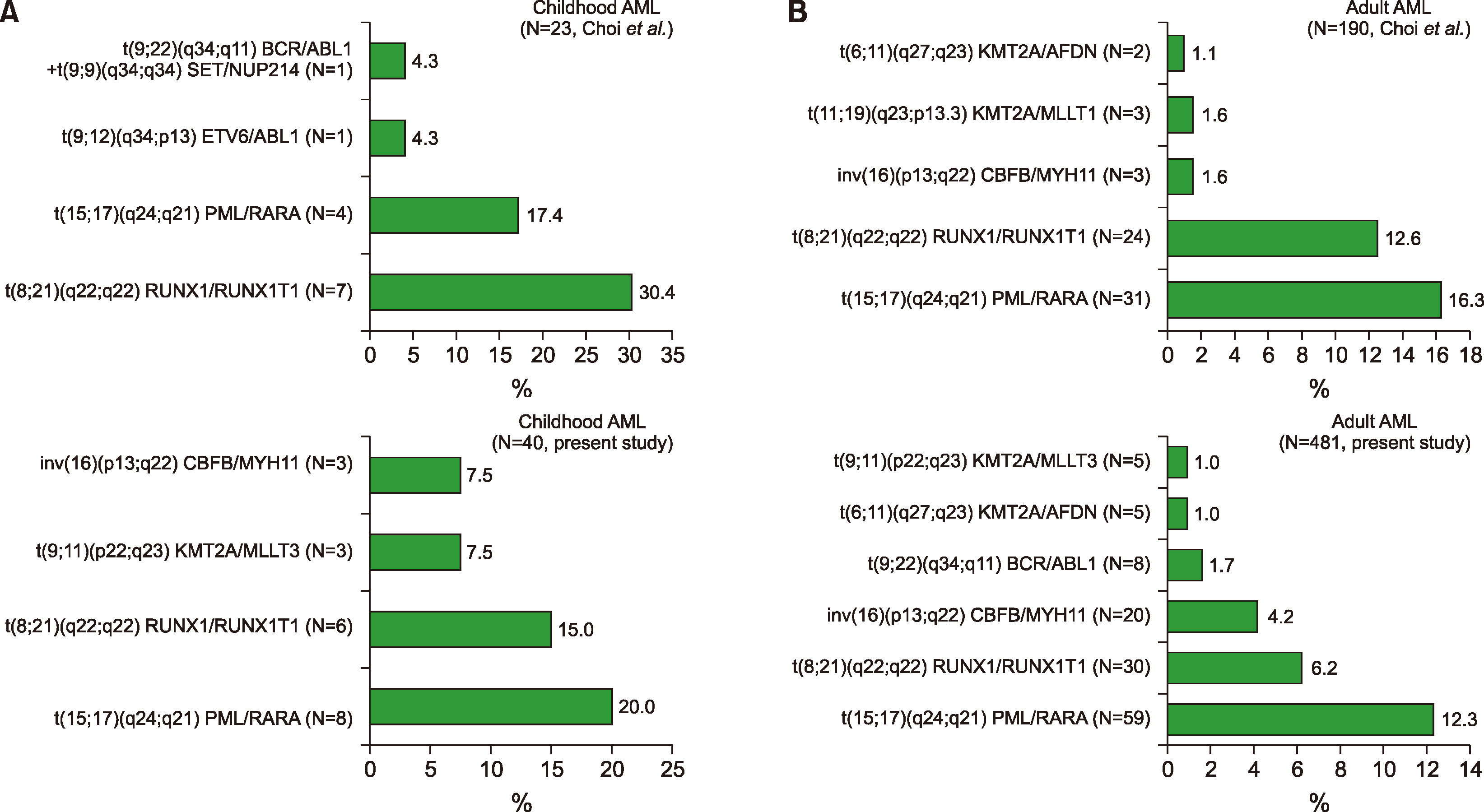
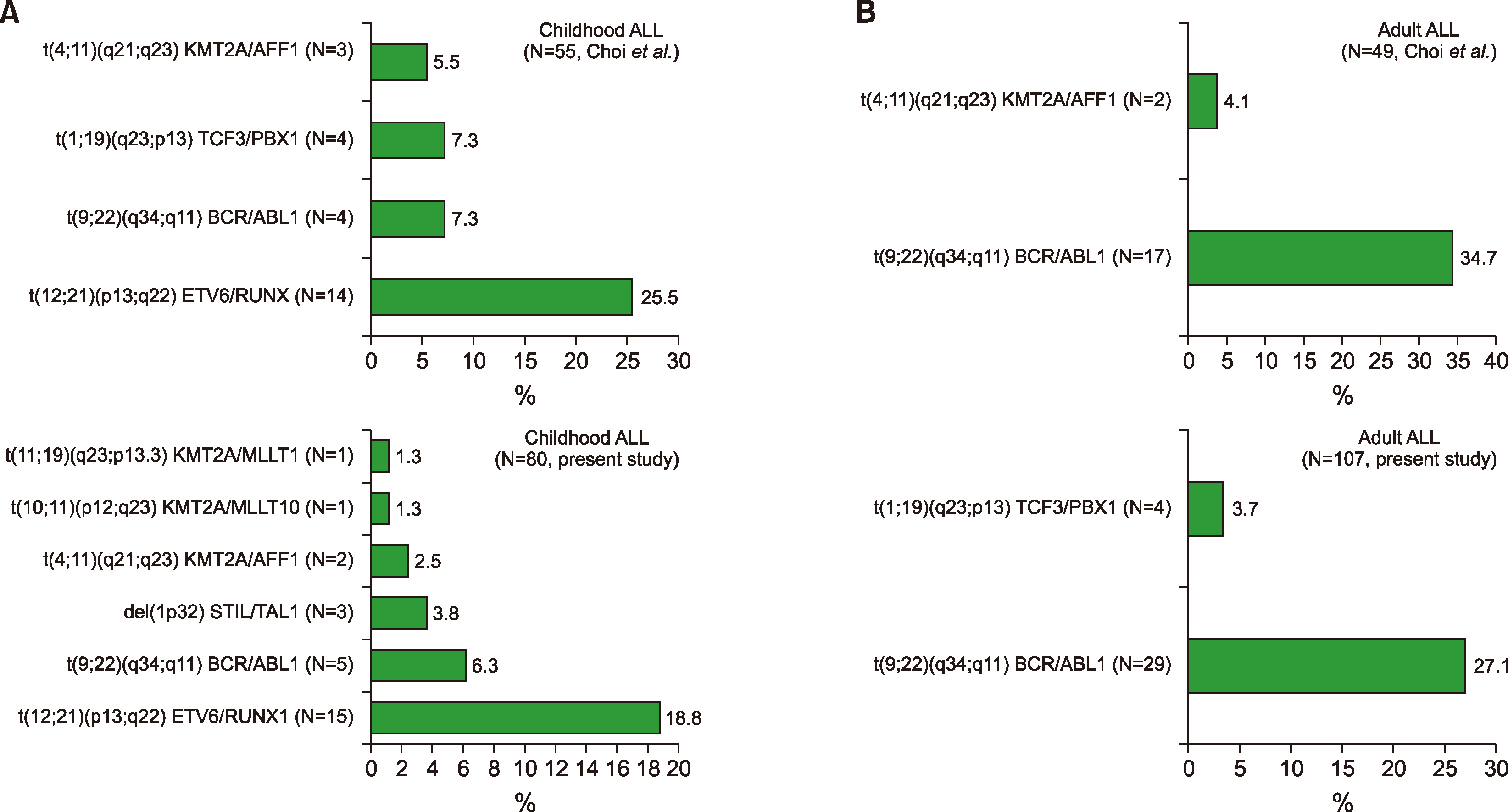
The incidence of CA changed in the leukemia subgroups during the two time periods. Notably, the most frequent CA of childhood acute myeloid leukemia (AML) was PML/RARA, and was followed by RUNX1/RUNX1T1 in the current study. In contrast, the most common CA was RUNX1/RUNX1T1 in a previous study [1] and was followed by PML/RARA. In this study, the most frequent CA of the mixed phenotype AL was BCR/ABL1, which was followed by KMT2A/MLLT3. In a previous report, [1] the most frequent CA was BCR/ABL1, which was followed by KMT2A/ELL.
Conclusion
The distribution of CA in Korean AL patients changed over time in a single institute. This change might be due to environmental and lifestyle changes.
Keyword
Figure
Reference
-
1. Choi HJ, Kim HR, Shin MG, et al. 2011; Spectra of chromosomal aberrations in 325 leukemia patients and implications for the development of new molecular detection systems. J Korean Med Sci. 26:886–92. DOI: 10.3346/jkms.2011.26.7.886. PMID: 21738341. PMCID: PMC3124718.
Article2. Bacher U, Kern W, Schnittger S, Hiddemann W, Schoch C, Haferlach T. 2005; Further correlations of morphology according to FAB and WHO classification to cytogenetics in de novo acute myeloid leukemia: a study on 2,235 patients. Ann Hematol. 84:785–91. DOI: 10.1007/s00277-005-1099-0. PMID: 16132906.
Article3. Klaus M, Haferlach T, Schnittger S, Kern W, Hiddemann W, Schoch C. 2004; Cytogenetic profile in de novo acute myeloid leukemia with FAB subtypes M0, M1, and M2: a study based on 652 cases analyzed with morphology, cytogenetics, and fluorescence in situ hybridization. Cancer Genet Cytogenet. 155:47–56. DOI: 10.1016/j.cancergencyto.2004.03.008. PMID: 15527902.
Article4. Betts DR, Ammann RA, Hirt A, et al. 2007; The prognostic significance of cytogenetic aberrations in childhood acute myeloid leukaemia. A study of the Swiss Paediatric Oncology Group (SPOG). Eur J Haematol. 78:468–76. DOI: 10.1111/j.1600-0609.2007.00854.x. PMID: 17419750.
Article5. Nakase K, Bradstock K, Sartor M, et al. 2000; Geographic heterogeneity of cellular characteristics of acute myeloid leukemia: a comparative study of Australian and Japanese adult cases. Leukemia. 14:163–8. DOI: 10.1038/sj.leu.2401638. PMID: 10637492.
Article6. Cheng Y, Wang Y, Wang H, et al. 2009; Cytogenetic profile of de novo acute myeloid leukemia: a study based on 1432 patients in a single institution of China. Leukemia. 23:1801–6. DOI: 10.1038/leu.2009.107. PMID: 19474801.
Article7. Xie Y, Davies SM, Xiang Y, Robison LL, Ross JA. 2003; Trends in leukemia incidence and survival in the United States (1973-1998). Cancer. 97:2229–35. DOI: 10.1002/cncr.11316. PMID: 12712476.
Article8. Irigaray P, Newby JA, Clapp R, et al. 2007; Lifestyle-related factors and environmental agents causing cancer: an overview. Biomed Pharmacother. 61:640–58. DOI: 10.1016/j.biopha.2007.10.006. PMID: 18055160.
Article9. Pallisgaard N, Hokland P, Riishøj DC, Pedersen B, Jørgensen P. 1998; Multiplex reverse transcription-polymerase chain reaction for simultaneous screening of 29 translocations and chromosomal aberrations in acute leukemia. Blood. 92:574–88. DOI: 10.1182/blood.V92.2.574. PMID: 9657758.
Article10. Hutchings Hoffmann M, Wirenfeldt Klausen T, Hasle H, Schmiegelow K, Brondum-Nielsen K, Johnsen HE. 2005; Multiplex reverse transcription polymerase chain reaction screening in acute myeloid leukemia detects cytogenetically unrevealed abnormalities of prognostic significance. Haematologica. 90:984–6. PMID: 15996940.11. Strehl S, König M, Mann G, Haas OA. 2001; Multiplex reverse transcriptase-polymerase chain reaction screening in childhood acute myeloblastic leukemia. Blood. 97:805–8. DOI: 10.1182/blood.V97.3.805. PMID: 11157501.
Article12. Elia L, Mancini M, Moleti L, et al. 2003; A multiplex reverse transcriptase-polymerase chain reaction strategy for the diagnostic molecular screening of chimeric genes: a clinical evaluation on 170 patients with acute lymphoblastic leukemia. Haematologica. 88:275–9. PMID: 12651265.13. Jung J, Cho BS, Kim HJ, et al. 2019; Reclassification of acute myeloid leukemia according to the 2016 WHO classification. Ann Lab Med. 39:311–6. DOI: 10.3343/alm.2019.39.3.311. PMID: 30623623. PMCID: PMC6340847.
Article14. Pui CH. 2000; Acute lymphoblastic leukemia in children. Curr Opin Oncol. 12:3–12. DOI: 10.1097/00001622-200001000-00002. PMID: 10687723.
Article15. Pullarkat V, Slovak ML, Kopecky KJ, Forman SJ, Appelbaum FR. 2008; Impact of cytogenetics on the outcome of adult acute lymphoblastic leukemia: results of Southwest Oncology Group 9400 study. Blood. 111:2563–72. DOI: 10.1182/blood-2007-10-116186. PMID: 18156492. PMCID: PMC2254550.
Article16. Amare P, Gladstone B, Varghese C, Pai S, Advani S. 1999; Clinical significance of cytogenetic findings at diagnosis and in remission in childhood and adult acute lymphoblastic leukemia: experience from India. Cancer Genet Cytogenet. 110:44–53. DOI: 10.1016/S0165-4608(98)00179-4. PMID: 10198622.17. Chang HH, Lu MY, Jou ST, Lin KH, Tien HF, Lin DT. 2006; Cytogenetics in childhood acute lymphoblastic leukemia in Taiwan: a single- institutional experience. Pediatr Hematol Oncol. 23:495–506. DOI: 10.1080/08880010600739368. PMID: 16849281.18. Pinheiro RF, Chauffaille Mde L, Silva MR. 2006; Isochromosome 17q in MDS: a marker of a distinct entity. Cancer Genet Cytogenet. 166:189–90. DOI: 10.1016/j.cancergencyto.2005.10.004. PMID: 16631479.
Article19. Kim MH, Hwang HY, Jeong SH, et al. 2000; Detection of p53 mutant and isochromosome 17q in myelodysplastic syndromes and leukemias. Korean J Clin Pathol. 20:349–53.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Review of Chromosomal Analyses Performed in a Single Hospital
- Spectra of Chromosomal Aberrations in 325 Leukemia Patients and Implications for the Development of New Molecular Detection Systems
- Two Concurrent Chromosomal Aberrations Involving Three-way t(3;21;8)(p21;q22;q22) and Two-way t(2;11)(q31;p15) Translocations in a Case of de novo Acute Myeloid Leukemia
- A case report of near-triploid in adult acute lymphocytic leukemia
- A Case of Acute Lymphoblastic Leukemia with Facial Nerve Palsy in Infant