Pediatric liver transplantation with hyperreduced left lateral segment graft
- Affiliations
-
- 1Departments of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Departments of Pediatrics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2508860
- DOI: http://doi.org/10.14701/ahbps.2020.24.4.503
Abstract
- Backgrounds/Aims
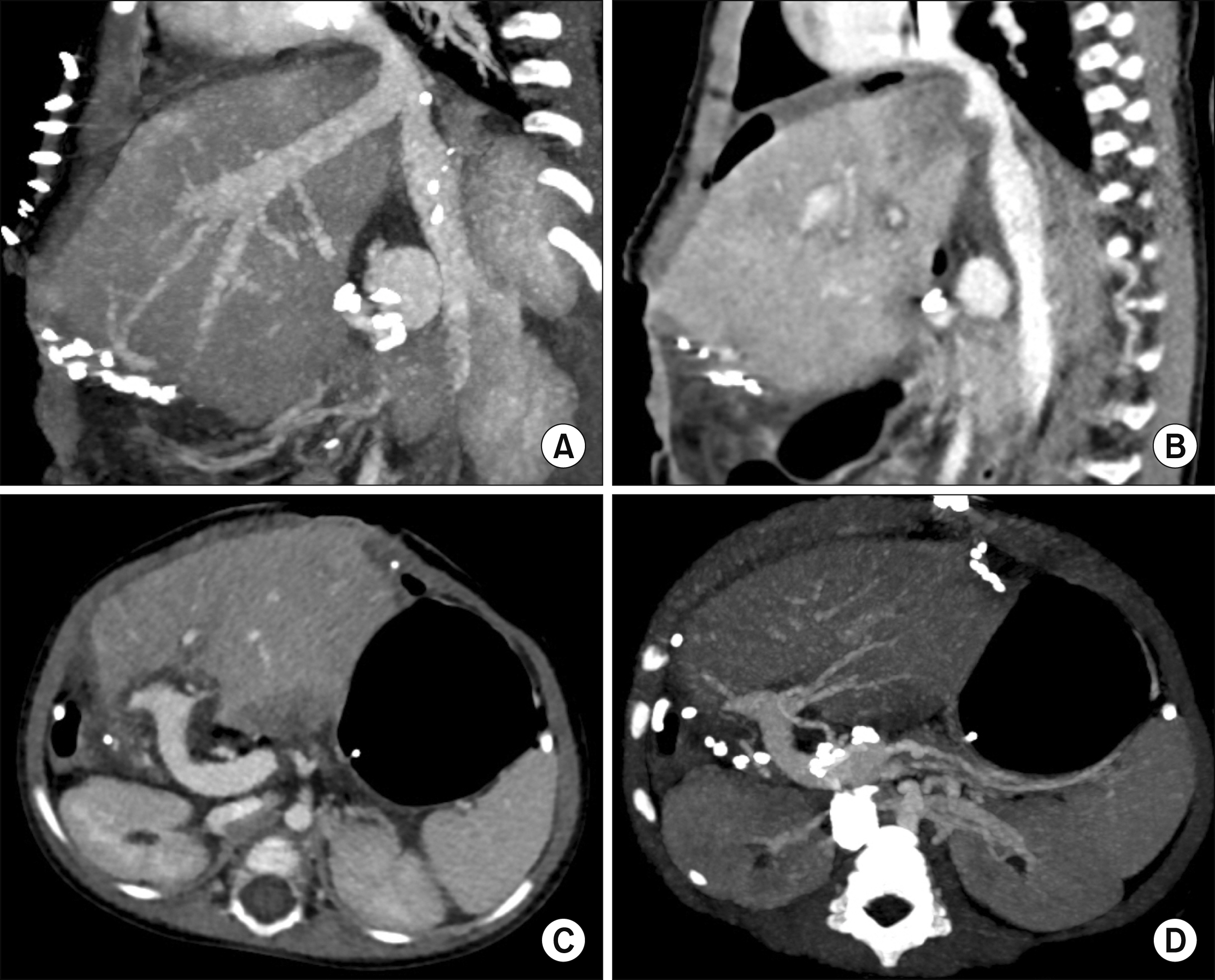
To prevent large-for-size graft-related complications in small infant patients, the size of a left lateral segment (LLS) graft can be reduced to be a hyperreduced LLS (HRLLS) graft.
Methods
This study was intended to describe the detailed techniques for harvesting and implanting HRLLS grafts developed in a high-volume liver transplantation (LT) center.
Results
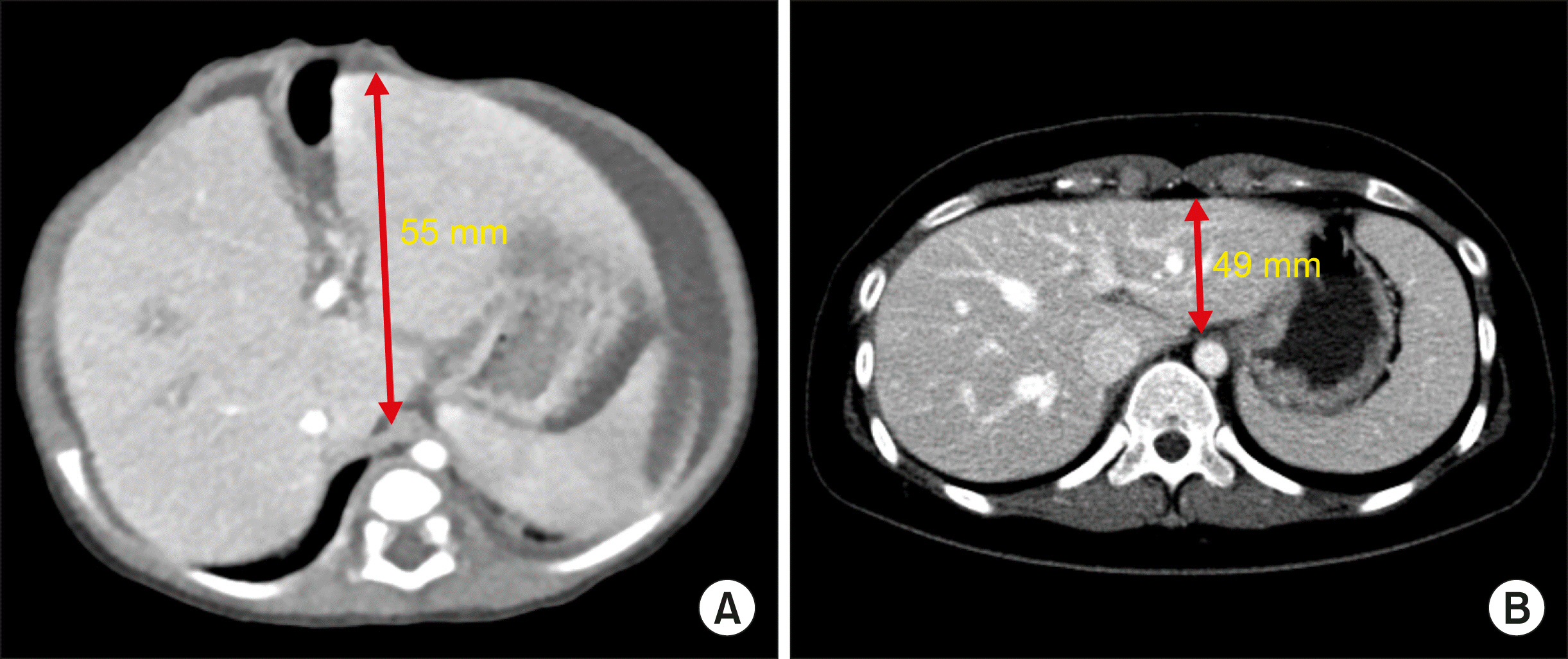
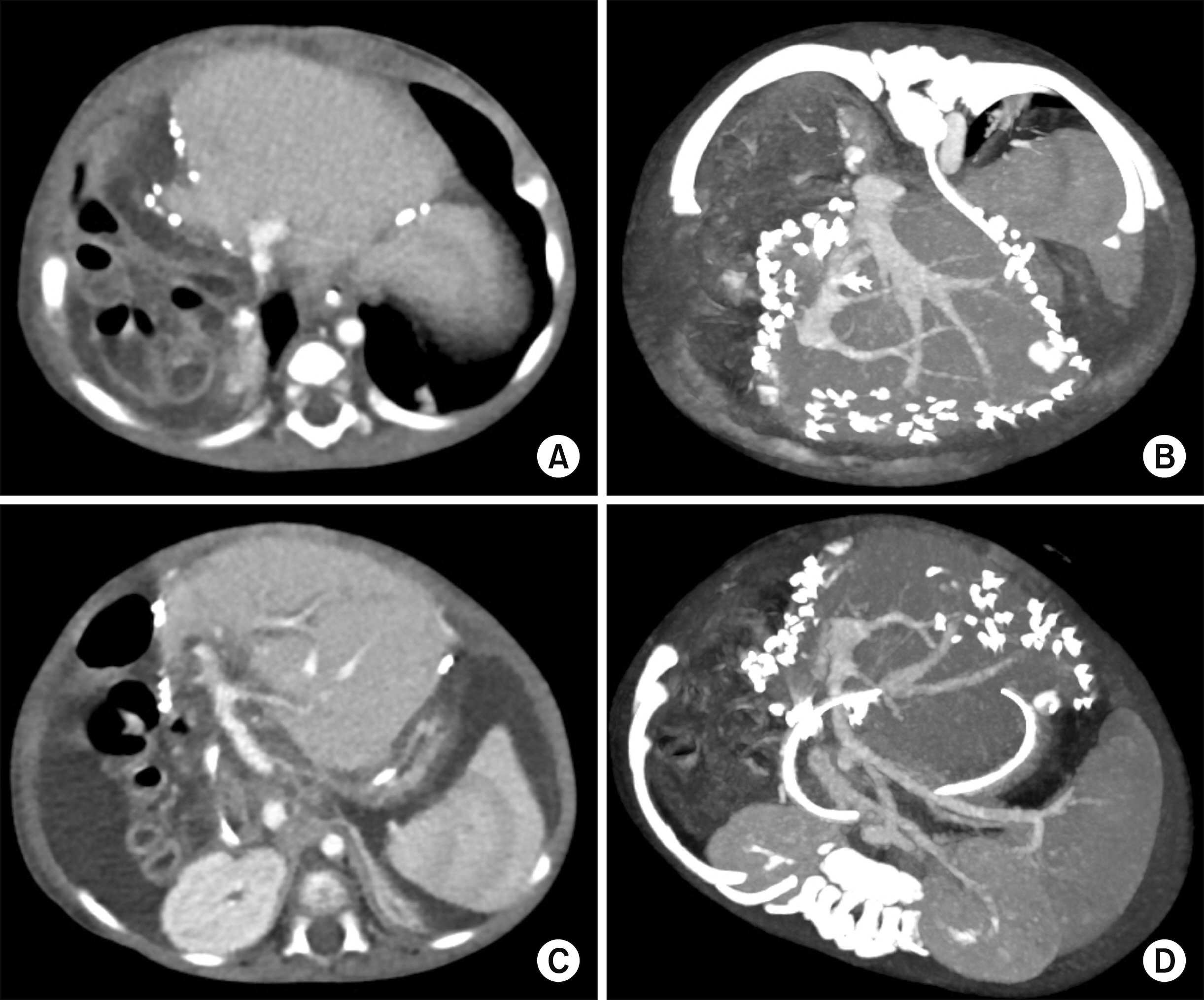
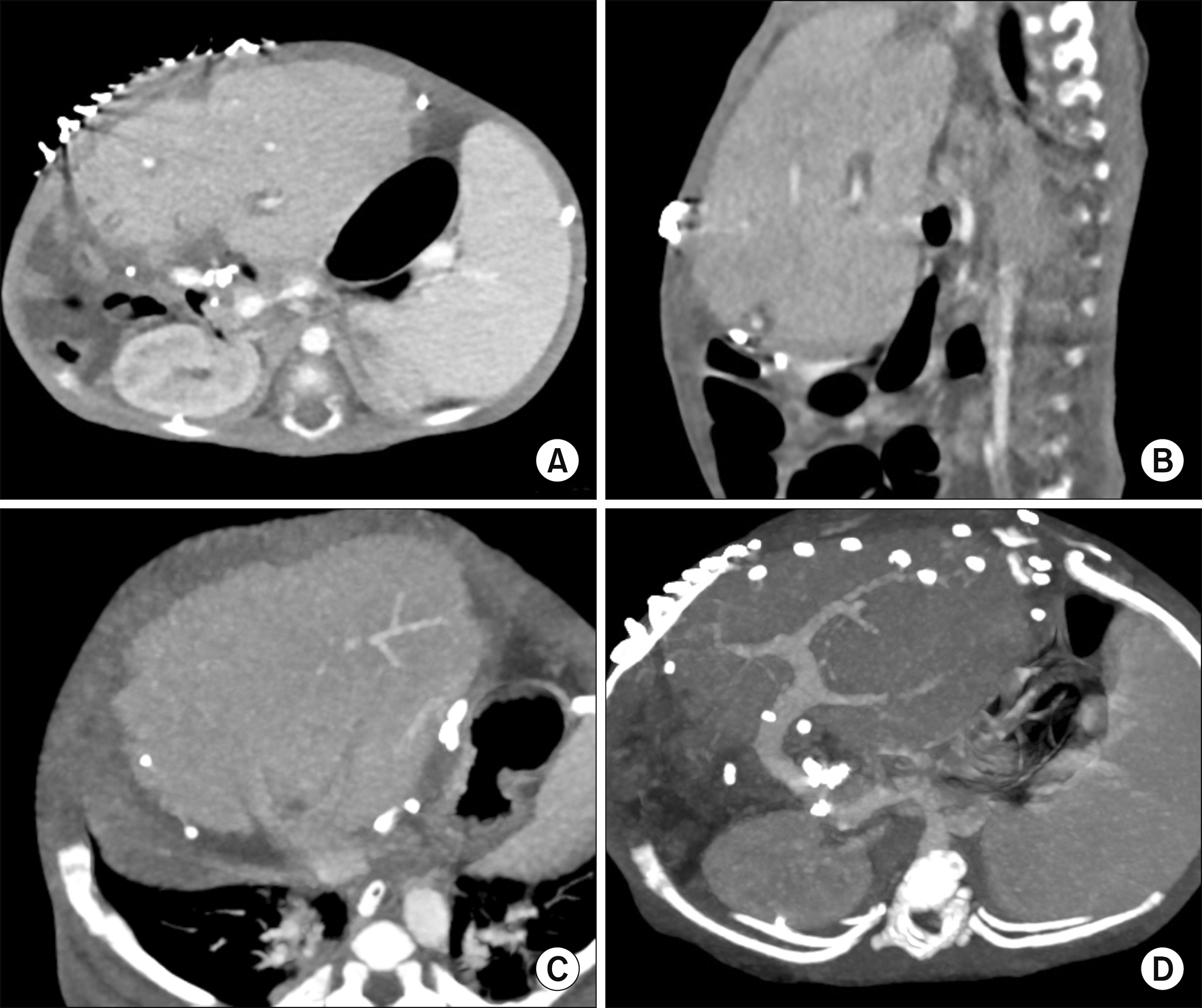
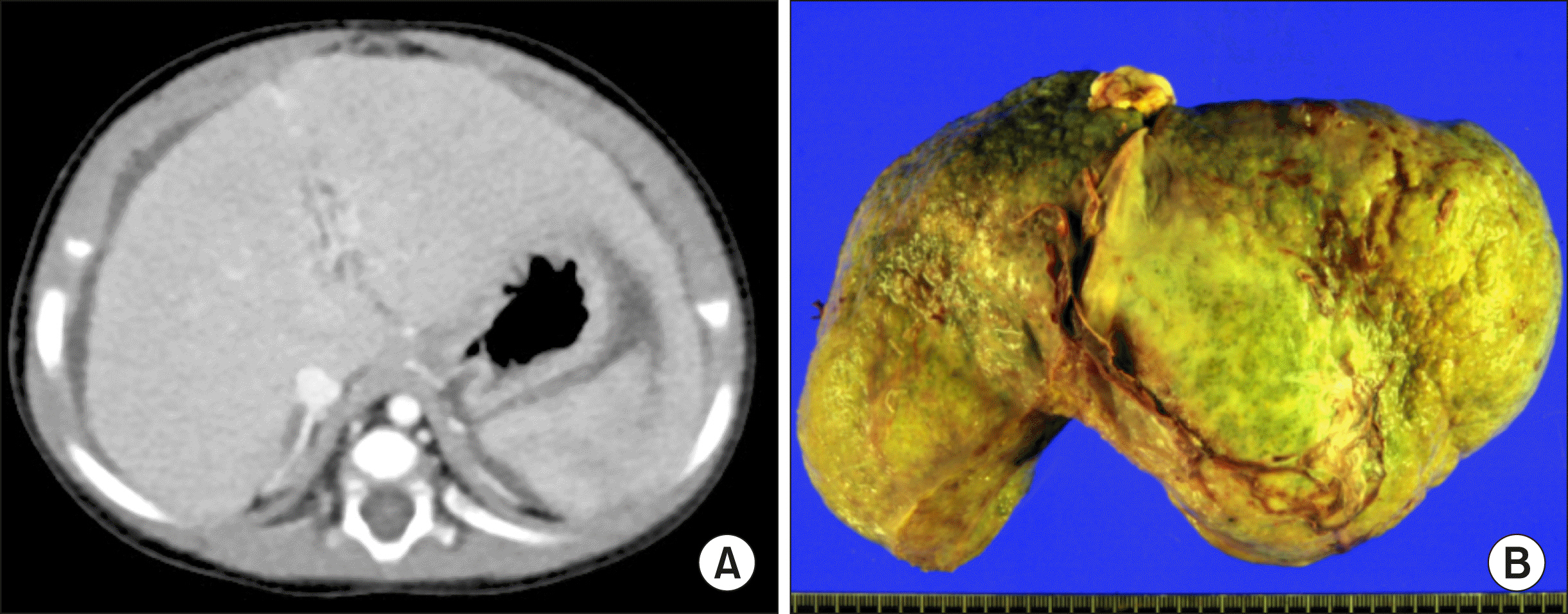
The mean recipient age was 4.0±1.7 months (range: 3-6) and body weight was 5.3±1.4 kg (range: 4.1-6.9). Primary diagnoses of the recipients were progressive familial intrahepatic cholestasis in 2 and biliary atresia in 1. The types of LT were living donor LT in 1 and split deceased donor LT in 2. Non-anatomical size reduction was performed to the transected LLS grafts. The mean weight of the HRLLS grafts was 191.7±62.1 g (range: 120-230) and graft-recipient weight ratio was 3.75±1.57% (range: 2.45-5.49). Widening venoplasty was applied to the graft left hepatic vein outflow orifice. Vein homograft interposition was used in a case with portal vein hypoplasia. Types of the abdomen wound closure were one case of primary repair, one of two-staged closure with a mesh, and one of three-staged repair with a silo and a mesh. All three patients recovered uneventfully from the LT operation and are doing well to date for more than 6 years after transplantation.
Conclusions
Making a HRLLS graft through non-anatomical resection during living donor LT and split deceased donor LT can be a useful option for treating small infant patients.
Keyword
Figure
Cited by 4 articles
-
Third retransplantation using a whole liver graft for late graft failure from hepatic vein stent stenosis in a pediatric patient who underwent split liver retransplantation
Jung-Man Namgoong, Shin Hwang, Young-In Yoon, Yong-Pil Cho, Woo-Hyoung Kang, Yong Jae Kwon, Hyunhee Kwon, Sang Hoon Kim, Kyung Mo Kim, Seak Hee Oh
Ann Hepatobiliary Pancreat Surg. 2021;25(2):299-306. doi: 10.14701/ahbps.2021.25.2.299.Dextroplantation of a reduced left lateral section graft in an infant undergoing living donor liver transplantation
Jung-Man Namgoong, Shin Hwang, Gil-Chun Park, Kyung Mo Kim, Seak Hee Oh, Hyunhee Kwon, Yong Jae Kwon
Ann Hepatobiliary Pancreat Surg. 2021;25(3):414-418. doi: 10.14701/ahbps.2021.25.3.414.Liver transplantation in pediatric patients with progressive familial intrahepatic cholestasis: Single center experience of seven cases
Jung-Man Namgoong, Shin Hwang, Hyunhee Kwon, Suhyeon Ha, Kyung Mo Kim, Seak Hee Oh, Seung-Mo Hong
Ann Hepatobiliary Pancreat Surg. 2022;26(1):69-75. doi: 10.14701/ahbps.21-114.Living donor liver transplantation with hyperreduced segment II monosegment graft for an infant weighing 3 kilograms
Jung-Man Namgoong, Gil-Chun Park, Shin Hwang, Sang-Hoon Kim, Suhyeon Ha, Kyung Mo Kim, Seak Hee Oh
Ann Liver Transplant. 2023;3(1):50-56. doi: 10.52604/alt.23.0001.
Reference
-
1. Kanazawa H, Sakamoto S, Fukuda A, Uchida H, Hamano I, Shigeta T, et al. 2013; Living-donor liver transplantation with hyperreduced left lateral segment grafts: a single-center experience. Transplantation. 95:750–754. DOI: 10.1097/TP.0b013e31827a93b4. PMID: 23503505.2. Shehata MR, Yagi S, Okamura Y, Iida T, Hori T, Yoshizawa A, et al. 2012; Pediatric liver transplantation using reduced and hyper-reduced left lateral segment grafts: a 10-year single-center experience. Am J Transplant. 12:3406–3413. DOI: 10.1111/j.1600-6143.2012.04268.x. PMID: 22994696.
Article3. Ardiles V, Ciardullo MA, D'Agostino D, Pekolj J, Mattera FJ, Boldrini GH, et al. 2013; Transplantation with hyper-reduced liver grafts in children under 10 kg of weight. Langenbecks Arch Surg. 398:79–85. DOI: 10.1007/s00423-012-1020-y. PMID: 23093088.4. Thomas N, Thomas G, Verran D, Stormon M, O'Loughlin E, Shun A. 2010; Liver transplantation in children with hyper-reduced grafts - a single-center experience. Pediatr Transplant. 14:426–430. DOI: 10.1111/j.1399-3046.2010.01294.x. PMID: 20214746.
Article5. Yamada N, Sanada Y, Hirata Y, Okada N, Wakiya T, Ihara Y, et al. 2015; Selection of living donor liver grafts for patients weighing 6kg or less. Liver Transpl. 21:233–238. DOI: 10.1002/lt.24048. PMID: 25422258.
Article6. Sakuma Y, Sasanuma H, Miki A, Shimizu A, Sata N, Yasuda Y, et al. 2016; Living-donor liver transplantation using segment 2 monosegment graft: a single-center experience. Transplant Proc. 48:1110–1114. DOI: 10.1016/j.transproceed.2015.12.119. PMID: 27320568.
Article7. Hong SK, Suh KS, Kim HS, Yoon KC, Ahn SW, Kim H, et al. 2018; Pediatric living donor liver transplantation using a monosegment procured by Pure 3D laparoscopic left lateral sectionectomy and in situ reduction. J Gastrointest Surg. 22:1135–1136. DOI: 10.1007/s11605-018-3705-1. PMID: 29435902.
Article8. Srinivasan P, Vilca-Melendez H, Muiesan P, Prachalias A, Heaton ND, Rela M. 1999; Liver transplantation with monosegments. Surgery. 126:10–12. DOI: 10.1067/msy.1999.98686. PMID: 10418586.
Article9. Lee S, Lee SK. 2013; Pediatric liver transplantation. J Korean Assoc Pediatr Surg. 19:14–21. DOI: 10.13029/jkaps.2013.19.1.14. PMID: 28502445.
Article10. Sakamoto S, Kanazawa H, Shigeta T, Uchida H, Sasaki K, Hamano I, et al. 2014; Technical considerations of living donor hepatectomy of segment 2 grafts for infants. Surgery. 156:1232–1237. DOI: 10.1016/j.surg.2014.05.003. PMID: 24909347.
Article11. Hwang S, Kim DY, Ahn CS, Moon DB, Kim KM, Park GC, et al. 2013; Computational simulation-based vessel interposition reconstruction technique for portal vein hypoplasia in pediatric liver transplantation. Transplant Proc. 45:255–258. DOI: 10.1016/j.transproceed.2012.05.090. PMID: 23375311.
Article12. Kiuchi T, Kasahara M, Uryuhara K, Inomata Y, Uemoto S, Asonuma K, et al. 1999; Impact of graft size mismatching on graft prognosis in liver transplantation from living donors. Transplantation. 67:321–327. DOI: 10.1097/00007890-199901270-00024. PMID: 10075602.13. Kasahara M, Fukuda A, Yokoyama S, Sato S, Tanaka H, Kuroda T, et al. 2008; Living donor liver transplantation with hyperreduced left lateral segments. J Pediatr Surg. 43:1575–1578. DOI: 10.1016/j.jpedsurg.2008.02.056. PMID: 18675660.
Article14. Vanatta JM, Esquivel CO. 2007; Status of liver transplantation in infants < 5 kg. Pediatr Transplant. 11:5–9. DOI: 10.1111/j.1399-3046.2006.00627.x. PMID: 17328158.15. Raices M, Czerwonko ME, Ardiles V, Boldrini G, D'Agostino D, Marcó Del Pont J, et al. 2019; Short- and long-term outcomes after live-donor transplantation with hyper-reduced liver grafts in low-weight pediatric recipients. J Gastrointest Surg. 23:2411–2420. DOI: 10.1007/s11605-019-04188-y. PMID: 30887299.
Article16. Hwang S, Kim KH, Kim DY, Kim KM, Ahn CS, Moon DB, et al. 2013; Anomalous hepatic vein anatomy of left lateral section grafts and customized unification venoplasty for pediatric living donor liver transplantation. Liver Transpl. 19:184–190. DOI: 10.1002/lt.23557. PMID: 23045153.
Article17. Namgoong JM, Hwang S, Park GC, Kwon H, Kwon YJ, Kim SH. 2020; Graft outflow vein unification venoplasty with superficial left hepatic vein branch in pediatric living donor liver transplantation using a left lateral section graft. Ann Hepatobiliary Pancreat Surg. 24:326–332. DOI: 10.14701/ahbps.2020.24.3.326. PMID: 32843600. PMCID: PMC7452796.
Article18. Kidd JN Jr, Jackson RJ, Smith SD, Wagner CW. 2003; Evolution of staged versus primary closure of gastroschisis. Ann Surg. 237:759–764. discussion 764-765. DOI: 10.1097/01.SLA.0000071568.95915.DC. PMID: 12796571. PMCID: PMC1514688.
Article19. Kwon H, Kwon H, Hong JP, Han Y, Park H, Song GW, et al. 2015; Use of cryopreserved cadaveric arterial allograft as a vascular conduit for peripheral arterial graft infection. Ann Surg Treat Res. 89:51–54. DOI: 10.4174/astr.2015.89.1.51. PMID: 26131446. PMCID: PMC4481033.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pediatric split liver transplantation using a hyperreduced left lateral segment graft in an infant weighing 4 kg
- Living donor liver transplantation with hyperreduced segment II monosegment graft for an infant weighing 3 kilograms
- Left at right heterotopic implantation of left liver graft in adult-to-adult living donor liver transplantation: the technical concern for decision-making
- Pediatric liver transplantation with hyperreduced left lateral segment graft
- Tailored techniques of graft outflow vein reconstruction in pediatric liver transplantation at Asan Medical Center