Ann Lab Med.
2020 Nov;40(6):457-465. 10.3343/alm.2020.40.6.457.
Exploration and Validation of the Performance of Hemoglobin A1c in Detecting Diabetes in CommunityDwellers With Hypertension
- Affiliations
-
- 1Department of Endocrinology, Zhongda Hospital, Institute of Diabetes, School of Medicine, Southeast University, Nanjing, China
- 2School of Public Health, Southeast University, Nanjing, China
- 3Department of Integrated Services, Jiangsu Provincial Center for Disease Control and Prevention, Nanjing, China
- KMID: 2507791
- DOI: http://doi.org/10.3343/alm.2020.40.6.457
Abstract
- Background
Diabetes can complicate hypertension management by increasing the risk of cardiovascular disease (CVD) and all-cause mortality. Studies targeting diabetes detection in hypertensive individuals demonstrating an increased risk of diabetes are lacking. We aimed to assess the performance of hemoglobin A1c (HbA1c) and its cut-off point in detecting diabetes in the abovementioned population.
Methods
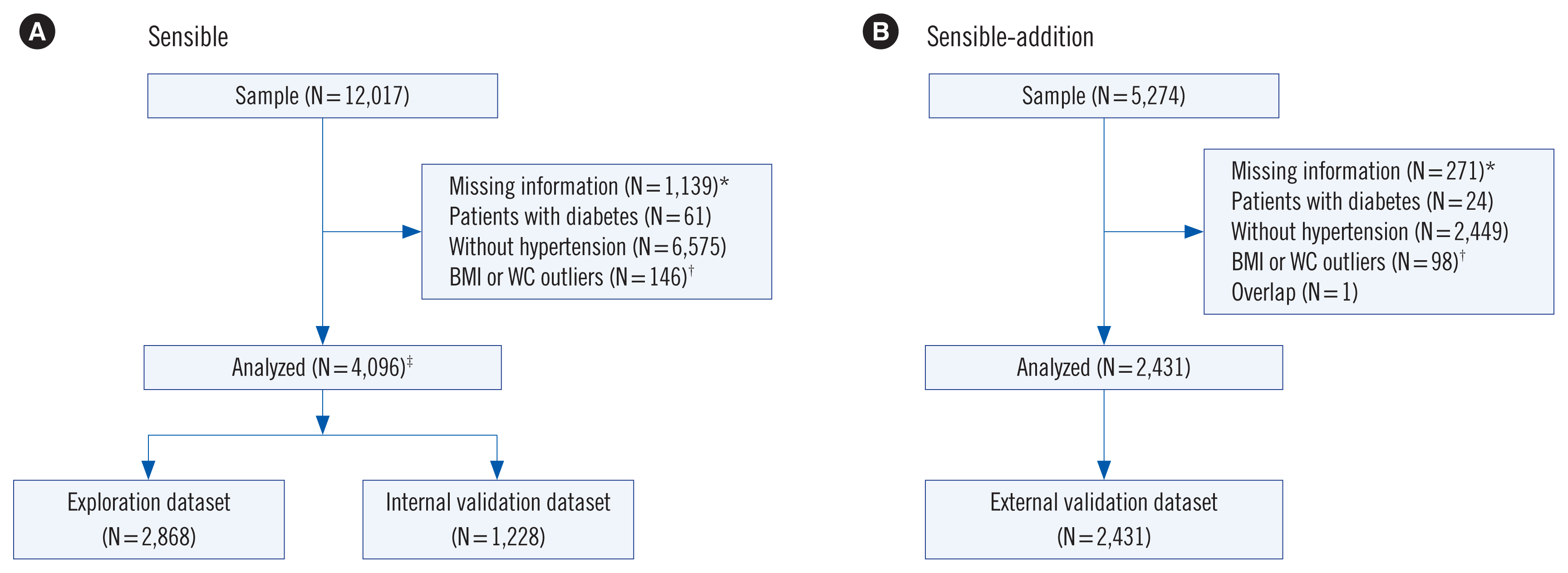
Data from 4,096 community-dwellers with hypertension but without known diabetes were obtained from the Study on Evaluation of iNnovated Screening tools and determInation of optimal diagnostic cut-off points for type 2 diaBetes in Chinese muLti-Ethnic (SENSIBLE) study; these data were randomly split into exploration (70% of the sample) and internal validation (the remaining 30%) datasets. The optimal HbA1c cut-off point was derived from the exploration dataset and externally validated using another dataset from 2,431 hypertensive individuals. The oral glucose tolerance test was considered the goldstandard for confirming diabetes.
Results
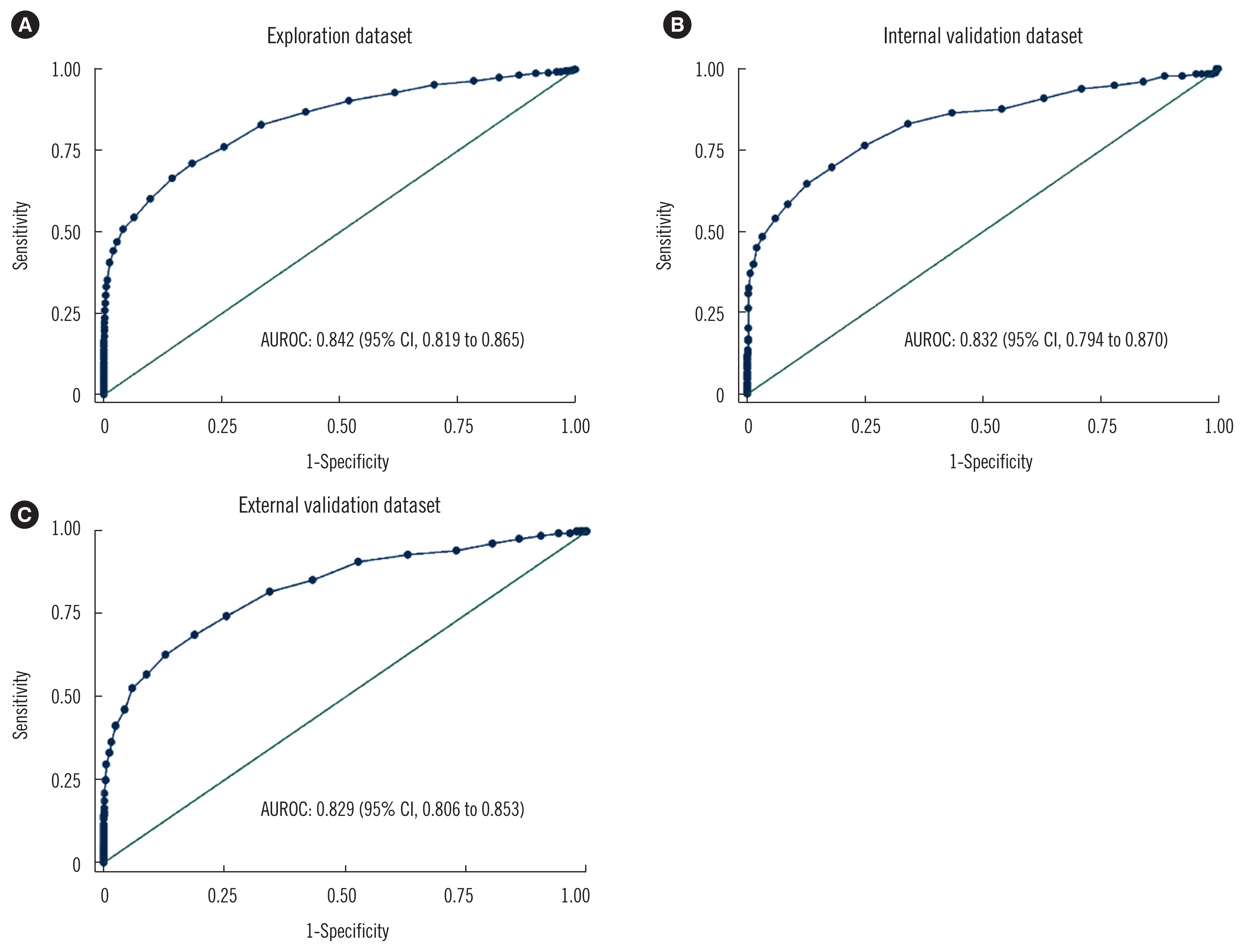
The areas under the ROC curves for HbA1c to detect diabetes were 0.842, 0.832, and 0.829 for the exploration, internal validation, and external validation datasets, respectively. An optimal HbA1c cut-off point of 5.8% (40 mmol/mol) yielded a sensitivity of 76.2% and a specificity of 74.5%. Individuals who were not diagnosed as having diabetes by HbA1c at 5.8% (40 mmol/mol) had a lower 10-year CVD risk score than those diagnosed as having diabetes (P = 0.01). HbA1c ≤ 5.1% (32 mmol/mol) and ≥ 6.4% (46 mmol/mol) could indicate the absence and presence of diabetes, respectively.
Conclusions
HbA1c could detect diabetes effectively in community-dwellers with hypertension.
Keyword
Figure
Reference
-
1. Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016; 134:441–50.2. Lu J, Lu Y, Wang X, Li X, Linderman GC, Wu C, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1.7 million adults in a population-based screening study (China PEACE Million Persons Project). Lancet. 2017; 390:2549–58.
Article3. Tsimihodimos V, Gonzalez-Villalpando C, Meigs JB, Ferrannini E. Hypertension and diabetes mellitus: coprediction and time trajectories. Hypertension. 2018; 71:422–8.4. Li T, Chen S, Guo X, Yang J, Sun Y. Impact of hypertension with or without diabetes on left ventricular remodeling in rural Chinese population: a cross-sectional study. BMC Cardiovasc Disord. 2017; 17:206.
Article5. Thomopoulos C, Parati G, Zanchetti A. Effects of blood-pressure-lowering treatment on outcome incidence in hypertension: 10-Should blood pressure management differ in hypertensive patients with and without diabetes mellitus? Overview and meta-analyses of randomized trials. J Hypertens. 2017; 35:922–44.6. Oh JY, Allison MA, Barrett-Connor E. Different impacts of hypertension and diabetes mellitus on all-cause and cardiovascular mortality in community-dwelling older adults: the Rancho Bernardo Study. J Hypertens. 2017; 35:55–62.7. Zafari N, Asgari S, Lotfaliany M, Hadaegh A, Azizi F, Hadaegh F. Impact of hypertension versus diabetes on cardiovascular and all-cause mortality in Iranian older adults: results of 14 years of follow-up. Sci Rep. 2017; 7:14220.
Article8. Kim MJ, Lim NK, Choi SJ, Park HY. Hypertension is an independent risk factor for type 2 diabetes: the Korean genome and epidemiology study. Hypertens Res. 2015; 38:783–9.
Article9. Tatsumi Y, Morimoto A, Asayama K, Sonoda N, Miyamatsu N, Ohno Y, et al. Risk of developing type 2 diabetes according to blood pressure levels and presence or absence of hypertensive treatment: the Saku study. Hypertens Res. 2019; 42:105–13.
Article10. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010; 33(S1):S62–9.11. Bennett CM, Guo M, Dharmage SC. HbA1c as a screening tool for detection of Type 2 diabetes: a systematic review. Diabet Med. 2007; 24:333–43.12. Bertran EA, Berlie HD, Taylor A, Divine G, Jaber LA. Diagnostic performance of HbA1c for diabetes in Arab vs. European populations: a systematic review and meta-analysis. Diabet Med. 2017; 34:156–66.
Article13. Maesa JM, Fernandez-Riejos P, Gonzalez-Rodriguez C, Sanchez-Margalet V. Screening for gestational diabetes mellitus by measuring glycated hemoglobin can reduce the use of the glucose challenge test. Ann Lab Med. 2019; 39:524–9.
Article14. Ehehalt S, Wiegand S, Körner A, Schweizer R, Liesenkötter KP, Partsch CJ, et al. Diabetes screening in overweight and obese children and adolescents: choosing the right test. Eur J Pediatr. 2017; 176:89–97.
Article15. Li W, Xie B, Qiu S, Huang X, Chen J, Wang X, et al. Non-lab and semi-lab algorithms for screening undiagnosed diabetes: a cross-sectional study. EBioMedicine. 2018; 35:307–16.
Article16. Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig L, et al. STARD 2015: an updated list of essential items for reporting diagnostic accuracy studies. BMJ. 2015; 351:h5527.
Article17. Weykamp C. HbA1c: a review of analytical and clinical aspects. Ann Lab Med. 2013; 33:393–400.
Article18. Gabir MM, Hanson RL, Dabelea D, Imperatore G, Roumain J, Bennett PH, et al. The 1997 American Diabetes Association and 1999 World Health Organization criteria for hyperglycemia in the diagnosis and prediction of diabetes. Diabetes Care. 2000; 23:1108–12.
Article19. D’Agostino RB Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008; 117:743–53.20. Safari S, Baratloo A, Elfil M, Negida A. Evidence based emergency medicine; part 5 receiver operating curve and area under the curve. Emerg (Tehran). 2016; 4:111–3.21. Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ. 2003; 326:219.22. Lu ZX, Walker KZ, O’Dea K, Sikaris KA, Shaw JE. A1C for screening and diagnosis of type 2 diabetes in routine clinical practice. Diabetes Care. 2010; 33:817–9.
Article23. Li G, Han L, Wang Y, Zhao Y, Li Y, Fu J, et al. Evaluation of ADA HbA1c criteria in the diagnosis of pre-diabetes and diabetes in a population of Chinese adolescents and young adults at high risk for diabetes: a cross-sectional study. BMJ Open. 2018; 8:e020665.
Article24. Hoyer A, Rathmann W, Kuss O. Utility of HbA1c and fasting plasma glucose for screening of Type 2 diabetes: a meta-analysis of full ROC curves. Diabet Med. 2018; 35:317–22.
Article25. Franco LJ, Dal Fabbro AL, Martinez EZ, Sartorelli DS, Silva AS, Soares LP, et al. Performance of glycated haemoglobin (HbA1c) as a screening test for diabetes and impaired glucose tolerance (IGT) in a high risk population–the Brazilian Xavante Indians. Diabetes Res Clin Pract. 2014; 106:337–42.
Article26. Peter A, Fritsche A, Stefan N, Heni M, Häring HU, Schleicher E. Diagnostic value of hemoglobin A1c for type 2 diabetes mellitus in a population at risk. Exp Clin Endocrinol Diabetes. 2011; 119:234–7.
Article27. Lee H, Oh JY, Sung YA, Kim DJ, Kim SH, Kim SG, et al. Optimal hemoglobin A1C cutoff value for diagnosing type 2 diabetes mellitus in Korean adults. Diabetes Res Clin Pract. 2013; 99:231–6.
Article28. Smith AD, Crippa A, Woodcock J, Brage S. Physical activity and incident type 2 diabetes mellitus: a systematic review and dose–response meta-analysis of prospective cohort studies. Diabetologia. 2016; 59:2527–45.
Article29. Casula M, Mozzanica F, Scotti L, Tragni E, Pirillo A, Corrao G, et al. Statin use and risk of new-onset diabetes: a meta-analysis of observational studies. Nutr Metab Cardiovasc Dis. 2017; 27:396–406.
Article30. Di Bonito P, Valerio G, Pacifico L, Chiesa C, Invitti C, Morandi A, et al. A new index to simplify the screening of hypertension in overweight or obese youth. Nutr Metab Cardiovasc Dis. 2017; 27:830–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Performance Evaluation of the ARKRAY ADAMS A1c HA-8180
- Factors Associated with Hemoglobin A1c among Patient Aged 40 years over with Diabetes Mellitus: 2012 Korea Health and Nutrition Examination Survey
- The Optimal Cutoff Value of Glycated Hemoglobin for Detection of Diabetic Retinopathy
- HbA1c for Diagnosis of Type 2 Diabetes in Korea
- Performance Evaluation of the ADAMS A1c HA-8180 Analyzer for HbA1c