J Korean Soc Hypertens.
2011 Sep;17(3):125-132. 10.5646/jksh.2011.17.3.125.
Influence of Metabolic Syndrome on Hypertension-related Target Organ Damage: Diagnosis of Metabolic Syndrome Is Still Necessary
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea. hylee612@snu.ac.kr
- 2Korean Society of Hypertension, Working Group on Metabolic Syndrome, Seoul, Korea.
- KMID: 1750394
- DOI: http://doi.org/10.5646/jksh.2011.17.3.125
Abstract
- BACKGROUND
The value of metabolic syndrome (MetS) evaluation in predicting cardiovascular disease is recently criticized. We investigated, in hypertensive patients without diabetes mellitus, the influence of MetS on the target organ damage.
METHODS
Data from the fourth Korean National Health and Nutrition Examination Survey performed in 2008 were analyzed. Metabolic syndrome is defined by the 2001 National Cholesterol Education Program-Third Adult Treatment Panel guideline. The category of hypertension is defined following the seventh report of the Joint National Commitee-7 guideline.
RESULTS
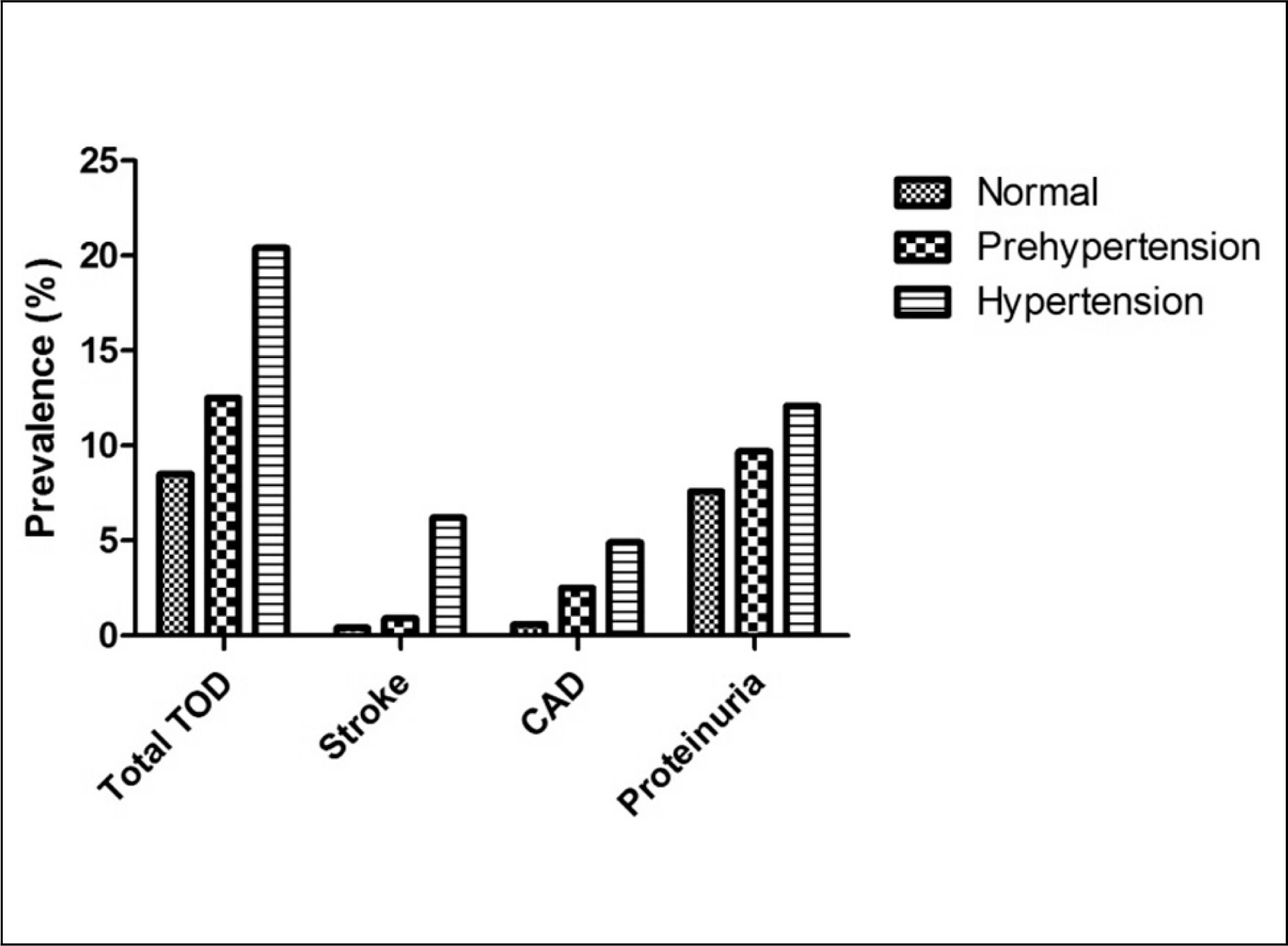
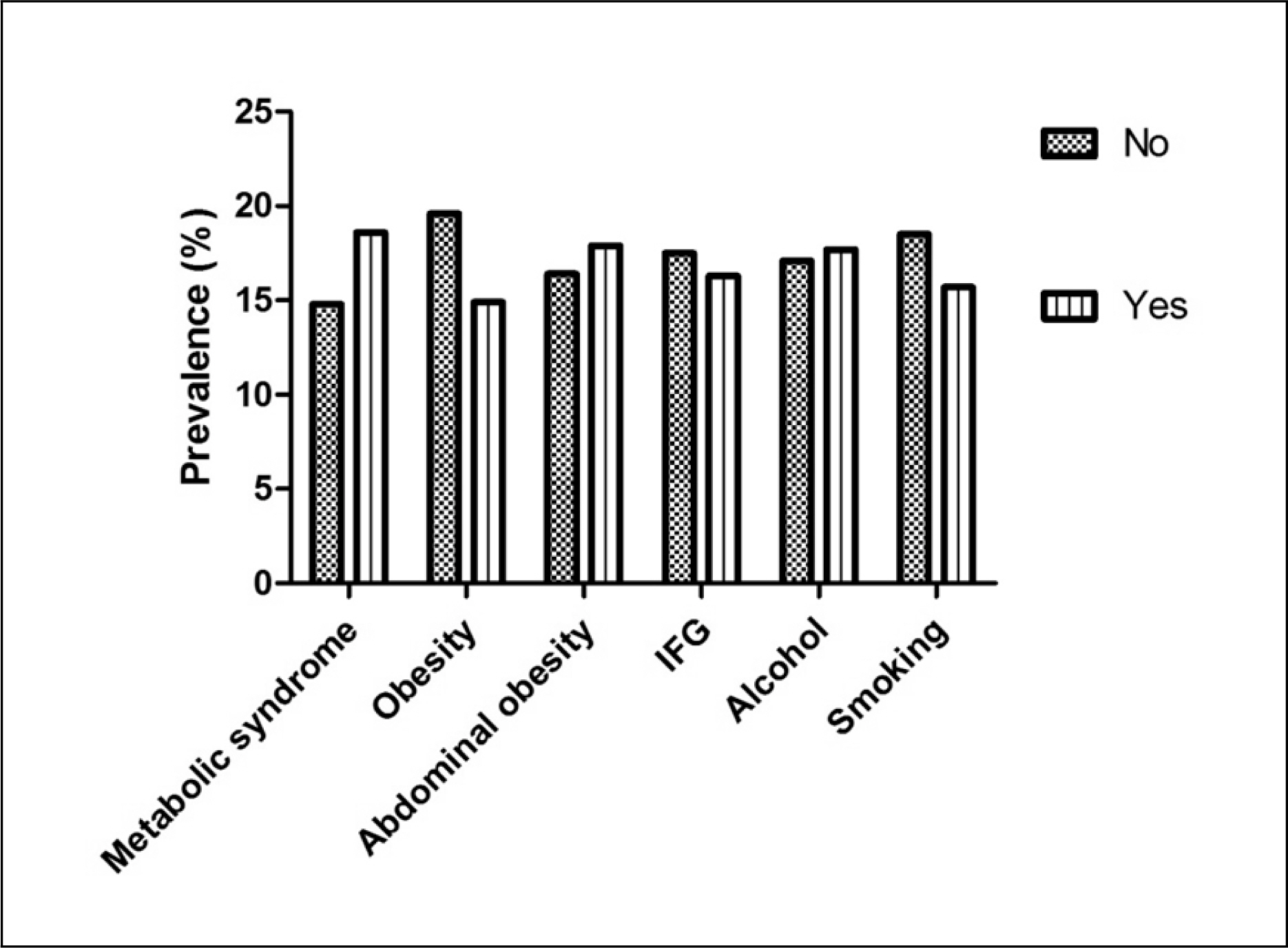
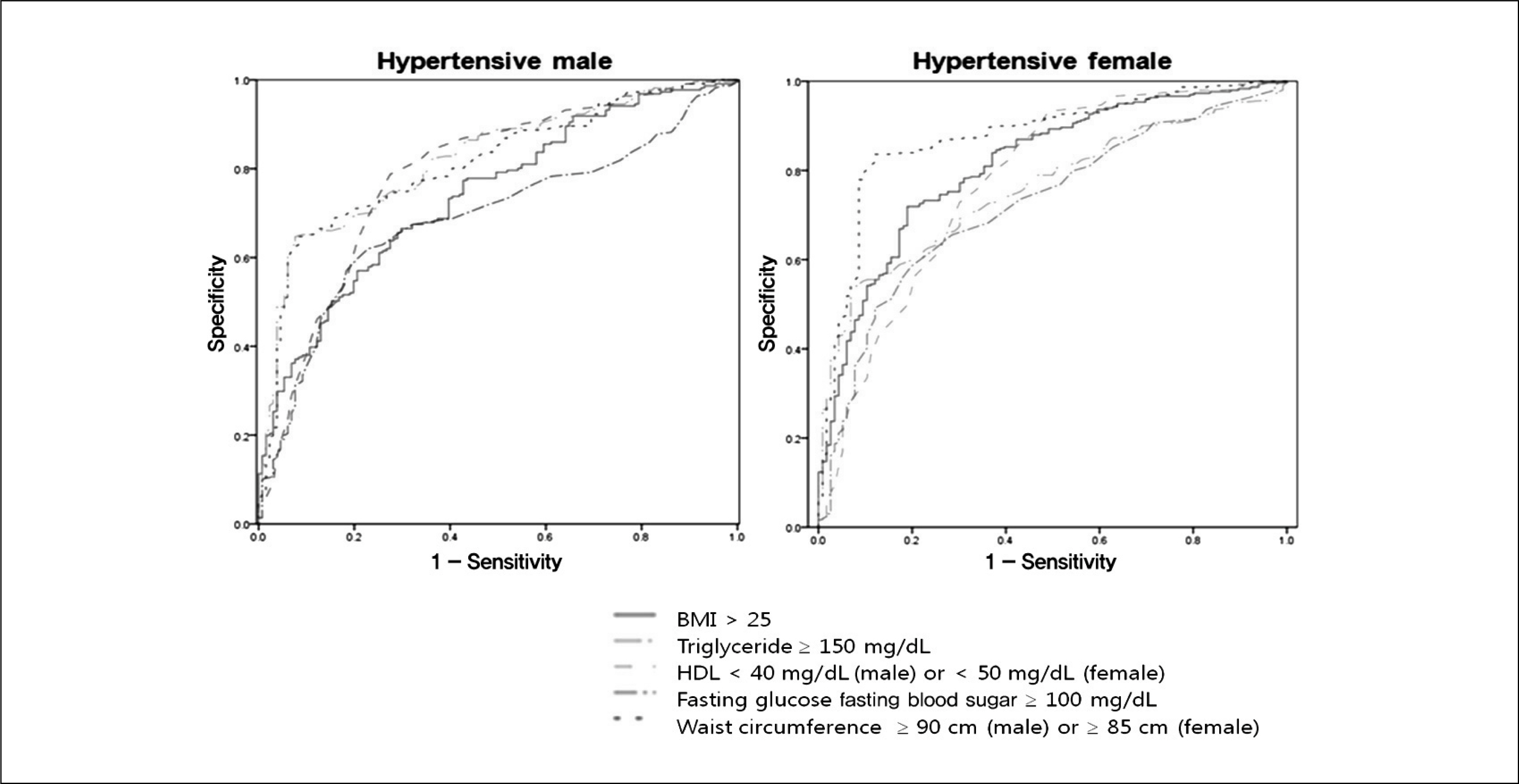
The prevalence of target organ damage (TOD), defined as history of myocardial infarction/angina/stroke/chronic renal disease as well as the presence of macroalbuminuria, was increased according to blood pressure; 8.5% in the population of normal blood pressure, 12.5% in those of prehypertensive range, and 20.5% in hypertensive population. Hypertensive population associated with MetS showed greater prevalence of TOD than those without MetS even excluding diabetic population. The presence of MetS in hypertensive population showed 2.2 fold increased risk for TOD. Any single parameter of MetS diagnostic criteria as well as obesity did not show the comparable range of risk prediction as MetS.
CONCLUSIONS
These results indicate a strong relationship of Mets with TOD in hypertensive population. Evaluating the metabolic components in hypertensive population is necessary in establishing management strategies for overall risk.
MeSH Terms
Figure
Reference
-
References
1. Park YW, Zhu S, Palaniappan L, Heshka S, Carnethon MR, Heymsfield SB. The metabolic syndrome: prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey 1988-1994. Arch Intern Med. 2003; 163:427–36.2. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults . Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001; 285:2486–97.3. Lee SY, Park HS, Kim DJ, Han JH, Kim SM, Cho GJ, et al. Appropriate waist circumference cutoff points for central obesity in Korean adults. Diabetes Res Clin Pract. 2007; 75:72–80.
Article4. Cha MJ, Lee HY, Ahn SV, Han KR, Park JB, Lim SJ, et al. Prevalence and clinical characteristics of metabolic syndrome in Korean hypertensive patients. Korean Hypertens J. 2009; 15:37–44.5. Kim TH, Kim DJ, Lim S, Jeong IK, Son HS, Chung CH, et al. Clinical characteristics according to the presence of the metabolic syndrome in type 2 diabetic patients with hypertension. Korean Hypertens J. 2009; 15:36–42.6. Cuspidi C, Meani S, Valerio C, Sala C, Fusi V, Zanchetti A, et al. Age and target organ damage in essential hypertension: role of the metabolic syndrome. Am J Hypertens. 2007; 20:296–303.
Article7. Schillaci G, Pirro M, Vaudo G, Gemelli F, Marchesi S, Porcellati C, et al. Prognostic value of the metabolic syndrome in essential hypertension. J Am Coll Cardiol. 2004; 43:1817–22.
Article8. Reaven GM. The metabolic syndrome: is this diagnosis necessary? Am J Clin Nutr. 2006; 83:1237–47.
Article9. Reaven GM. The metabolic syndrome: time to get off the merry-go-round? J Intern Med. 2011; 269:127–36.
Article10. Kanazawa M, Yoshiike N, Osaka T, Numba Y, Zimmet P, Inoue S. Criteria and classification of obesity in Japan and Asia-Oceania. Asia Pac J Clin Nutr. 2002; 11(Suppl 8):S732–7.
Article11. Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, et al. 2007 Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2007; 25:1105–87.12. Pontremoli R, Cheli V, Sofia A, Tirotta A, Ravera M, Nicolella C, et al. Prevalence of micro- and macroalbuminuria and their relationship with other cardiovascular risk factors in essential hypertension. Nephrol Dial Transplant. 1995; 10(Suppl 6):6–9.
Article13. Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 1983; 148:839–43.
Article14. Mule G, Nardi E, Cottone S, Cusimano P, Volpe V, Piazza G, et al. Influence of metabolic syndrome on hypertension-related target organ damage. J Intern Med. 2005; 257:503–13.
Article15. Leoncini G, Ratto E, Viazzi F, Vaccaro V, Parodi D, Parodi A, et al. Metabolic syndrome is associated with early signs of organ damage in nondiabetic, hypertensive patients. J Intern Med. 2005; 257:454–60.
Article16. Lind L, Andersson PE, Andren B, Hanni A, Lithell HO. Left ventricular hypertrophy in hypertension is associated with the insulin resistance metabolic syndrome. J Hypertens. 1995; 13:433–8.
Article17. Kahn R, Buse J, Ferrannini E. Stern M; American Diabetes Association; European Association for the Study of Diabetes. The metabolic syndrome: time for a critical appraisal: joint statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2005; 28:2289–304.18. Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2005; 365:1415–28.
Article19. Ferrannini E, Buzzigoli G, Bonadonna R, Giorico MA, Oleggini M, Graziadei L, et al. Insulin resistance in essential hypertension. N Engl J Med. 1987; 317:350–7.
Article20. Wang TD, Goto S, Bhatt DL, Steg PG, Chan JC, Richard AJ, et al. Ethnic differences in the relationships of anthropometric measures to metabolic risk factors in Asian patients at risk of atherothrombosis: results from the REduction of Atherothrombosis for Continued Health (REACH) Registry. Metabolism. 2010; 59:400–8.21. Obesity in Asia Collaboration. Is central obesity a better discriminator of the risk of hypertension than body mass index in ethnically diverse populations? J Hypertens. 2008; 26:169–77.22. Athyros VG, Ganotakis ES, Tziomalos K, Papageorgiou AA, Anagnostis P, Griva T, et al. Comparison of four definitions of the metabolic syndrome in a Greek (Mediterranean) population. Curr Med Res Opin. 2010; 26:713–9.
Article23. Ninomiya JK, L’Italien G, Criqui MH, Whyte JL, Gamst A, Chen RS. Association of the metabolic syndrome with history of myocardial infarction and stroke in the Third National Health and Nutrition Examination Survey. Circulation. 2004; 109:42–6.
Article