J Korean Med Sci.
2020 Apr;35(13):e80. 10.3346/jkms.2020.35.e80.
Impact of Bronchiectasis on Postoperative Pulmonary Complications after Extra-Pulmonary Surgery in Patients with Airflow Limitation
- Affiliations
-
- 1Division of Pulmonology, Center of Lung Cancer, National Cancer Center, Goyang, Korea.
- 2Division of Pulmonology and Critical and Care Medicine, Department of Internal Medicine, Chungbuk National University Hospital, Chungbuk National University College of Medicine, Cheongju, Korea.
- 3Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Internal Medicine, Hallym University Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea.
- 4Division of Pulmonary Medicine and Allergy, Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea.
- 5Division of Pulmonary, Allergy and Critical Care Medicine, Department of Internal Medicine, Yonsei University Wonju Severance Christian Hospital, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 6Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2509609
- DOI: http://doi.org/10.3346/jkms.2020.35.e80
Abstract
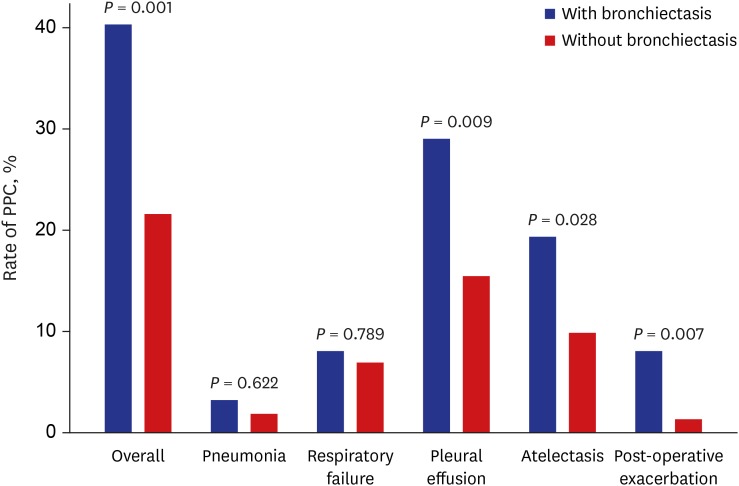
- The impact of bronchiectasis on the occurrence of postoperative pulmonary complications (PPC) after extra-pulmonary surgery in patients with airflow limitation is not well elucidated. A retrospective analysis of 437 patients with airflow limitations, including 62 patients with bronchiectasis, was conducted. The analysis revealed that bronchiectasis was associated with increased PPC (adjusted odds ratio [aOR], 2.73; P = 0.001), which was especially significant in patients who did not use bronchodilators (aOR, 3.24; P = 0.002). Our study indicates that bronchiectasis is associated with an increased risk of PPC following extra-pulmonary surgery in patients with airflow limitation, and bronchodilators may prevent PPC in these patients.
Keyword
Figure
Reference
-
1. Choi H, Yang B, Nam H, Kyoung DS, Sim YS, Park HY, et al. Population-based prevalence of bronchiectasis and associated comorbidities in South Korea. Eur Respir J. 2019; 54(2):1900194. PMID: 31048349.
Article2. Henkle E, Chan B, Curtis JR, Aksamit TR, Daley CL, Winthrop KL. Characteristics and health-care utilization history of patients with bronchiectasis in US medicare enrollees with prescription drug plans, 2006 to 2014. Chest. 2018; 154(6):1311–1320. PMID: 30055168.
Article3. Kang HR, Choi GS, Park SJ, Song YK, Kim JM, Ha J, et al. The effects of bronchiectasis on asthma exacerbation. Tuberc Respir Dis. 2014; 77(5):209–214.
Article4. Shin B, Lee H, Kang D, Jeong BH, Kang HK, Chon HR, et al. Airflow limitation severity and post-operative pulmonary complications following extra-pulmonary surgery in COPD patients. Respirology. 2017; 22(5):935–941. PMID: 28117553.
Article5. Smetana GW. Preoperative pulmonary evaluation. N Engl J Med. 1999; 340(12):937–944. PMID: 10089188.
Article6. Canet J, Gallart L, Gomar C, Paluzie G, Vallès J, Castillo J, et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology. 2010; 113(6):1338–1350. PMID: 21045639.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis and Management of Comorbidities Associated with Bronchiectasis
- Pathophysiology of Chronic Obstructive Pulmonary Disease
- Pathophysiology of Chronic Obstructive Pulmonary Disease
- Effect of Airflow Limitation on Acute Exacerbations in Patients with Destroyed Lungs by Tuberculosis
- Risk Factors for Unawareness of Obstructive Airflow Limitation among Adults with Chronic Obstructive Pulmonary Disease