Ann Pediatr Endocrinol Metab.
2020 Sep;25(3):187-191. 10.6065/apem.1938172.086.
A case of primary hyperparathyroidism due to an intrathymic ectopic parathyroid adenoma in a 15-year-old boy
- Affiliations
-
- 1Department of Pediatrics, Severance Children’s Hospital, Endocrine Research Institute, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2507562
- DOI: http://doi.org/10.6065/apem.1938172.086
Abstract
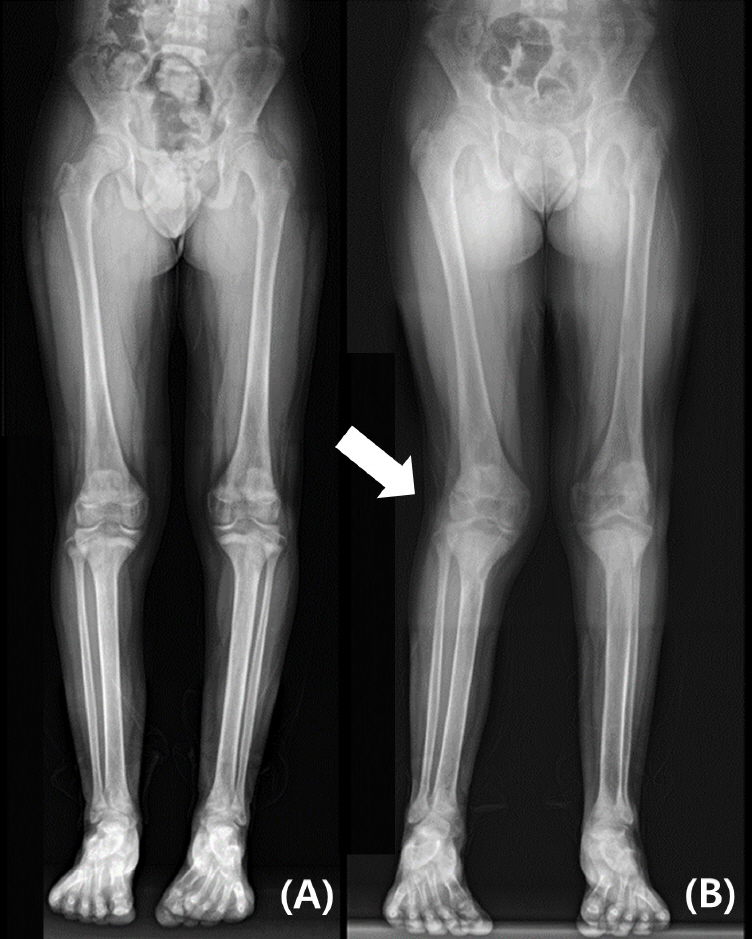
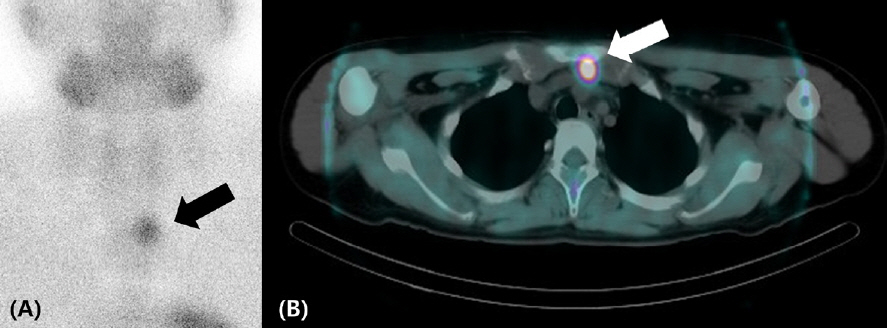
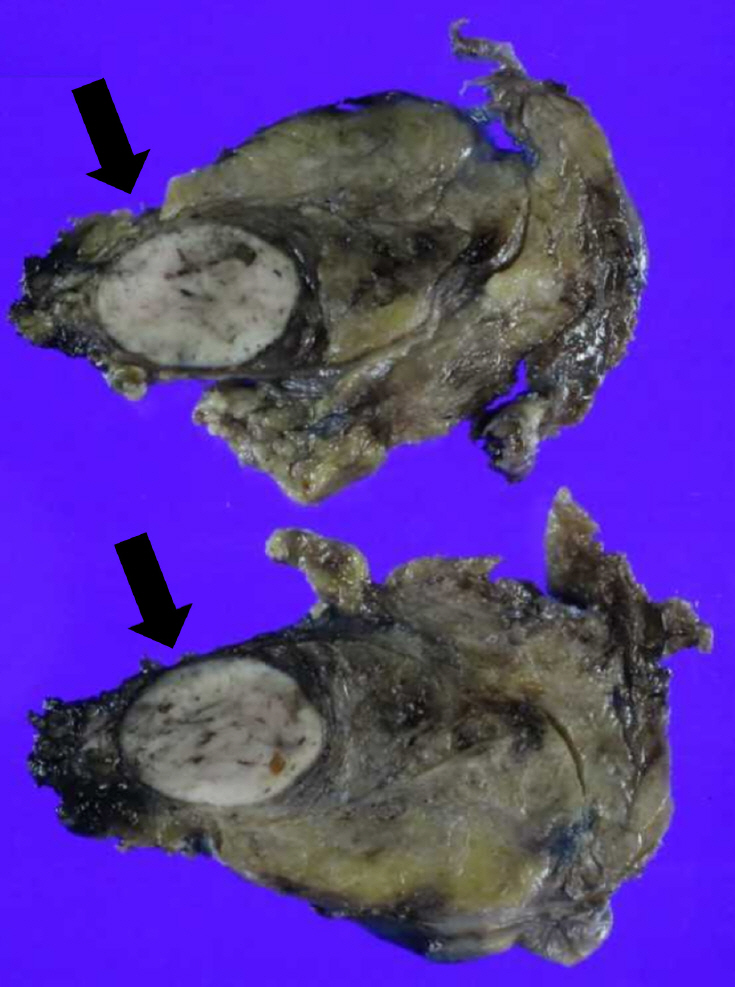
- Hypercalcemia due to primary hyperparathyroidism (PHPT) is uncommon in children. PHPT is typically caused by a single parathyroid adenoma. Ectopic parathyroid adenomas account for 6%–16% of all parathyroid adenomas and are rare in children but should be considered in cases that present with hypercalcemia. We report the case of a 15-year-old boy with PHPT due to an intrathymic ectopic parathyroid adenoma. Neck ultrasonography and Tc-99m-sestamibi (MIBI) scanning with single-photon emission computed tomography/computed tomography (SPECT/CT) revealed ectopic parathyroid adenoma in the thymus. Video-assisted thoracoscopic surgery was performed to remove the ectopic parathyroid adenoma. Pathology showed intrathymic ectopic parathyroid adenoma. After surgery, the patient’s serum calcium level immediately normalized. Intact parathyroid hormone (iPTH) and alkaline phosphatase levels returned to normal ranges within 3 months. Delayed diagnosis of PHPT can cause end-organ damage; a timely diagnosis is especially critical to preserve bone and renal function. If ectopic parathyroid adenomas are well localized in preoperative imaging evaluation and intraoperative iPTH level decreases after resection, ectopic parathyroidectomy without bilateral neck exploration may be performed to avoid unnecessary morbidity.
Keyword
Figure
Reference
-
References
1. McNeilly JD, Boal R, Shaikh MG, Ahmed SF. Frequency and aetiology of hypercalcaemia. Arch Dis Child. 2016; 101:344–7.
Article2. Stokes VJ, Nielsen MF, Hannan FM, Thakker RV. Hypercalcemic disorders in children. J B one Miner Res. 2017; 32:2157–70.
Article3. Bilezikian JP. Primary hyperparathyroidism. J Clin Endocrinol Metabol. 2018; 103:3993–4004.
Article4. Cormier C. Genetic hypercalcemia. Joint Bone Spine. 2019; 86:459–66.
Article5. Walker MD, Silverberg SJ. Primary hyperparathyroidism. Nat Rev Endocrinol. 2018; 14:115–25.
Article6. Kollars J, Zarroug AE, van Heerden J, Lteif A, Stavlo P, Suarez L, et al. Primary hyperparathyroidism in pediatric patients. Pediatrics. 2005; 115:974–80.
Article7. Nicholson KJ, McCoy KL, Witchel SF, Stang MT, Carty SE, Yip L. Comparative characteristics of primar y hyperparathyroidism in pediatric and young adult patients. Surgery. 2016; 160:1008–16.
Article8. Roy M, Mazeh H, Chen H, Sippel RS. Incidence and localization of ectopic parathyroid adenomas in previously unexplored patients. World J Surg. 2013; 37:102–6.
Article9. Li CC, Yang C, Wang S, Zhang J, Kong XR, Ouyang J. A 10-year retrospective study of primary hyperparathyroidism in children. Exp Clin Endocrinol Diabetes. 2012; 120:229–33.
Article10. Liu X, Sun L, Shao M, Li P, Liu W, Zhang X, et al. Primary hyperparathyroidism due to ectopic parathyroid adenoma in an adolescent: a case report and review of the literature. Endocrine. 2019; 64:38–42.11. Arambewela MH, Liyanarachchi KD, Somasundaram NP, Pallewatte AS, Punchihewa GL. Case report: rare skeletal manifestations in a child with primary hyperparathyroidism. BMC Endocr Disord. 2017; 17:45.
Article12. Udelsman R, Akerstrom G, Biagini C, Duh QY, Miccoli P, Niederle B, et al. The surgical management of asymptomatic primar y hyperparathyroidism: proceedings of the Fourth International Workshop. J Clin Endocrinol Metab. 2014; 99:3595–606.13. Khan AA, Hanley DA, Rizzoli R, Bollerslev J, Young JE, Rejnmark L, et al. Primary hyperparathyroidism: review and recommendations on evaluation, diagnosis, and management. A Canadian and international consensus. Osteoporos Int. 2017; 28:1–19.
Article14. Cheung K, Wang TS, Farrokhyar F, Roman SA, Sosa JA. A meta-analysis of preoperative localization techniques for patients with primary hyperparathyroidism. Ann Surg Oncol. 2012; 19:577–83.
Article15. Iihara M, Suzuki R, Kawamata A, Horiuchi K, Okamoto T. Thoracoscopic removal of mediastinal parathyroid lesions: selection of surgical approach and pitfalls of preoperative and intraoperative localization. World J Surg. 2012; 36:1327–34.
Article16. Kaplan EL, Yashiro T, Salti G. Primary hyperparathyroidism in the 1990s. Choice of surgical procedures for this disease. Ann Surg. 1992; 215:300–17.17. Chou PL, Chao YK, Liu YH. Minimally invasive removal of mediastinal ectopic parathyroid glands: a single-center experience. Formos J Surg. 2019; 52:6–10.18. Said SM, Cassivi SD, Allen MS, Deschamps C, Nichols FC 3rd, Shen KR, et al. Minimally invasive resection for mediastinal ectopic parathyroid glands. Ann Thorac Surg. 2013; 96:1229–33.
Article19. Thakker RV, Newey PJ, Walls GV, Bilezikian J, Dralle H, Ebeling PR, et al. Clinical practice guidelines for multiple endocrine neoplasia type 1 (MEN1). J Clin Endocrinol Metabol. 2012; 97:2990–3011.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Parathyroid Adenoma without Hyperparathyroidism Presenting as a Large Neck Mass
- A Case of Hyperparathyroidism Caused by Intrathyroidal Parathyroid Adenoma
- Benign Recurrent Primary Hyperparathyroidism After Parathyroid Carcinoma
- Supernumerary Ectopic Mediastinal Parathyroid Adenoma Combined With Parathyroid Hyperplasia
- Giant Parathyroid Adenoma in the Posterior Mediastinum