Intest Res.
2020 Oct;18(4):447-458. 10.5217/ir.2019.00042.
An assessment of dietary intake, food avoidance and food beliefs in patients with ulcerative colitis of different disease status
- Affiliations
-
- 1Dietetic Unit & Centre of Healthy Ageing and Wellness, Faculty of Health Sciences, National University of Malaysia, Kuala Lumpur, Malaysia
- 2Department of Physiology, Faculty of Medicine, National University of Malaysia, Kuala Lumpur, Malaysia
- 3GUT Research Group, Faculty of Medicine, National University of Malaysia, Kuala Lumpur, Malaysia
- 4Gastroenterology Unit, Department of Medicine, UKM Medical Centre, Kuala Lumpur, Malaysia
- KMID: 2508577
- DOI: http://doi.org/10.5217/ir.2019.00042
Abstract
- Background/Aims
Ulcerative colitis (UC) is a chronic, relapsing and remitting inflammation of the gastrointestinal tract. Little is known about the link between dietary intake, food avoidance, and beliefs among UC patients of different disease severity. Therefore, this study aimed to assess the dietary intake, food avoidance, and beliefs among active and inactive UC patients.
Methods
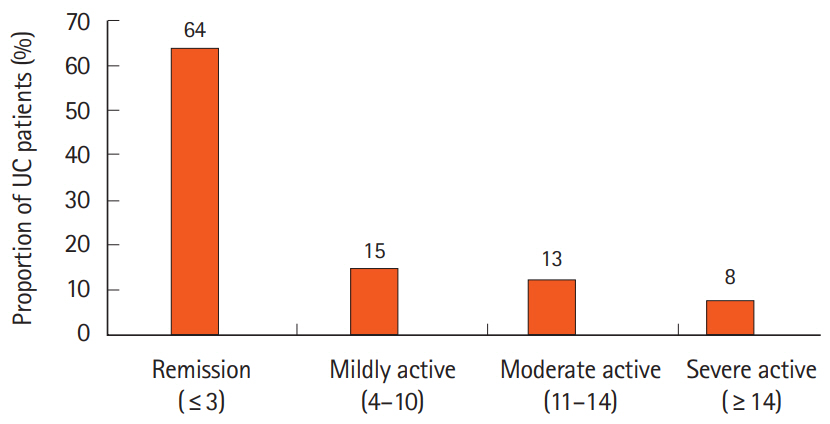
A cross-sectional study was conducted among UC patients from a tertiary medical center in Kuala Lumpur, Malaysia. Demographic, anthropometric, dietary intake, food avoidance and beliefs were assessed. Disease activity of UC patients was evaluated using the Powell Tuck Index.
Results
UC patients were recruited (64.1% inactive UC and 35.9% active UC). As compared to inactive UC patients, active UC patients were likely to lose weight (75.0% vs. 0%), possess certain food beliefs (95.7% vs. 39.0%), and frequently practiced dietary avoidance (95.7% vs. 43.9%). The dietary intake among inactive UC patients was higher than active UC patients. However, neither of them met the standard nutrients recommendation for protein, calcium, iron, folate, zinc, vitamin D, vitamin B12, and vitamin E.
Conclusions
Active UC patients had poorer dietary intake, were more prone to practicing food avoidance and exhibited certain food beliefs as compared to inactive UC patients. Both macro- and micronutrients intakes were inadequate regardless of patient’s disease status. These findings emphasized the importance for patients to be provided with the nutrition-related knowledge as part of strategies to avoid nutritional inadequacies.
Keyword
Figure
Cited by 1 articles
-
Evaluation of nutritional status using bioelectrical impedance analysis in patients with inflammatory bowel disease
Seung Hyuk Kim, You Sun Kim, Si Hyeong Lee, Hyun Mi Lee, Won Eui Yoon, Seo Hyun Kim, Hee Jun Myung, Jeong Seop Moon
Intest Res. 2022;20(3):321-328. doi: 10.5217/ir.2021.00022.
Reference
-
1. Goyal N, Rana A, Ahlawat A, Bijjem KR, Kumar P. Animal models of inflammatory bowel disease: a review. Inflammopharmacology. 2014; 22:219–233.
Article2. Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012; 142:46–54.
Article3. Ng WK, Wong SH, Ng SC. Changing epidemiological trends of inflammatory bowel disease in Asia. Intest Res. 2016; 14:111–119.
Article4. Jakubowski A, Zagórowicz E, Kraszewska E, Bartnik W. Rising hospitalization rates for inflammatory bowel disease in Poland. Pol Arch Med Wewn. 2014; 124:180–190.
Article5. Wędrychowicz A, Zając A, Tomasik P. Advances in nutritional therapy in inflammatory bowel diseases: review. World J Gastroenterol. 2016; 22:1045–1066.
Article6. Scaldaferri F, Pizzoferrato M, Lopetuso LR, et al. Nutrition and IBD: malnutrition and/or sarcopenia? A practical guide. Gastroenterol Res Pract. 2017; 2017:8646495.
Article7. Cohen AB, Lee D, Long MD, et al. Dietary patterns and self-reported associations of diet with symptoms of inflammatory bowel disease. Dig Dis Sci. 2013; 58:1322–1328.
Article8. Vagianos K, Clara I, Carr R, et al. What are adults with inflammatory bowel disease (IBD) eating? A closer look at the dietary habits of a population-based Canadian IBD cohort. JPEN J Parenter Enteral Nutr. 2016; 40:405–411.
Article9. O’Sullivan M. Vitamin D as a novel therapy in inflammatory bowel disease: new hope or false dawn? Proc Nutr Soc. 2015; 74:5–12.
Article10. Guagnozzi D, Lucendo AJ. Anemia in inflammatory bowel disease: a neglected issue with relevant effects. World J Gastroenterol. 2014; 20:3542–3551.
Article11. Silva AF, Schieferdecker ME, Amarante S. Food intake in patients with inflammatory bowel disease. ABCD Arq Bras Cir Dig. 2011; 24:204–209.12. Brasil Lopes M, Rocha R, Castro Lyra A, et al. Restriction of dairy products; a reality in inflammatory bowel disease patients. Nutr Hosp. 2014; 29:575–581.13. Lomer MC, Hart AL, Verjee A, Daly A, Solomon J, Mclaughlin J. What are the dietary treatment research priorities for inflammatory bowel disease? A short report based on a priority setting partnership with the James Lind Alliance. J Hum Nutr Diet. 2017; 30:709–713.
Article14. Walton M, Alaunyte I. Do patients living with ulcerative colitis adhere to healthy eating guidelines? A cross-sectional study. Br J Nutr. 2014; 112:1628–1635.
Article15. Limdi JK, Aggarwal D, McLaughlin JT. Dietary practices and beliefs in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2016; 22:164–170.
Article16. de Vries JHM, Dijkhuizen M, Tap P, Witteman BJM. Patient’s dietary beliefs and behaviours in inflammatory bowel disease. Dig Dis. 2019; 37:131–139.
Article17. Tomar SK, Kedia S, Upadhyay AD, et al. Impact of dietary beliefs and practices on patients with inflammatory bowel disease: an observational study from India. JGH Open. 2017; 1:15–21.
Article18. Krejcie RV, Morgan DW. Determining sample size for research activities. Educ Psychol Meas. 1970; 30:607–610.19. Shahar S, Earland J, Abdulrahman S. Validation of a dietary history questionnaire against a 7-D weighed record for estimating nutrient intake among rural elderly Malays. Malays J Nutr. 2000; 6:33–44.20. Bingham SA, Nelson M, Paul AA, Haraldsdottir J, Loken EB, Van Staveren WA. Methods for data collection at an individual level. In : Cameron ME, Van Staveren WA, editors. Manual on methodology for food consumption studies. New York: Oxford University Press;1988. p. 53–59.21. Barbaresko J, Koch M, Schulze MB, Nöthlings U. Dietary pattern analysis and biomarkers of low-grade inflammation: a systematic literature review. Nutr Rev. 2013; 71:511–527.
Article22. Suzana S, Noor Aini MY, Nik Shanita S, Rafidah G, Roslina A. Atlas of food exchanges and portion sizes. 2nd ed. Kuala Lumpur: MDC Publishers;2009.23. Norimah AK Jr, Safiah M, Jamal K, et al. Food consumption patterns: findings from the Malaysian Adult Nutrition Survey (MANS). Malays J Nutr. 2008; 14:25–39.24. Tee ES, Ismail MN, Nasir MA, Khatijah I. Nutrient composition of Malaysian foods. 4th ed. Kuala Lumpur: Institute for Medical Research;1997.25. National Coordinating Committee on Food and Nutrition. RNI Recommended Nutrient Intake for Malaysia: a report of the Technical Working Group on Nutritional Guideline. Putrajaya: Ministry of Health Malaysia;2017.26. Kinsey L, Burden S. A survey of people with inflammatory bowel disease to investigate their views of food and nutritional issues. Eur J Clin Nutr. 2016; 70:852–854.
Article27. Powell-Tuck J, Bown RL, Lennard-Jones JE. A comparison of oral prednisolone given as single or multiple daily doses for active proctocolitis. Scand J Gastroenterol. 1978; 13:833–837.
Article28. Ismail IS, Bebakar WM, Kamaruddin NA. Clinical practice guideline on management of obesity 2004. Putrajaya: Ministry of Health Malaysia, Academy of Medicine of Malaysia Malaysian Association for the Study of Obesity, Malaysian Endocrine and Metabolic Society;2004.29. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. National Institutes of Health. 1998; 6 Suppl 2–51S209S.30. Kondrup J, Allison SP, Elia M, et al. ESPEN guidelines for nutrition screening 2002. Clin Nutr. 2003; 22:415–421.
Article31. Forbes A, Escher J, Hébuterne X, et al. ESPEN guideline: clinical nutrition in inflammatory bowel disease. Clin Nutr. 2017; 36:321–347.
Article32. Marsh A, Kinneally J, Robertson T, Lord A, Young A, Radford Smith G. Food avoidance in outpatients with inflammatory bowel disease: who, what and why. Clin Nutr ESPEN. 2019; 31:10–16.
Article33. Bergeron F, Bouin M, D’Aoust L, Lemoyne M, Presse N. Food avoidance in patients with inflammatory bowel disease: what, when and who? Clin Nutr. 2018; 37:884–889.
Article34. Owczarek D, Rodacki T, Domagała-Rodacka R, Cibor D, Mach T. Diet and nutritional factors in inflammatory bowel diseases. World J Gastroenterol. 2016; 22:895–905.
Article35. Vidarsdottir JB, Johannsdottir SE, Thorsdottir I, Bjornsson E, Ramel A. A cross-sectional study on nutrient intake and -status in inflammatory bowel disease patients. Nutr J. 2016; 15:61.
Article36. Magee EA, Richardson CJ, Hughes R, Cummings JH. Contribution of dietary protein to sulfide production in the large intestine: an in vitro and a controlled feeding study in humans. Am J Clin Nutr. 2000; 72:1488–1494.
Article37. Nakahigashi M, Yamamoto T. Increases in body mass index during infliximab therapy in patients with Crohn’s disease: an open label prospective study. Cytokine. 2011; 56:531–535.
Article38. Wiese D, Lashner B, Seidner D. Measurement of nutrition status in Crohn’s disease patients receiving infliximab therapy. Nutr Clin Pract. 2008; 23:551–556.
Article39. Gatt K, Schembri J, Katsanos KH, et al. Inflammatory bowel disease [IBD] and physical activity: a study on the impact of diagnosis on the level of exercise amongst patients with IBD. J Crohns Colitis. 2019; 13:686–692.
Article40. Hou JK, Lee D, Lewis J. Diet and inflammatory bowel disease: review of patient-targeted recommendations. Clin Gastroenterol Hepatol. 2014; 12:1592–1600.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Association of Household Food Security with Dietary Intake: Based on the Third (2005) Korea National Health and Nutrition Examination Survey (KNHANES III)
- Food Elimination Diet and Nutritional Deficiency in Patients with Inflammatory Bowel Disease
- Fast Food Intake Frequency and Health Practices
- Food Diversity and Nutrient Intake of Elementary School Students in Daegu-Kyungbook Area
- Nutrient Intake and Bone Mineral Density by Nutritional Status in Patients with Inflammatory Bowel Disease