Korean J Transplant.
2020 Sep;34(3):134-150. 10.4285/kjt.2020.34.3.134.
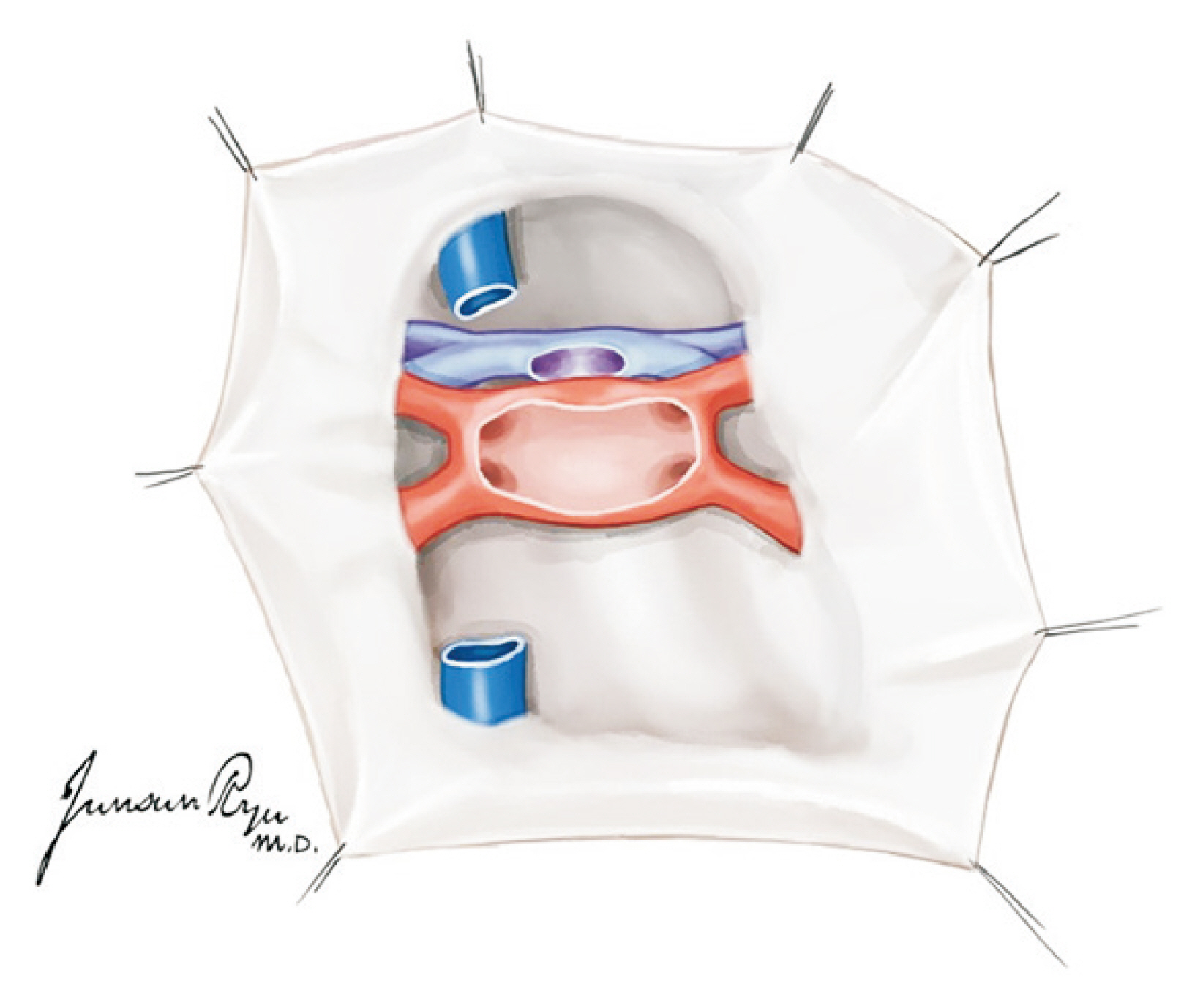
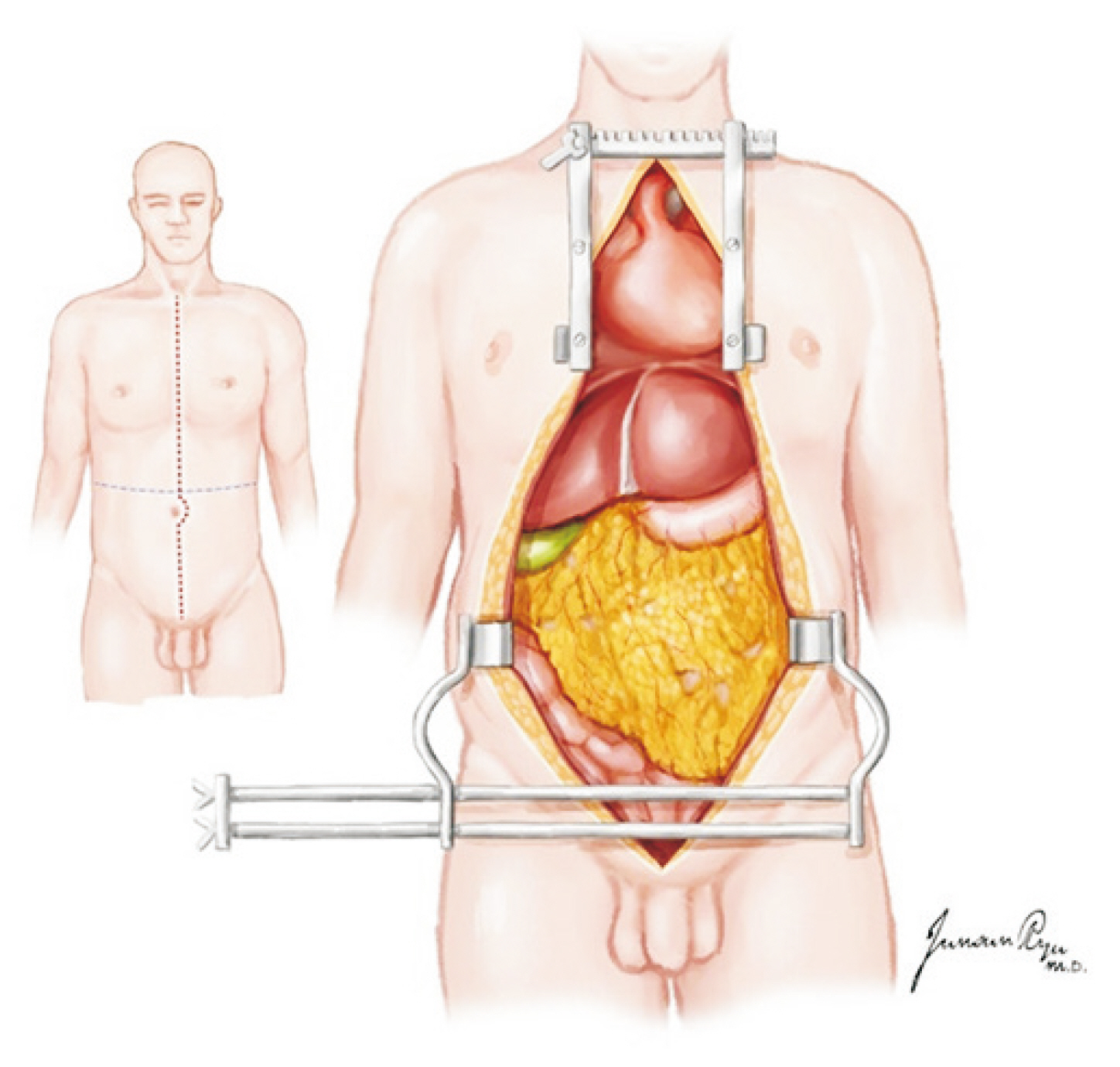
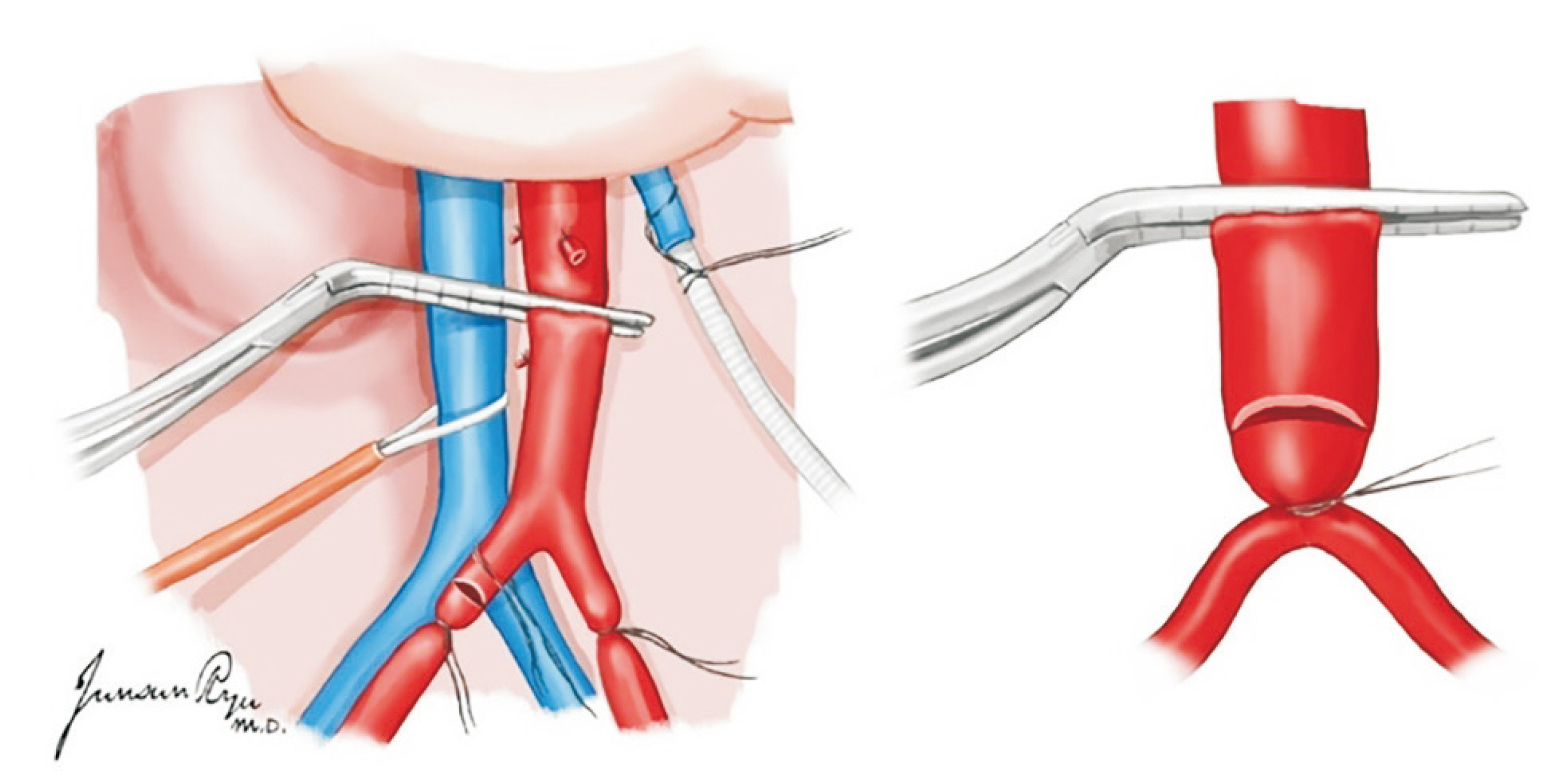
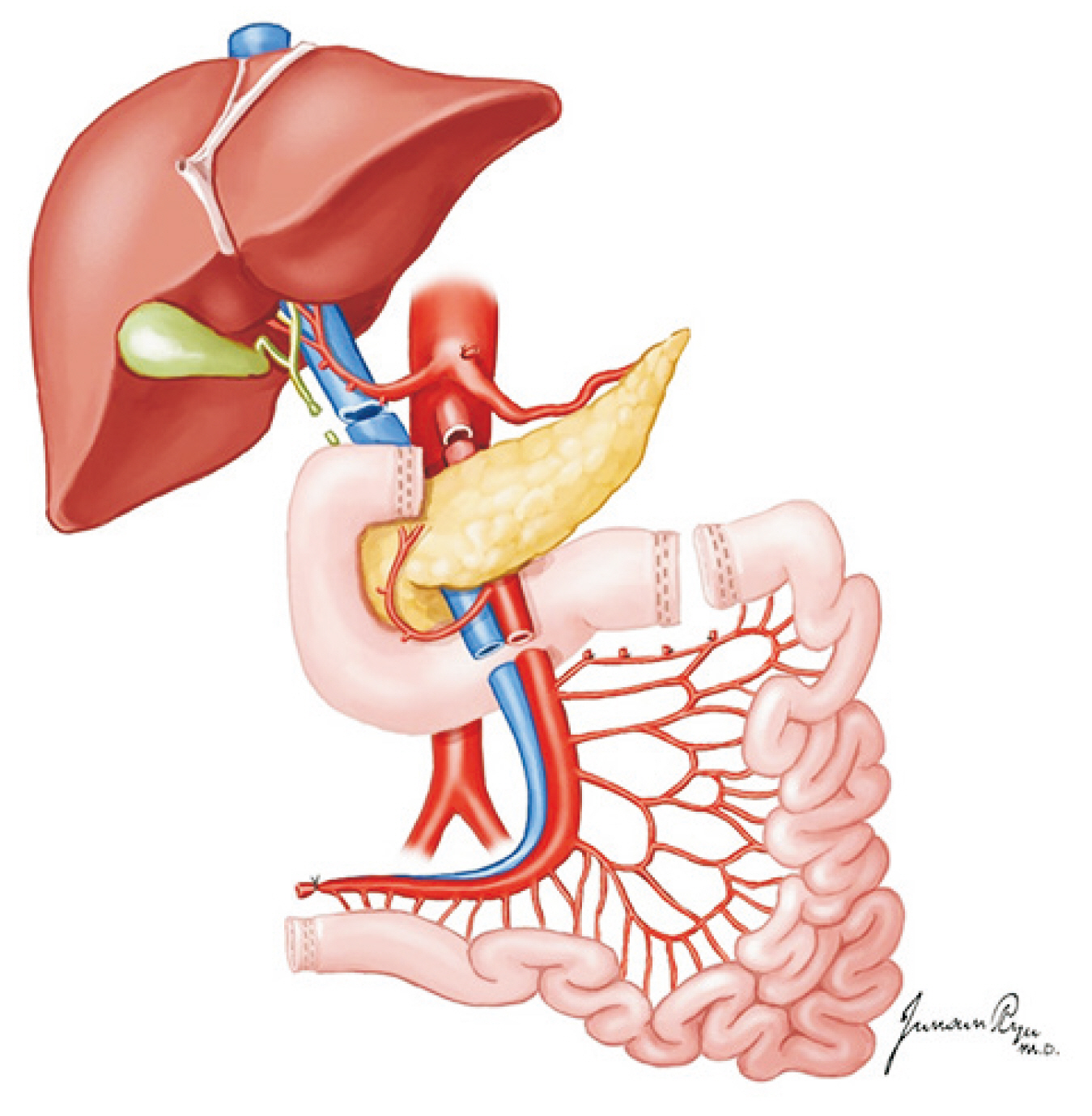
Organ procurement in a deceased donor
- Affiliations
-
- 1Department of Surgery, Jeonbuk National University Medical School and Hospital, Jeonju, Korea
- 2Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 4Division of Transplantation and Vascular Surgery, Department of Surgery, Kyung Hee University College of Medicine, Seoul, Korea
- 5Department of Internal Medicine, Jeonbuk National University Medical School, Jeonju, Korea
- 6Department of Surgery, Yonsei University College of Medicine, Seoul, Korea
- 7Department of Internal Medicine, Keimyung University School of Medicine, Daegu, Korea
- 8Department of Thoracic and Cardiovascular Surgery, Ajou University School of Medicine, Suwon, Korea
- 9Department of Surgery, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 10Department of Surgery, Research Institute of Clinical Medicine, Biomedical Research Institute, Jeonbuk National University Medical School and Hospital, Jeonju, Korea
- KMID: 2507153
- DOI: http://doi.org/10.4285/kjt.2020.34.3.134
Abstract
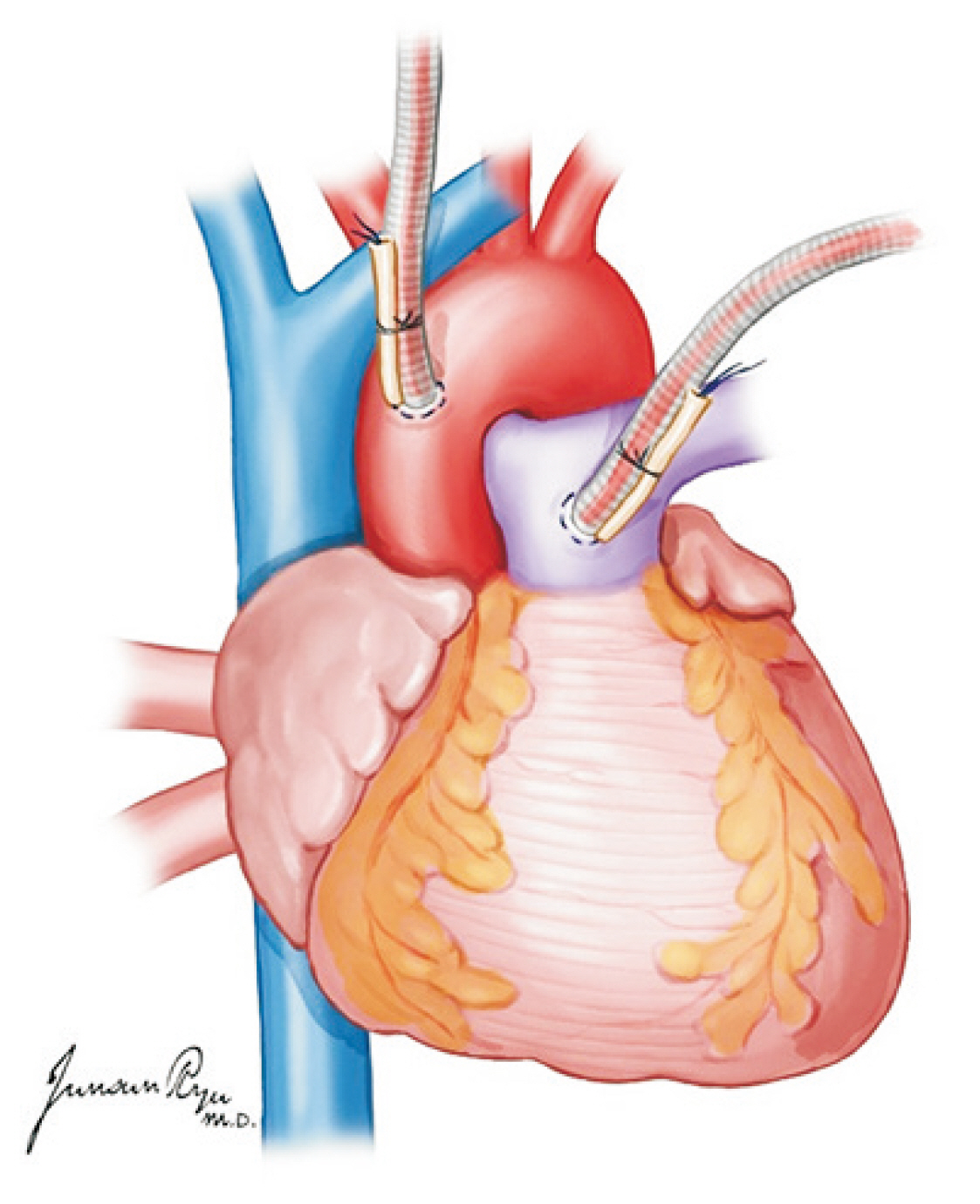
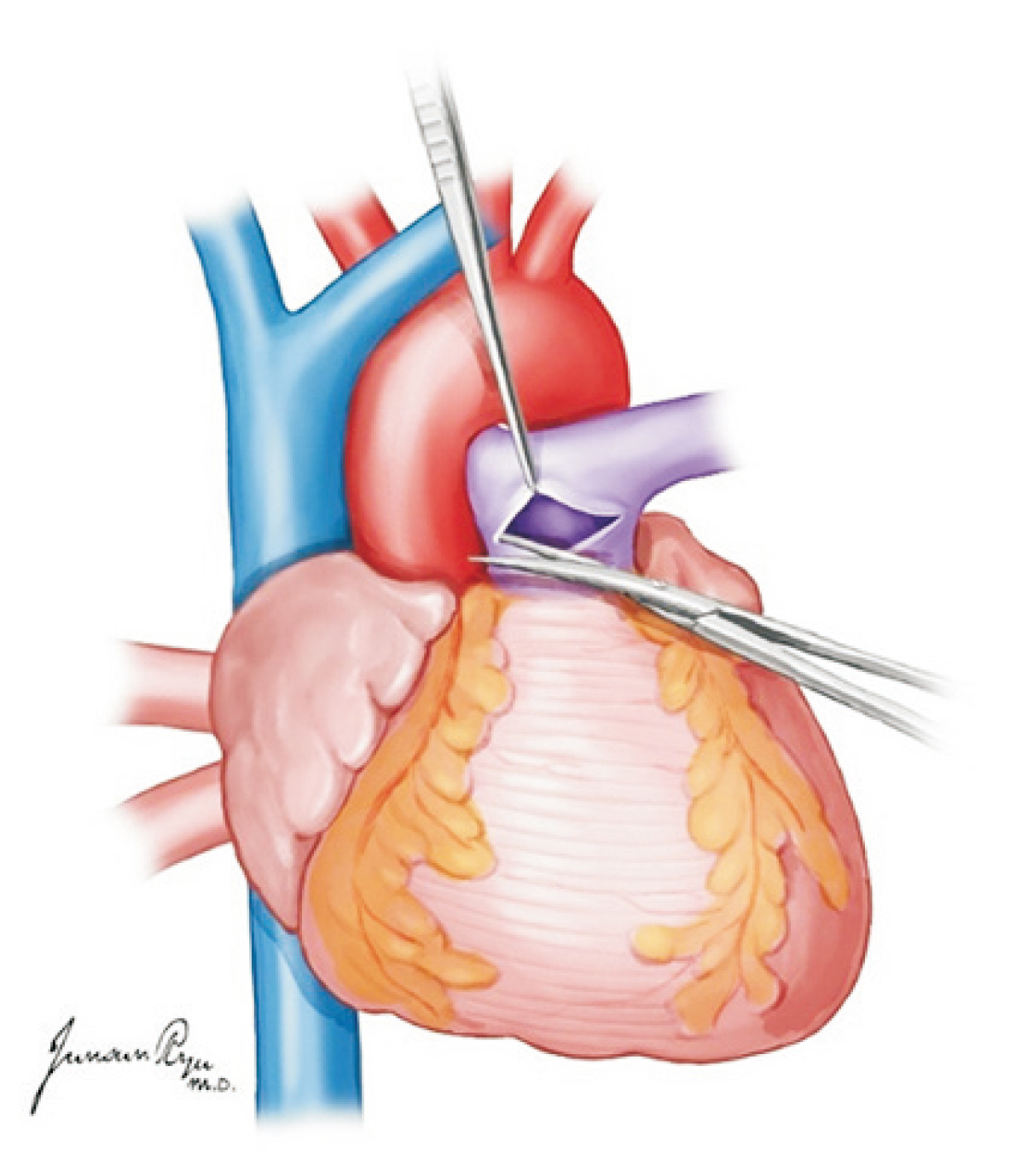
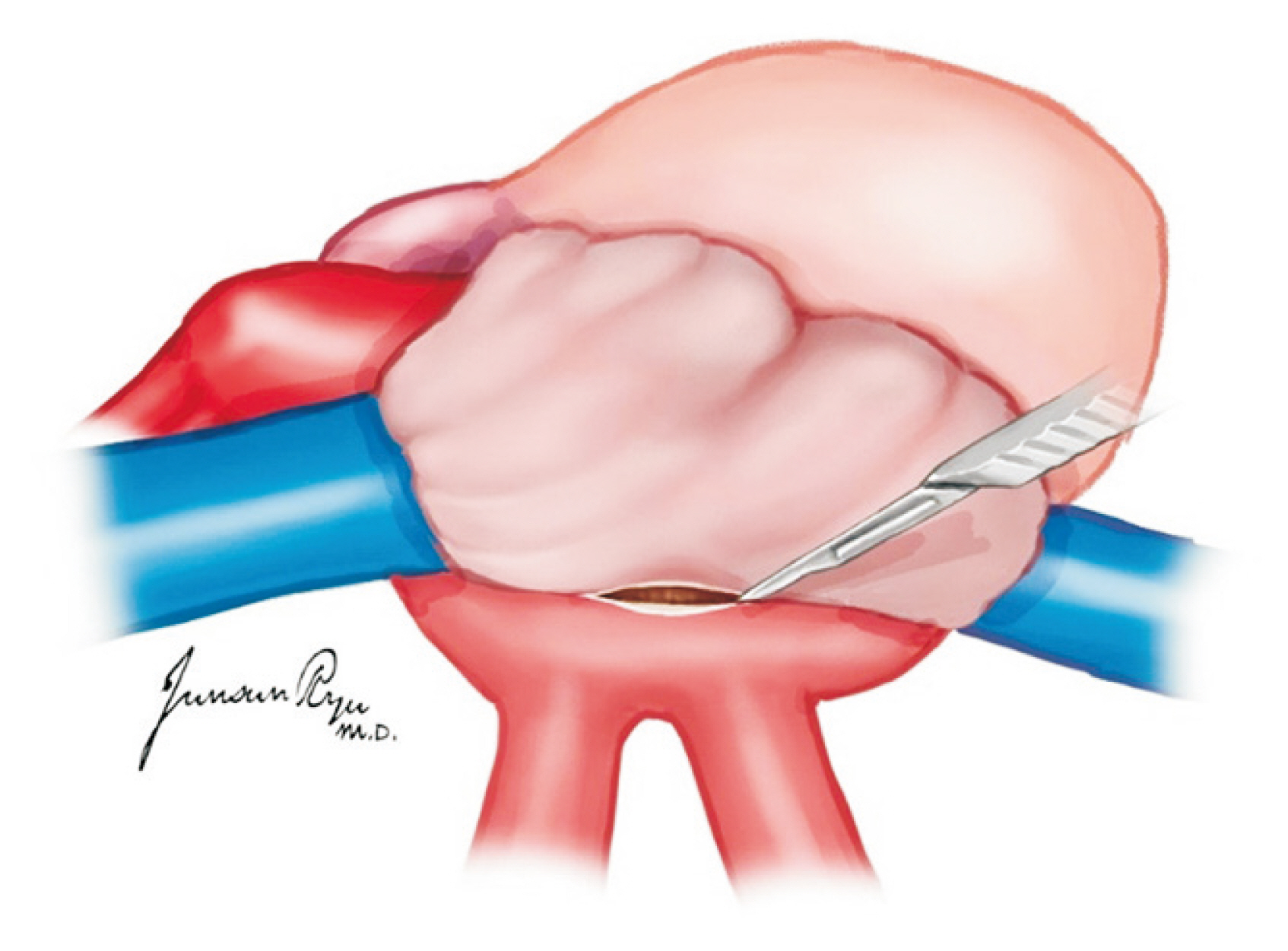
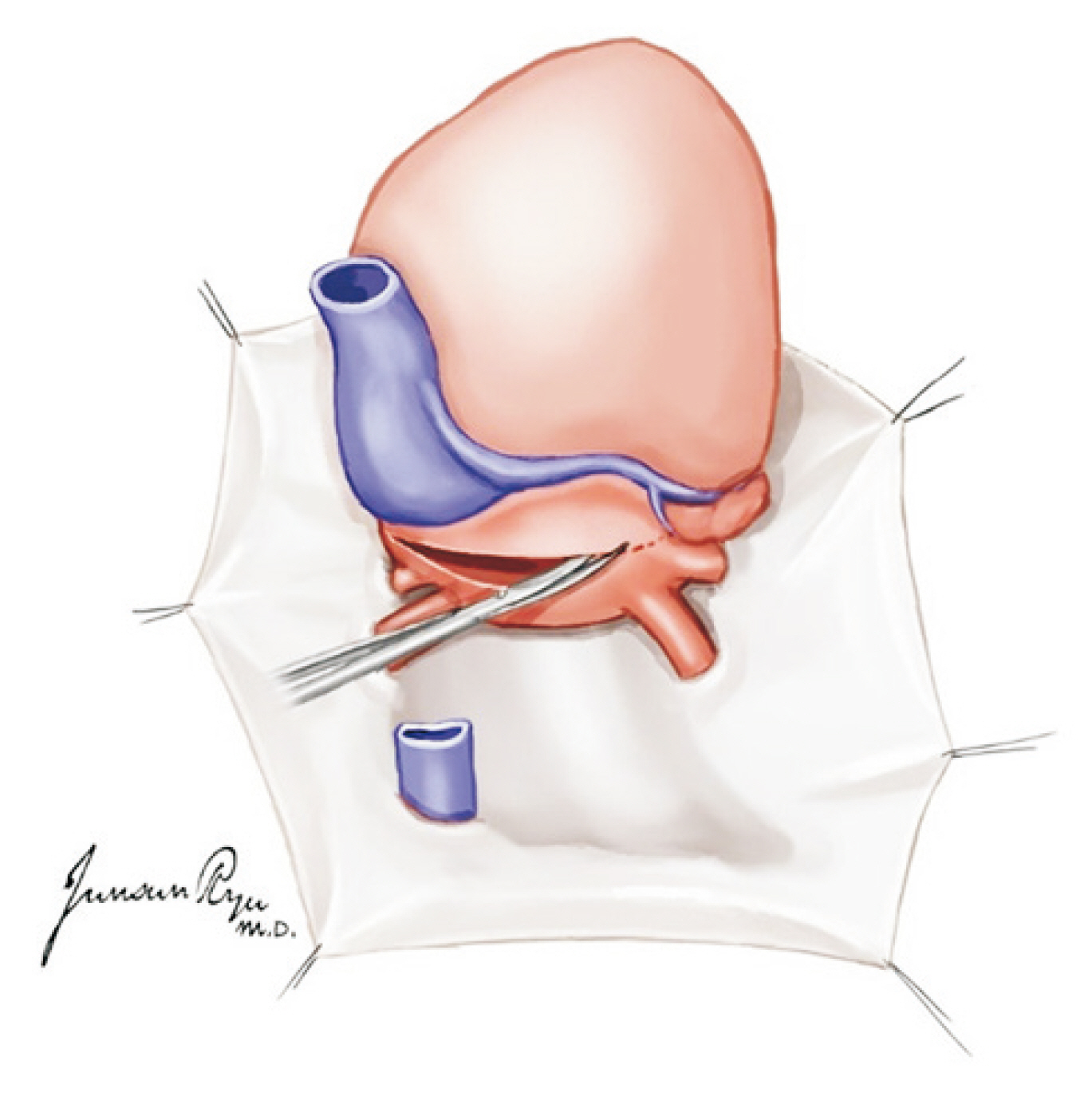
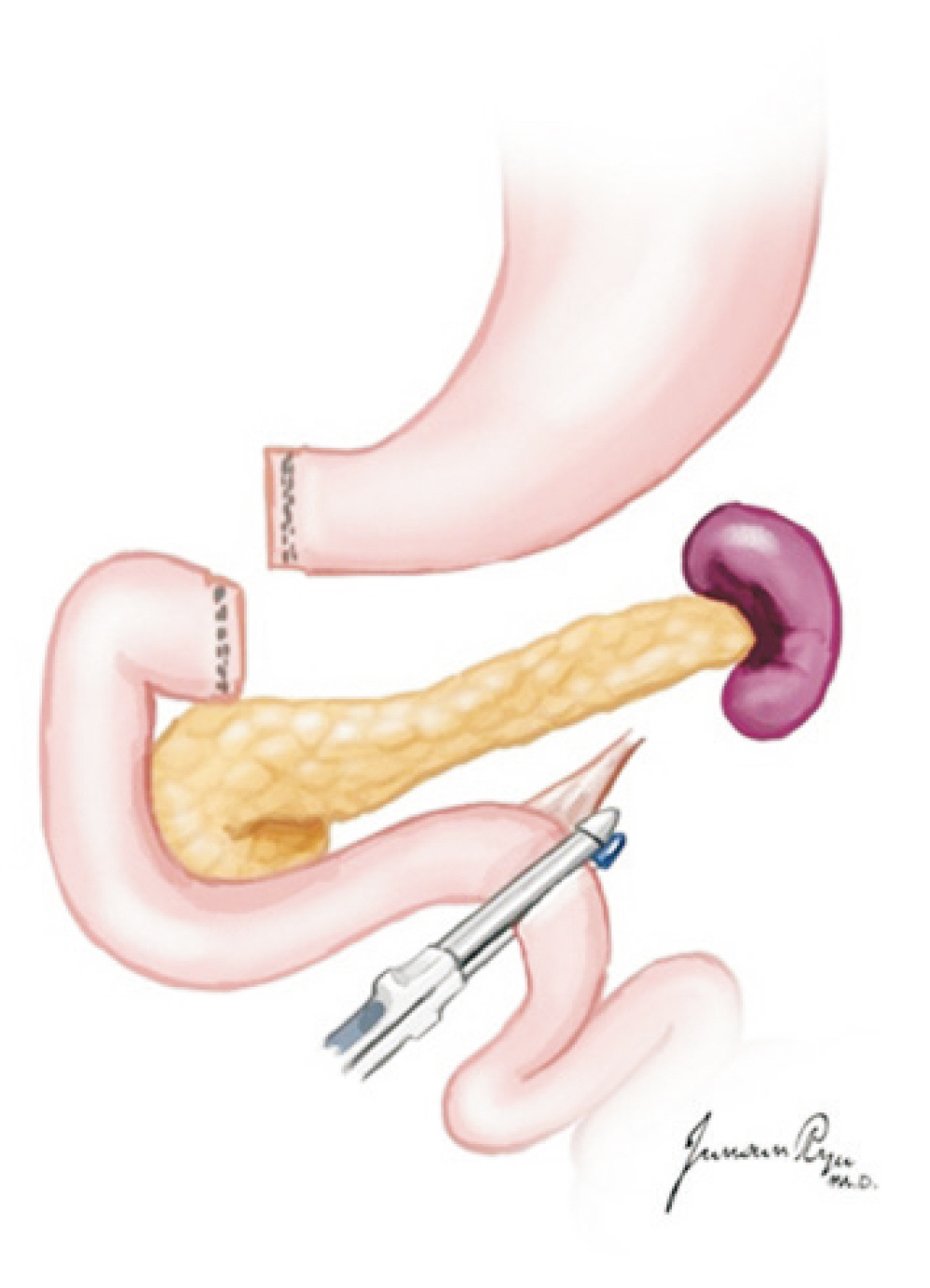
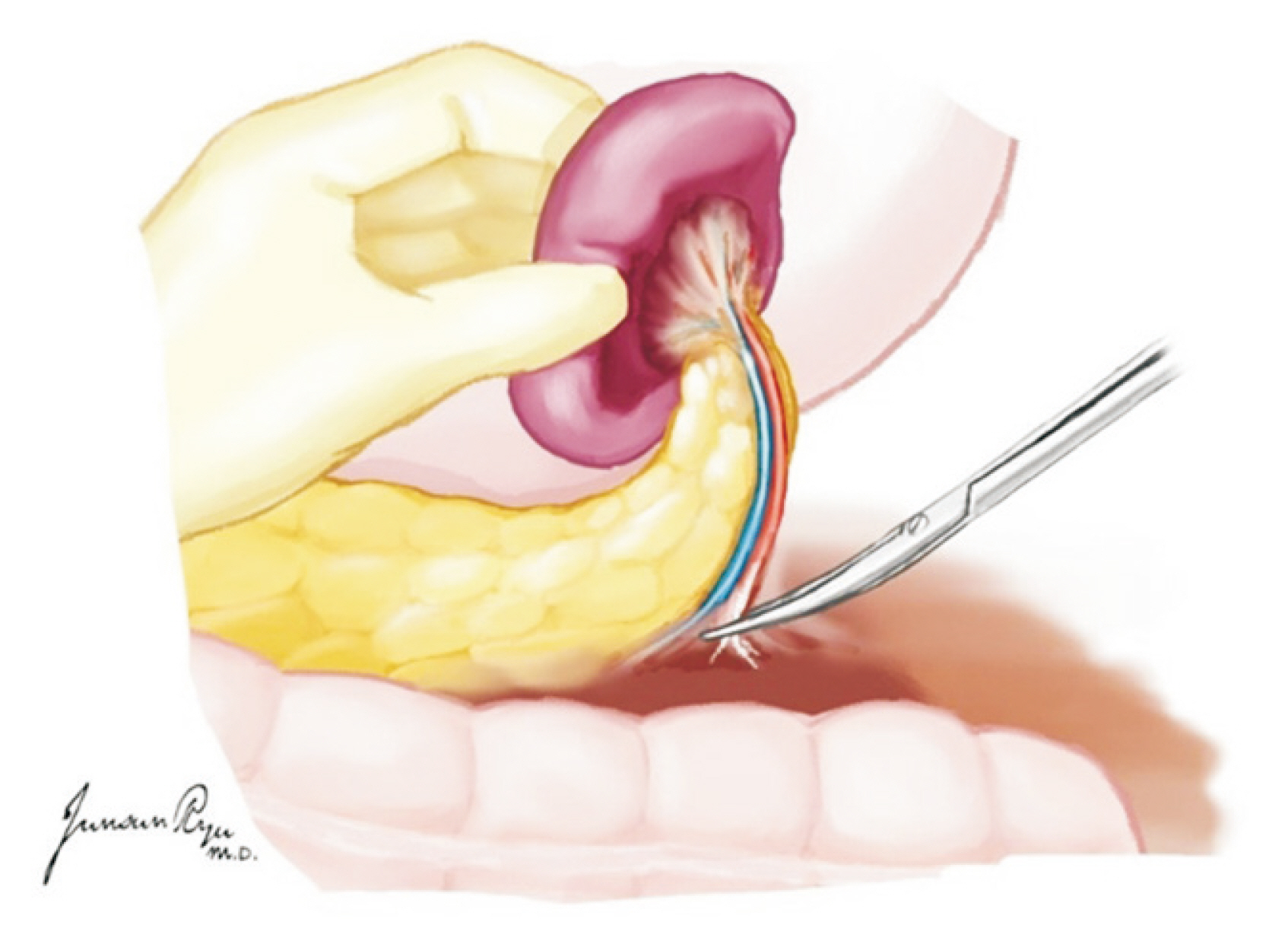
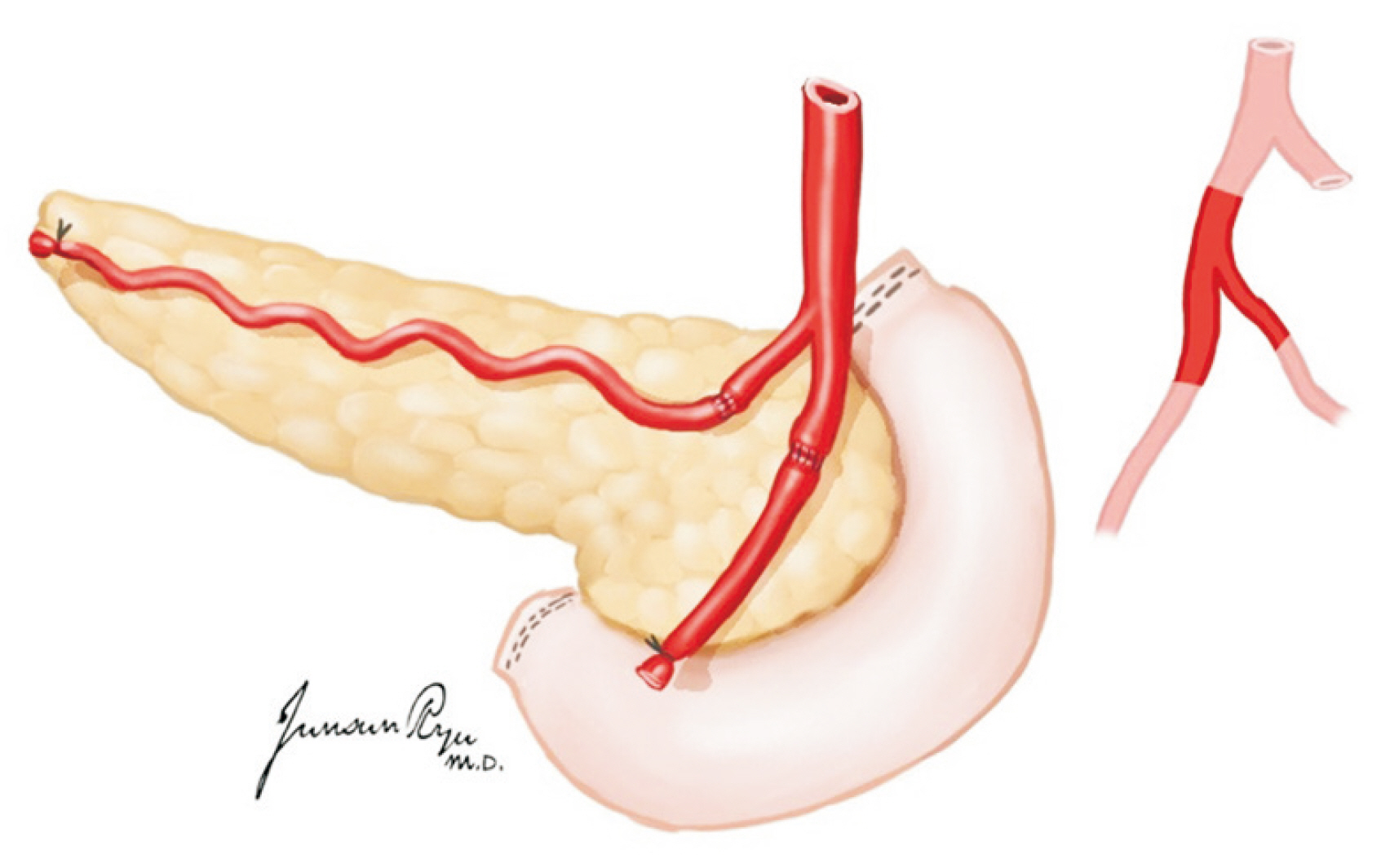
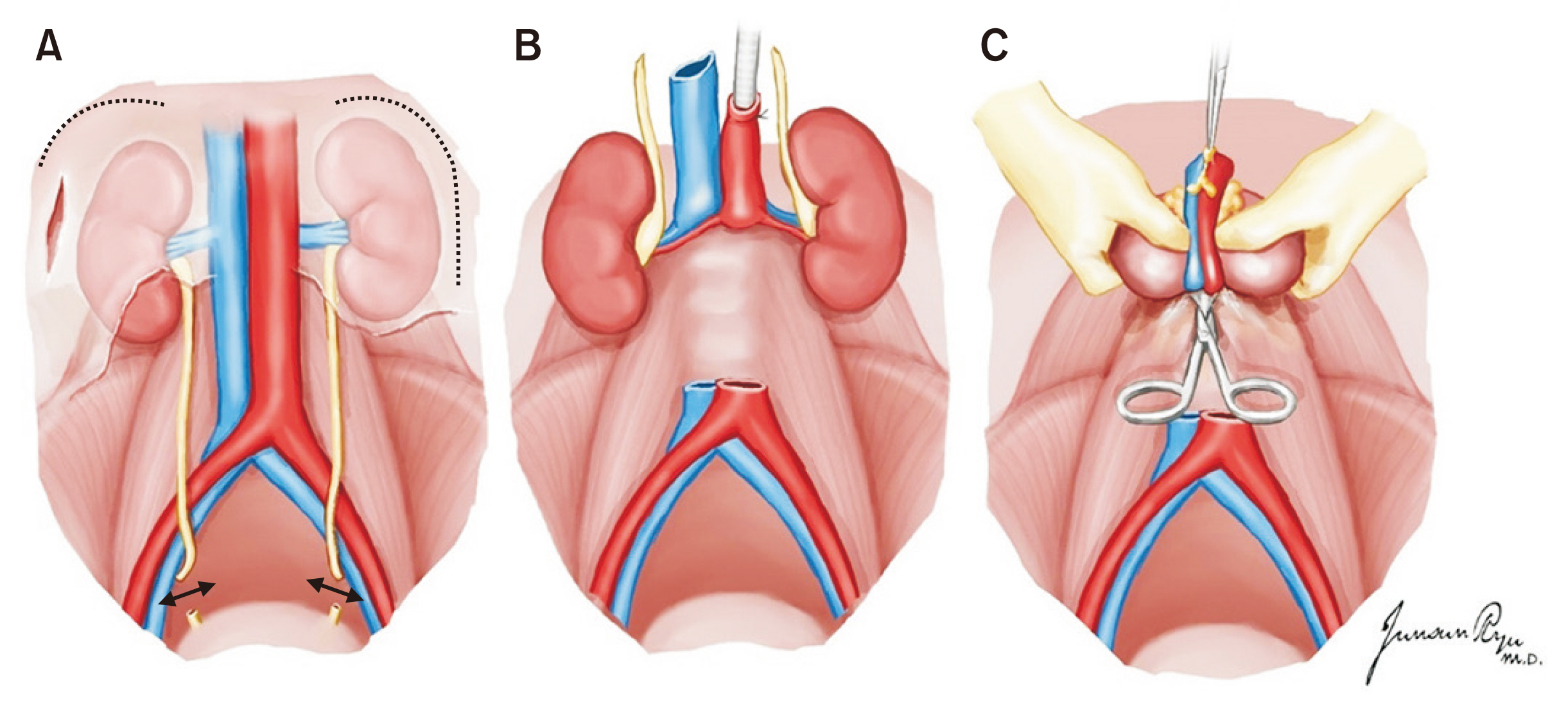
- With the increasing demand for organ transplantation, organ procurement from a deceased donor is an essential step for deceased donor organ transplantation. A proper surgical technique for the procurement of an organ graft from a deceased donor must be carried out to avoid any damage to it. Moreover, how to manage deceased donors until they enter the operating room in a stable condition is a critical point to be considered. The establishment of a surgical technique and preoperative management for organ procurement is encouraged to achieve a nationwide standard and consistency for organ graft sharing among the transplant units.
Keyword
Figure
Cited by 1 articles
-
Management of potential cardiac donors
Junho Hyun, Sang Eun Lee, Jae-Joong Kim
Clin Transplant Res. 2024;38(1):37-45. doi: 10.4285/ctr.23.0065.
Reference
-
1. Dare AJ, Bartlett AS, Fraser JF. 2012; Critical care of the potential organ donor. Curr Neurol Neurosci Rep. 12:456–65. DOI: 10.1007/s11910-012-0272-9. PMID: 22618126.
Article2. Patel MS, Abt PL. 2019; Current practices in deceased organ donor management. Curr Opin Organ Transplant. 24:343–50. DOI: 10.1097/MOT.0000000000000638. PMID: 31090647.
Article3. Souter MJ, Eidbo E, Findlay JY, Lebovitz DJ, Moguilevitch M, Neidlinger NA, et al. 2018; Organ donor management: part 1. toward a consensus to guide anesthesia services during donation after brain death. Semin Cardiothorac Vasc Anesth. 22:211–22. DOI: 10.1177/1089253217749053. PMID: 29276852.
Article4. van Erp AC, van Dullemen LF, Ploeg RJ, Leuvenink HG. 2018; Systematic review on the treatment of deceased organ donors. Transplant Rev (Orlando). 32:194–206. DOI: 10.1016/j.trre.2018.06.001. PMID: 30049604.
Article5. Chamorro-Jambrina C, Muñoz-Ramírez MR, Martínez- Melgar JL, Pérez-Cornejo MS. 2017; Organ donor management: eight common recommendations and actions that deserve reflection. Med Intensiva. 41:559–68. DOI: 10.1016/j.medin.2017.01.012. PMID: 28318674.
Article6. Chudoba P, Krajewski W, Wojciechowska J, Kamińska D. 2017; Brain death-associated pathological events and therapeutic options. Adv Clin Exp Med. 26:1457–64. DOI: 10.17219/acem/65068. PMID: 29442469.
Article7. Opdam HI. 2019; Hormonal therapy in organ donors. Crit Care Clin. 35:389–405. DOI: 10.1016/j.ccc.2018.11.013. PMID: 30784617.
Article8. Berthelsen PG, Marik PE. 2015; Therapeutic hypothermia in deceased organ donors and kidney-graft function. N Engl J Med. 373:2686. DOI: 10.1056/NEJMc1511744. PMID: 27186763.
Article9. Miñambres E, Pérez-Villares JM, Chico-Fernández M, Zabalegui A, Dueñas-Jurado JM, Misis M, et al. 2015; Lung donor treatment protocol in brain dead-donors: a multicenter study. J Heart Lung Transplant. 34:773–80. DOI: 10.1016/j.healun.2014.09.024. PMID: 25447580. PMCID: PMC6988327.
Article10. Nguyen DC, Loor G, Carrott P, Shafii A. 2019; Review of donor and recipient surgical procedures in lung transplantation. J Thorac Dis. 11(Suppl 14):S1810–6. DOI: 10.21037/jtd.2019.06.31. PMID: 31632758. PMCID: PMC6783720.
Article11. Inci I. 2017; Donors after cardiocirculatory death and lung transplantation. J Thorac Dis. 9:2660–9. DOI: 10.21037/jtd.2017.07.82. PMID: 28932573. PMCID: PMC5594200.
Article12. de Perrot M, Fischer S, Liu M, Jin R, Bai XH, Waddell TK, et al. 2001; Prostaglandin E1 protects lung transplants from ischemia-reperfusion injury: a shift from pro- to anti-inflammatory cytokines. Transplantation. 72:1505–12. DOI: 10.1097/00007890-200111150-00006. PMID: 11707737.13. Oto T, Rabinov M, Negri J, Marasco S, Rowland M, Pick A, et al. 2006; Techniques of reconstruction for inadequate donor left atrial cuff in lung transplantation. Ann Thorac Surg. 81:1199–204. DOI: 10.1016/j.athoracsur.2005.11.057. PMID: 16564243.
Article14. Slama A, Schillab L, Barta M, Benedek A, Mitterbauer A, Hoetzenecker K, et al. 2017; Standard donor lung procurement with normothermic ex vivo lung perfusion: a prospective randomized clinical trial. J Heart Lung Transplant. 36:744–53. DOI: 10.1016/j.healun.2017.02.011. PMID: 28314503.
Article15. Huddleston CB, Richey SR. 2014; Heart-lung transplantation. J Thorac Dis. 6:1150–8. DOI: 10.3109/9781420019285-5. PMID: 23456080.16. Yu HC, Cho BH. 2006; How to do I make an organ procurement in deceased donor? J Korean Soc Transplant. 20:14–24.17. Choi YR, Lee KW. 2015; Liver procurement. J Korean Soc Transplant. 29:109–17. DOI: 10.4285/jkstn.2015.29.3.109.
Article18. Keutgen XM, Petrowsky H. 2014; Procurement for visceral organ transplantation: where to cannulate and how to perfuse? Curr Opin Organ Transplant. 19:92–9. DOI: 10.1097/MOT.0000000000000066. PMID: 24565959.19. Makowka L, Stieber AC, Sher L, Kahn D, Mieles L, Bowman J, et al. 1988; Surgical technique of orthotopic liver transplantation. Gastroenterol Clin North Am. 17:33–51.
Article20. Nickkholgh A, Contin P, Abu-Elmagd K, Golriz M, Gotthardt D, Morath C, et al. 2013; Intestinal transplantation: review of operative techniques. Clin Transplant. 27 Suppl 25:56–65. DOI: 10.1111/ctr.12190. PMID: 23909503.
Article21. Wunderlich H, Brockmann JG, Voigt R, Rauchfuss F, Pascher A, Brose S, et al. 2011; DTG procurement guidelines in heart beating donors. Transpl Int. 24:733–57. DOI: 10.1111/j.1432-2277.2011.01266.x. PMID: 21668528.
Article22. Humar A, Payne WD, Matas AJ. 2006. Atlas of organ transplantation. Springer;London, UK: DOI: 10.1007/978-1-84628-316-1.23. Yersiz H, Renz JF, Hisatake GM, Gordon S, Saggi BH, Feduska NJ Jr, et al. 2003; Multivisceral and isolated intestinal procurement techniques. Liver Transpl. 9:881–6. DOI: 10.1053/jlts.2003.50155. PMID: 12884206. PMCID: PMC6445255.
Article24. Hakim NS SR, Gray D, Friend P, Colman A. 2010. Pancreas, islet and stem cell transplantation for diabetes. 2nd ed. Oxford University Press;Oxford, UK: DOI: 10.1093/med/9780199565863.001.0001.25. Yang HC, Gifford RR, Dafoe DC, Neumyer MM, Thiele BL. 1991; Arterial reconstruction of the pancreatic allograft for transplantation. Am J Surg. 162:262–4. DOI: 10.1016/0002-9610(91)90083-P. PMID: 1928589.
Article26. Morris PJ, Tilney NL, editors. PM. 1984. Techniques of multiple organ harvesting. Progress in transplantation. Edinburgh. Churchill Livingstone;burgh, UK:27. Knechtle S, Morris P. 2008. Kidney transplantation. 6th ed. Saunders Elsevier;Philadelphia, PA:
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Activation Policy for Brain-dead Organ Donation
- Optimal System for Deceased Organ Donation and Procurement in Korea
- How to Do I Make an Organ Procurement in Deceased Donor?
- Current Status of Deceased Donor Organ Recovery and Sharing in Korea
- Donor Selection, Management, and Procurement for Lung Transplantation