Endocrinol Metab.
2020 Sep;35(3):595-601. 10.3803/EnM.2020.719.
Fasting Plasma Glucose Level Independently Predicts the Mortality of Patients with Coronavirus Disease 2019 Infection: A Multicenter, Retrospective Cohort Study
- Affiliations
-
- 1Department of Rehabilitation Medicine, Yeungnam University College of Medicine, Daegu, Korea
- 2Department of Rehabilitation Medicine, School of Medicine, Kyungpook National University, Daegu, Korea
- 3Department of Internal Medicine, School of Medicine, Kyungpook National University, Daegu, Korea
- 4Department of Medical Statistics, Daegu Catholic University School of Medicine, Daegu, Korea
- 5Department of Physical Medicine and Rehabilitation, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea
- 6Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea
- KMID: 2508009
- DOI: http://doi.org/10.3803/EnM.2020.719
Abstract
- Background
Coronavirus disease 2019 (COVID-19) has become a global pandemic, which prompts a consensus for the necessity to seek risk factors for this critical disease. Risk factors affecting mortality of the disease remain elusive. Diabetes and hyperglycemia are known to negatively affect a host’s antiviral immunity. We evaluated the relationship between a history of diabetes, fasting plasma glucose (FPG) levels and mortality among severely ill patients with COVID-19.
Methods
This was a retrospective cohort study that assessed 106 adult inpatients (aged ≥18 years) from two tertiary hospitals in Daegu, South Korea. The participants were transferred to tertiary hospitals because their medical condition required immediate intensive care. The demographic and laboratory data were compared between COVID-19 patients who survived and those who did not.
Results
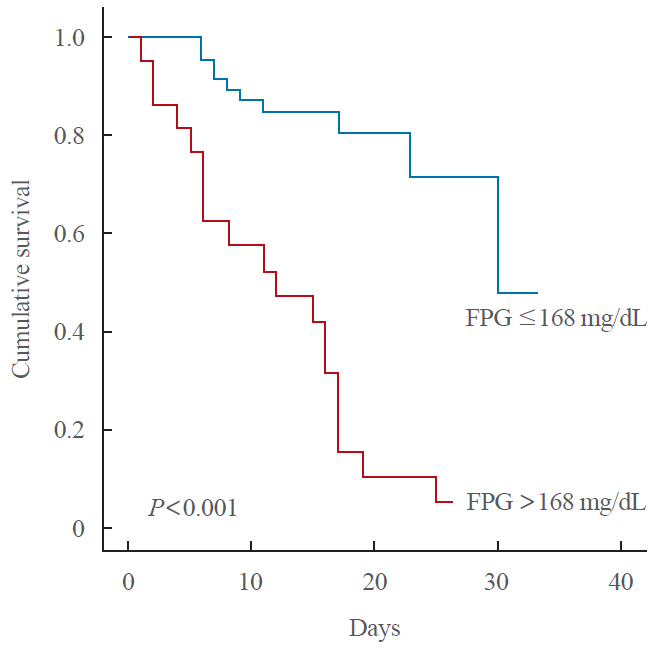
Compared with the survivor group, age, and the proportions of diabetes, chronic lung disease and FPG were significantly higher in the deceased group. In the Cox proportional hazards regression model for survival analysis, FPG level and age were identified as significant predictors of mortality (P<0.05). The threshold values for predicting high mortality were age >68 years and FPG of 168 mg/dL, respectively. Among those without diabetes, high FPG remained a significant predictor of mortality (P<0.04).
Conclusion
High FPG levels significantly predicted mortality in COVID-19, regardless of a known history of diabetes. These results suggest intensive monitoring should be provided to COVID-19 patients who have a high FPG level.
Keyword
Figure
Cited by 2 articles
-
Thyroid Hormone Profile and Its Prognostic Impact on the Coronavirus Disease 2019 in Korean Patients
Jiyeon Ahn, Min Kyung Lee, Jae Hyuk Lee, Seo Young Sohn
Endocrinol Metab. 2021;36(4):769-777. doi: 10.3803/EnM.2021.1109.Impact of Antidiabetic Drugs on Clinical Outcomes of COVID-19: A Nationwide Population-Based Study
Han Na Jang, Sun Joon Moon, Jin Hyung Jung, Kyung-Do Han, Eun-Jung Rhee, Won-Young Lee
Endocrinol Metab. 2024;39(3):479-488. doi: 10.3803/EnM.2023.1857.
Reference
-
1. Chang MC, Park D. How should rehabilitative departments of hospitals prepare for coronavirus disease 2019? Am J Phys Med Rehabil. 2020; 99:475–6.
Article2. Kucharski AJ, Russell TW, Diamond C, Liu Y, Edmunds J, Funk S, et al. Early dynamics of transmission and control of COVID-19: a mathematical modelling study. Lancet Infect Dis. 2020; 20:553–8.
Article3. Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R. Features, evaluation and treatment coronavirus (COVID-19). Treasure Island: StatPearls;2020.4. Kim SW, Lee KS, Kim K, Lee JJ, Kim JY; Daegu Medical Association. A brief telephone severity scoring system and therapeutic living centers solved acute hospital-bed shortage during the COVID-19 outbreak in Daegu, Korea. J Korean Med Sci. 2020; 35:e152.
Article5. Heymann DL, Shindo N; WHO Scientific and Technical Advisory Group for Infectious Hazards. COVID-19: what is next for public health? Lancet. 2020; 395:542–5.
Article6. Shah BR, Hux JE. Quantifying the risk of infectious diseases for people with diabetes. Diabetes Care. 2003; 26:510–3.
Article7. Wurtz R, Cameron BJ. Electronic laboratory reporting for the infectious diseases physician and clinical microbiologist. Clin Infect Dis. 2005; 40:1638–43.
Article8. Butler SO, Btaiche IF, Alaniz C. Relationship between hyperglycemia and infection in critically ill patients. Pharmacotherapy. 2005; 25:963–76.
Article9. Norhammar AM, Ryden L, Malmberg K. Admission plasma glucose: independent risk factor for long-term prognosis after myocardial infarction even in nondiabetic patients. Diabetes Care. 1999; 22:1827–31.
Article10. Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: an independent marker of inhospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab. 2002; 87:978–82.
Article11. Yang JK, Feng Y, Yuan MY, Yuan SY, Fu HJ, Wu BY, et al. Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS. Diabet Med. 2006; 23:623–8.
Article12. Chung SM, Lee YY, Ha E, Yoon JS, Won KC, Lee HW, et al. The risk of diabetes on clinical outcomes in patients with coronavirus disease 2019: a retrospective cohort study. Diabetes Metab J. 2020; 44:405–13.
Article13. COVID-19 National Emergency Response Center; Epidemiology and Case Management Team; Korea Centers for Disease Control and Prevention. Coronavirus disease-19: the first 7,755 cases in the Republic of Korea. Osong Public Health Res Perspect. 2020; 11:85–90.14. Kim MK, Ko SH, Kim BY, Kang ES, Noh J, Kim SK, et al. 2019 Clinical practice guidelines for type 2 diabetes mellitus in Korea. Diabetes Metab J. 2019; 43:398–406.
Article15. Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012; 120:c179–84.
Article16. Casqueiro J, Casqueiro J, Alves C. Infections in patients with diabetes mellitus: a review of pathogenesis. Indian J Endocrinol Metab. 2012; 16 Suppl 1:S27–36.17. Joshi N, Caputo GM, Weitekamp MR, Karchmer AW. Infections in patients with diabetes mellitus. N Engl J Med. 1999; 341:1906–12.
Article18. Brufsky A. Hyperglycemia, hydroxychloroquine, and the COVID-19 pandemic. J Med Virol. 2020; 92:770–5.
Article19. Yang JK, Lin SS, Ji XJ, Guo LM. Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes. Acta Diabetol. 2010; 47:193–9.
Article20. Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020; 94:91–5.
Article21. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020; 395:497–506.
Article22. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020; 395:1054–62.
Article23. Tian W, Jiang W, Yao J, Nicholson CJ, Li RH, Sigurslid HH, et al. Predictors of mortality in hospitalized COVID-19 patients: a systematic review and meta-analysis. J Med Virol. 2020; 92:1875–83.
Article24. Won JC, Lee JH, Kim JH, Kang ES, Won KC, Kim DJ, et al. Diabetes fact sheet in Korea, 2016: an appraisal of current status. Diabetes Metab J. 2018; 42:415–24.
Article25. Levetan CS, Passaro M, Jablonski K, Kass M, Ratner RE. Unrecognized diabetes among hospitalized patients. Diabetes Care. 1998; 21:246–9.
Article26. Clement S, Braithwaite SS, Magee MF, Ahmann A, Smith EP, Schafer RG, et al. Management of diabetes and hyperglycemia in hospitals. Diabetes Care. 2004; 27:553–91.
Article27. Kansagara D, Wolf F, Freeman M, Helfand M. Management of inpatient hyperglycemia: a systematic review. Washington DC: Department of Veterans Affairs;2008.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Potential Issue with Screening Prediabetes or Diabetes Using Serum Glucose: A Delay in Diagnosis
- Measurement and Treatment Goal of Postprandial Hyperglycemia
- Role of HbA1c in the Screening of Diabetes Mellitus in a Korean Rural Community
- Plasma leptin Concentrations in Korean Type 2 Diabetic Patients
- Convalescent Plasma Therapy for Coronavirus Disease 2019