J Korean Med Sci.
2020 Dec;35(48):e400. 10.3346/jkms.2020.35.e400.
Hypertension-Mediated Organ Damage and Long-term Cardiovascular Outcomes in Asian Hypertensive Patients without Prior Cardiovascular Disease
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Veterans Health Service Medical Center, Seoul, Korea
- KMID: 2509525
- DOI: http://doi.org/10.3346/jkms.2020.35.e400
Abstract
- Background
Hypertension-mediated organ damage (HMOD), comprising structural and functional changes in arteries or end organs, is a marker of cardiovascular (CV) disease. However, there are limited data on evaluation of risk of CV disease regarding HMOD, especially in Asians. We sought to investigate the association between CV events and HMOD, and we tried to determine the most important diagnostic marker among the component of HMOD for prevention of mortality and CV events in treated Korean hypertensive patients.
Methods
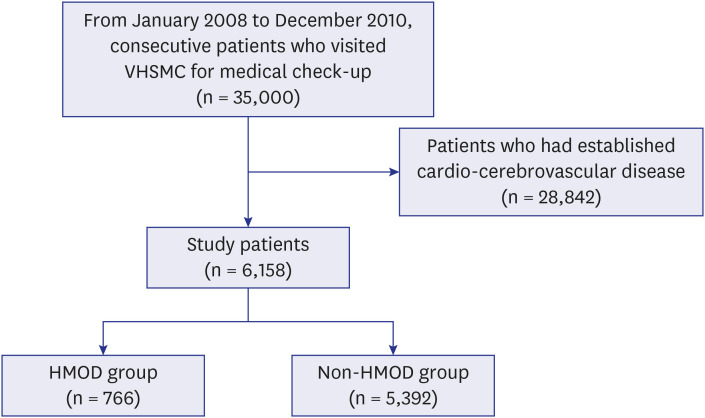
From January 2008 to December 2010, a total of 35,000 hypertensive Vietnamese War veterans who consecutively visited our hospital for medical check-up were reviewed, and 6,158 patients without established CV disease were enrolled. The patients were divided into two groups as follows: HMOD group (n = 766) and non-HMOD group (n = 5,392). The primary outcome was all-cause death.
Results
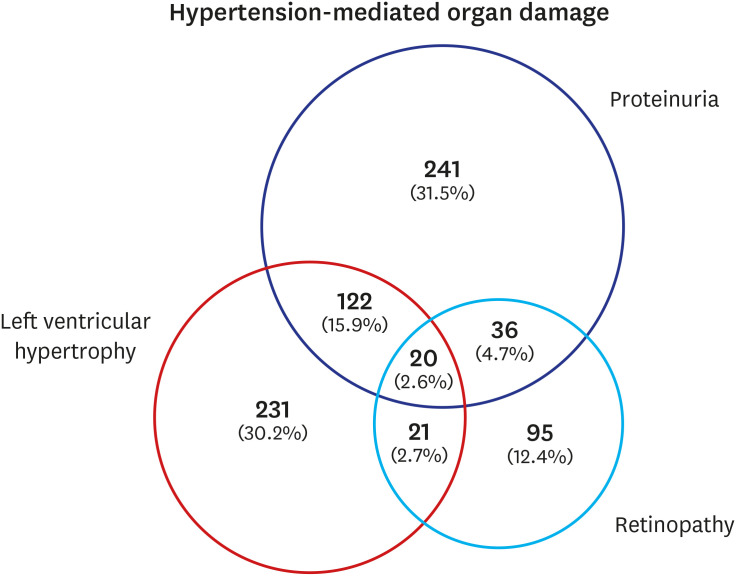
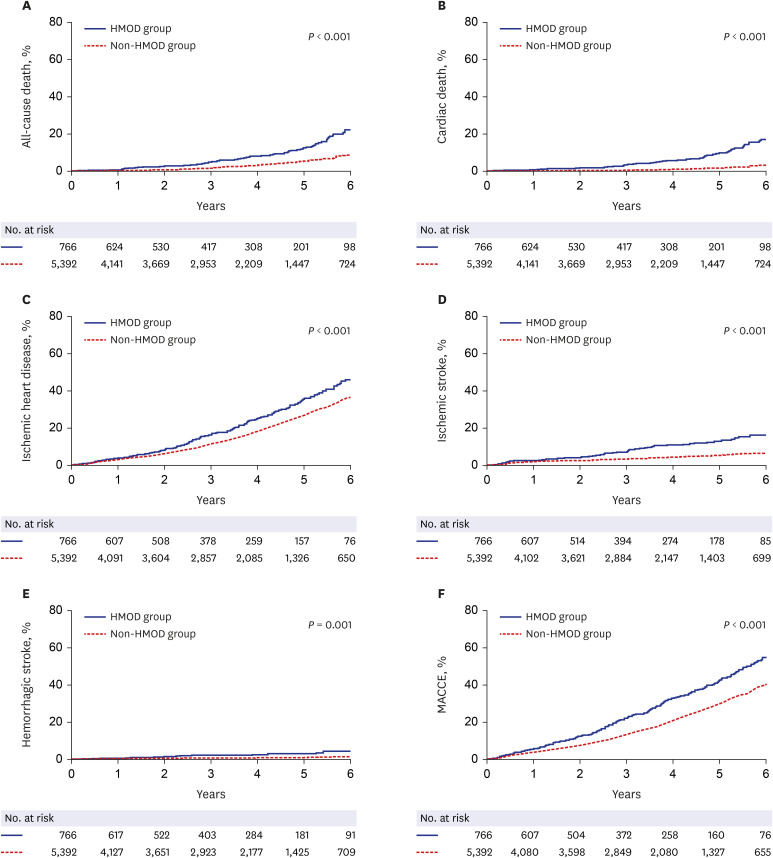
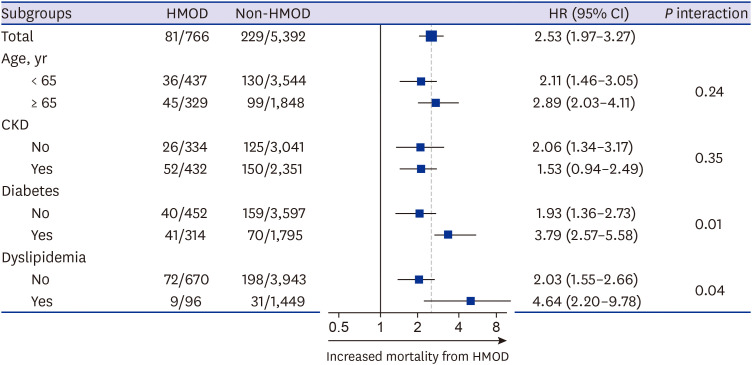
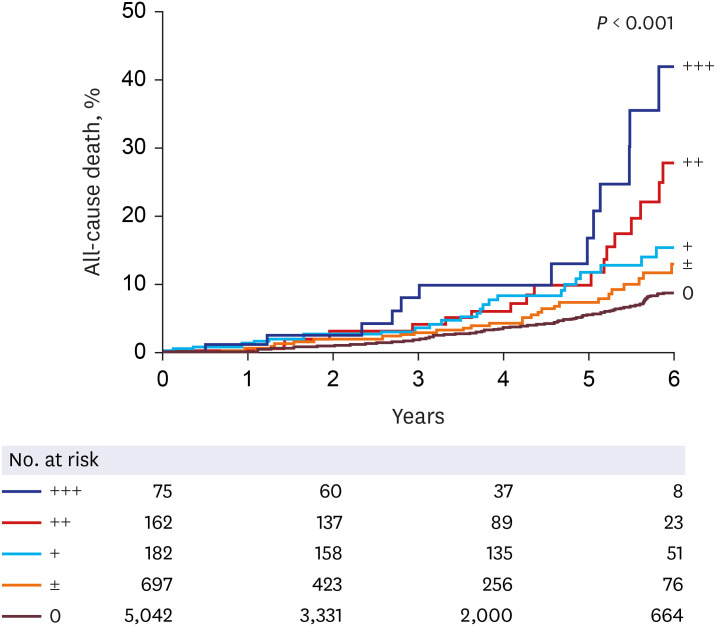
Median age was 63.3 years (interquartile range [IQR], 61.4–65.4), and median follow-up was 6.6 years (IQR, 5.9–7.2). Patients with old age, diabetes, and chronic kidney disease were more prevalent in the HMOD group than in the non-HMOD group (all P < 0.05).The lipid profiles were not significantly different between the two groups. Nephropathy was the most prevalent (54.7%) organ damage in the HMOD group. The 6-year incidence of all-cause death was higher in the HMOD group than in the non-HMOD group (22.5% vs.9.0%; adjusted hazard ratio [HR], 1.42; 95% confidence interval [CI], 1.01–2.00; P = 0.04). The incidence of cardiac death, ischemic heart disease, and ischemic and hemorrhagic stroke were also significantly higher in the HMOD group than in the non-HMOD group (P < 0.05, respectively). In multivariate analysis, proteinuria (adjusted HR, 2.21; 95% CI, 1.52–3.20; P < 0.001) was the most powerful independent risk factor to predict all-cause death among components of HMOD. As the degree of proteinuria increased, the rate of all-cause death also increased (long-rank P < 0.001).
Conclusion
HMOD was associated with increased risk of mortality and CV events. Proteinuria was the most powerful independent risk factor for all-cause death, and the degree of proteinuria and mortality rate were proportional. Our data suggest that monitoring of the proteinuria is important to predict long-term CV events in hypertensive patients.
Keyword
Figure
Reference
-
1. Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012; 380(9859):2224–2260. PMID: 23245609.2. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet. 2017; 389(10064):37–55. PMID: 27863813.3. Chow CK, Teo KK, Rangarajan S, Islam S, Gupta R, Avezum A, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013; 310(9):959–968. PMID: 24002282.
Article4. Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990–2015. JAMA. 2017; 317(2):165–182. PMID: 28097354.5. Mancia G, Facchetti R, Bombelli M, Polo Friz H, Grassi G, Giannattasio C, et al. Relationship of office, home, and ambulatory blood pressure to blood glucose and lipid variables in the PAMELA population. Hypertension. 2005; 45(6):1072–1077. PMID: 15867138.
Article6. Goff DC Jr, Lloyd-Jones DM, Bennett G, Coady S, D'Agostino RB, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation. 2014; 129(25):Suppl 2. S49–S73. PMID: 24222018.7. Pontremoli R, Ravera M, Bezante GP, Viazzi F, Nicolella C, Berruti V, et al. Left ventricular geometry and function in patients with essential hypertension and microalbuminuria. J Hypertens. 1999; 17(7):993–1000. PMID: 10419073.
Article8. Roman MJ, Pickering TG, Schwartz JE, Pini R, Devereux RB. Association of carotid atherosclerosis and left ventricular hypertrophy. J Am Coll Cardiol. 1995; 25(1):83–90. PMID: 7798531.
Article9. Greve SV, Blicher MK, Sehestedt T, Gram-Kampmann EM, Rasmussen S, Vishram JK, et al. Effective risk stratification in patients with moderate cardiovascular risk using albuminuria and atherosclerotic plaques in the carotid arteries. J Hypertens. 2015; 33(8):1563–1570. PMID: 26103123.
Article10. Cuspidi C, Valerio C, Sala C, Esposito A, Masaidi M, Negri F, et al. Prevalence and correlates of multiple organ damage in a never-treated hypertensive population: role of ambulatory blood pressure. Blood Press Monit. 2008; 13(1):7–13. PMID: 18199918.
Article11. Devereux RB, Alderman MH. Role of preclinical cardiovascular disease in the evolution from risk factor exposure to development of morbid events. Circulation. 1993; 88(4 Pt 1):1444–1455. PMID: 8403291.
Article12. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018; 39(33):3021–3104. PMID: 30165516.
Article13. Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, et al. 2016 European guidelines on cardiovascular disease prevention in clinical practice: the sixth joint task force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of 10 societies and by invited experts)developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016; 37(29):2315–2381. PMID: 27222591.14. Peake M, Whiting M. Measurement of serum creatinine--current status and future goals. Clin Biochem Rev. 2006; 27(4):173–184. PMID: 17581641.15. Chapter 1: definition and classification of CKD. Kidney Int Suppl (2011). 2013; 3(1):19–62. PMID: 25018975.16. Levey AS, Coresh J, Greene T, Stevens LA, Zhang YL, Hendriksen S, et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006; 145(4):247–254. PMID: 16908915.
Article17. Surawicz B, Childers R, Deal BJ, Gettes LS, Bailey JJ, Gorgels A, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part III: intraventricular conduction disturbances: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society: endorsed by the International Society for Computerized Electrocardiology. Circulation. 2009; 119(10):e235–e240. PMID: 19228822.
Article18. Reibis RK, Huber M, Karoff M, Kamke W, Kreutz R, Wegscheider K, et al. Target organ damage and control of cardiovascular risk factors in hypertensive patients. Evidence from the multicenter ESTher registry. Herz. 2015; 40(Suppl 2):209–216. PMID: 25630386.19. de Simone G, Izzo R, Chinali M, De Marco M, Casalnuovo G, Rozza F, et al. Does information on systolic and diastolic function improve prediction of a cardiovascular event by left ventricular hypertrophy in arterial hypertension? Hypertension. 2010; 56(1):99–104. PMID: 20497990.
Article20. Bakris GL, Williams M, Dworkin L, Elliott WJ, Epstein M, Toto R, et al. Preserving renal function in adults with hypertension and diabetes: a consensus approach. National Kidney Foundation Hypertension and Diabetes Executive Committees Working Group. Am J Kidney Dis. 2000; 36(3):646–661. PMID: 10977801.21. Ljungman S, Wikstrand J, Hartford M, Berglund G. Urinary albumin excretion--a predictor of risk of cardiovascular disease. A prospective 10-year follow-up of middle-aged nondiabetic normal and hypertensive men. Am J Hypertens. 1996; 9(8):770–778. PMID: 8862223.22. Agewall S, Wikstrand J, Ljungman S, Fagerberg B. Usefulness of microalbuminuria in predicting cardiovascular mortality in treated hypertensive men with and without diabetes mellitus. Risk Factor Intervention Study Group. Am J Cardiol. 1997; 80(2):164–169. PMID: 9230153.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hypertensive Retinopathy and Associated Target Organ Damage in Korean Hypertensive Patients
- Carotid artery intima-media thickness and hypertensive heart disease: a short review
- Arterial stiffness and hypertension
- Anesthetic management of hypertensive patients
- Influence of Metabolic Syndrome on Hypertension-related Target Organ Damage: Diagnosis of Metabolic Syndrome Is Still Necessary