Korean Circ J.
2020 Nov;50(11):998-1009. 10.4070/kcj.2020.0065.
Long-term Clinical Outcomes of Radiofrequency Catheter Ablation versus Permanent Pacemaker Implantation in Patients with Tachycardia-Bradycardia Syndrome
- Affiliations
-
- 1Department of Internal Medicine, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea
- 2Cardiovascular Center, Kyung Hee University Hospital at Gangdong, Seoul, Korea
- 3Division of Cardiology, Department of Internal Medicine, Pusan National University Yangsan Hospital, Pusan National University of Medicine, Yangsan, Korea
- 4Division of Cardiology, Department of Internal Medicine, Soonchunhyang University Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea
- 5Division of Cardiology, Department of Internal Medicine, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea
- 6Division of Cardiology, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 7Division of Cardiology, Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University, Seoul, Korea
- KMID: 2508277
- DOI: http://doi.org/10.4070/kcj.2020.0065
Abstract
- Background and Objectives
Pacemaker (PM) implantation is a well-accepted treatment option for patients with paroxysmal atrial fibrillation (AF) and related tachycardiabradycardia syndrome (TBS). Data on the long-term clinical outcomes after radiofrequency catheter ablation (RFCA) or PM implantation are sparse.
Methods
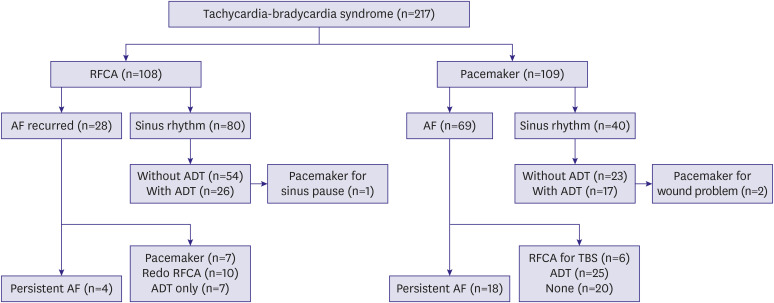
The medical records of 217 patients with TBS were retrospectively assessed. Outcomes in patients who underwent RFCA (n=108, 49.8%) were compared to those with PM implantation (n=109, 50.2%). The clinical outcomes were sinus rhythm maintenance, conversion to persistent AF, additional procedure or crossover, and the composite of cardiovascular hospitalization and death.
Results
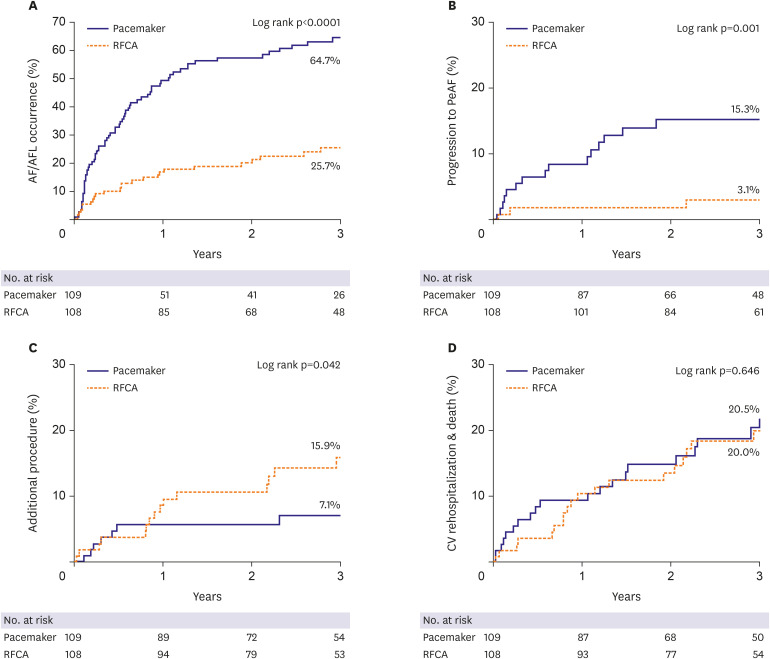
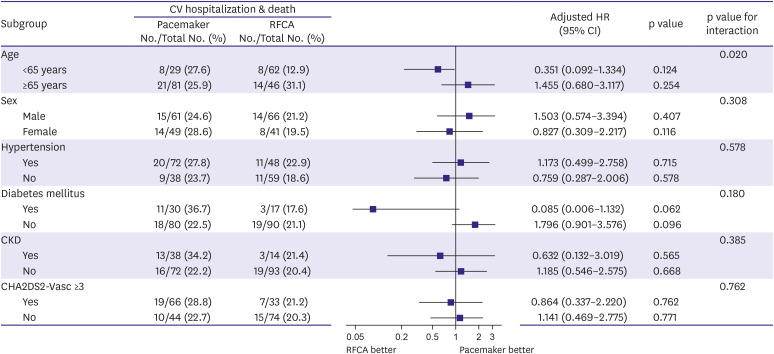
During the follow-up period (mean 3.5±2.0 years), the RFCA group, compared to the PM group, showed better sinus rhythm maintenance (adjusted hazard ratio [aHR], 0.27; 95% confidence interval [CI], 0.15–0.46; p=0.002) and less progression to persistent AF (aHR, 0.20; 95% CI, 0.06–0.63; p=0.006). Additional procedure or crossover did not differ significantly between the groups (aHR, 2.07; 95% CI, 0.71–6.06; p=0.185 and aHR, 0.69; 95% CI, 10.8–2.67; p=0.590, respectively). Most RFCA patients (92.6%) did not require pacemaker implantation during long term follow-up period (>3.5 years). The composite endpoint of cardiovascular rehospitalization and death was not significantly different between the groups (aHR, 0.92; 95% CI, 0.50–1.66; p=0.769). Background and Objectives: Pacemaker (PM) implantation is a well-accepted treatment option for patients with paroxysmal atrial fibrillation (AF) and related tachycardiabradycardia syndrome (TBS). Data on the long-term clinical outcomes after radiofrequency catheter ablation (RFCA) or PM implantation are sparse.
Methods
The medical records of 217 patients with TBS were retrospectively assessed. Outcomes in patients who underwent RFCA (n=108, 49.8%) were compared to those with PM implantation (n=109, 50.2%). The clinical outcomes were sinus rhythm maintenance, conversion to persistent AF, additional procedure or crossover, and the composite of cardiovascular hospitalization and death.
Results
During the follow-up period (mean 3.5±2.0 years), the RFCA group, compared to the PM group, showed better sinus rhythm maintenance (adjusted hazard ratio [aHR], 0.27; 95% confidence interval [CI], 0.15–0.46; p=0.002) and less progression to persistent AF (aHR, 0.20; 95% CI, 0.06–0.63; p=0.006). Additional procedure or crossover did not differ significantly between the groups (aHR, 2.07; 95% CI, 0.71–6.06; p=0.185 and aHR, 0.69; 95% CI, 10.8–2.67; p=0.590, respectively). Most RFCA patients (92.6%) did not require pacemaker implantation during long term follow-up period (>3.5 years). The composite endpoint of cardiovascular rehospitalization and death was not significantly different between the groups (aHR, 0.92; 95% CI, 0.50–1.66; p=0.769).
Conclusions
RFCA is an effective alternative to PM implantation in patients with TBS. In these patients, successful RF ablation of AF is related to a higher rate of sinus rhythm maintenance compared to PM implantation, and the composite outcome of cardiovascular rehospitalization and death is similar.
Keyword
Figure
Cited by 1 articles
-
Management of Tachycarida-bradycardia Syndrome: To Pace or to Ablate, That Is the Question
Jaemin Shim
Korean Circ J. 2020;50(11):1010-1012. doi: 10.4070/kcj.2020.0363.
Reference
-
1. Ferrer MI. The sick sinus syndrome in atrial disease. JAMA. 1968; 206:645–646. PMID: 5695590.
Article3. Ganesan AN, Shipp NJ, Brooks AG, et al. Long-term outcomes of catheter ablation of atrial fibrillation: a systematic review and meta-analysis. J Am Heart Assoc. 2013; 2:e004549. PMID: 23537812.
Article4. Chen YW, Bai R, Lin T, et al. Pacing or ablation: which is better for paroxysmal atrial fibrillation-related tachycardia-bradycardia syndrome? Pacing Clin Electrophysiol. 2014; 37:403–411. PMID: 24456243.
Article5. Inada K, Yamane T, Tokutake K, et al. The role of successful catheter ablation in patients with paroxysmal atrial fibrillation and prolonged sinus pauses: outcome during a 5-year follow-up. Europace. 2014; 16:208–213. PMID: 23751930.
Article6. Hada M, Miyazaki S, Kajiyama T, et al. Catheter ablation of paroxysmal atrial fibrillation in patients with sick sinus syndrome. Heart Vessels. 2019; 34:503–508. PMID: 30178186.
Article7. Wu JT, Dong JZ, Sang CH, Tang RB, Li XH, Ma CS. Efficacy of catheter ablation for atrial fibrillation in patients with a permanent pacemaker for sick sinus syndrome. Intern Med. 2013; 52:2305–2310. PMID: 24126390.
Article8. European Society of Cardiology (ESC). European Heart Rhythm Association (EHRA). Brignole M, et al. 2013 ESC guidelines on cardiac pacing and cardiac resynchronization therapy: the task force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Europace. 2013; 15:1070–1118. PMID: 23801827.9. Epstein AE, DiMarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices): developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons. Circulation. 2008; 117:e350–e408. PMID: 18483207.
Article10. Rajappan K. Permanent pacemaker implantation technique: part I: arrhythmias. Heart. 2009; 95:259–264. PMID: 19144885.11. Rajappan K. Permanent pacemaker implantation technique: part II. Heart. 2009; 95:334–342. PMID: 19176569.
Article12. Sanders P, Morton JB, Kistler PM, et al. Electrophysiological and electroanatomic characterization of the atria in sinus node disease: evidence of diffuse atrial remodeling. Circulation. 2004; 109:1514–1522. PMID: 15007004.13. Khaykin Y, Marrouche NF, Martin DO, et al. Pulmonary vein isolation for atrial fibrillation in patients with symptomatic sinus bradycardia or pauses. J Cardiovasc Electrophysiol. 2004; 15:784–789. PMID: 15250863.
Article14. Ohkubo K, Watanabe I, Okumura Y, et al. Pulmonary vein isolation for atrial fibrillation in patients with paroxysmal atrial fibrillation and prolonged sinus pause. Int Heart J. 2007; 48:247–252. PMID: 17409589.
Article15. Miyanaga S, Yamane T, Date T, et al. Impact of pulmonary vein isolation on the autonomic modulation in patients with paroxysmal atrial fibrillation and prolonged sinus pauses. Europace. 2009; 11:576–581. PMID: 19363052.
Article16. Pokushalov E, Romanov A, Corbucci G, et al. Ablation of paroxysmal and persistent atrial fibrillation: 1-year follow-up through continuous subcutaneous monitoring. J Cardiovasc Electrophysiol. 2011; 22:369–375. PMID: 20958836.
Article17. Weerasooriya R, Khairy P, Litalien J, et al. Catheter ablation for atrial fibrillation: are results maintained at 5 years of follow-up? J Am Coll Cardiol. 2011; 57:160–166. PMID: 21211687.18. Berruezo A, Tamborero D, Mont L, et al. Pre-procedural predictors of atrial fibrillation recurrence after circumferential pulmonary vein ablation. Eur Heart J. 2007; 28:836–841. PMID: 17395676.
Article19. Wilber DJ, Pappone C, Neuzil P, et al. Comparison of antiarrhythmic drug therapy and radiofrequency catheter ablation in patients with paroxysmal atrial fibrillation: a randomized controlled trial. JAMA. 2010; 303:333–340. PMID: 20103757.20. Kim DH, Choi JI, Lee KN, et al. Long-term clinical outcomes of catheter ablation in patients with atrial fibrillation predisposing to tachycardia-bradycardia syndrome: a long pause predicts implantation of a permanent pacemaker. BMC Cardiovasc Disord. 2018; 18:106. PMID: 29843616.
Article21. Pappone C, Rosanio S, Augello G, et al. Mortality, morbidity, and quality of life after circumferential pulmonary vein ablation for atrial fibrillation: outcomes from a controlled nonrandomized long-term study. J Am Coll Cardiol. 2003; 42:185–197. PMID: 12875749.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A single‑center outcome of choosing catheter ablation as the initial treatment in tachycardia–bradycardia syndrome and a new predictive factor for pacemaker implantation
- Permanent Pacemaker Implantations after Catheter Ablation in Patients with Atrial Fibrillation Associated with Underlying Sinus Node Dysfunction
- Diagnostic usefulness of implantable loop recorder in patients with unexplained syncope or palpitation
- A Case of Permanent Junctional Reciprocating Tachycardia Treated with Radiofrequency Catheter Ablation
- Treatment of Tachycardia and Bradycardia in a Persistent Left Superior Vena Cava Patient Who Underwent Warden's Procedure and Tricuspid Annuloplasty