J Cerebrovasc Endovasc Neurosurg.
2020 Sep;22(3):141-155. 10.7461/jcen.2020.22.3.141.
Role of microsurgery for treatment of posterior circulation aneurysms in the endovascular era
- Affiliations
-
- 1Department of Neurosurgery, Asan Medical Center, University of Ulsan, College of Medicine, Seoul, Korea
- 2Department of Radiology, Asan Medical Center, University of Ulsan, College of Medicine, Seoul, Korea
- 3Department of Neurosurgery, Kyunghee University School of Medicine, Seoul, Korea
- KMID: 2506761
- DOI: http://doi.org/10.7461/jcen.2020.22.3.141
Abstract
Objective
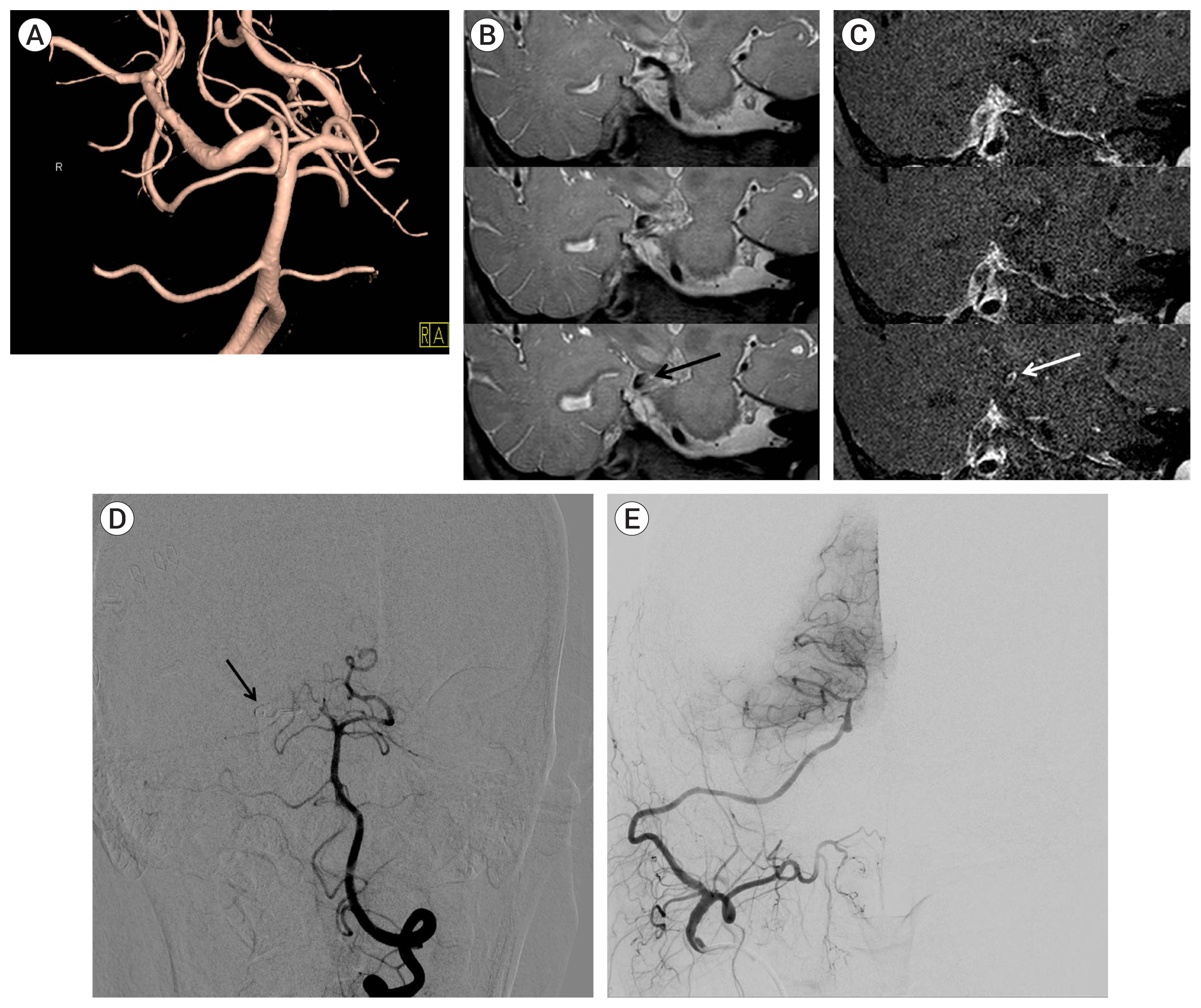
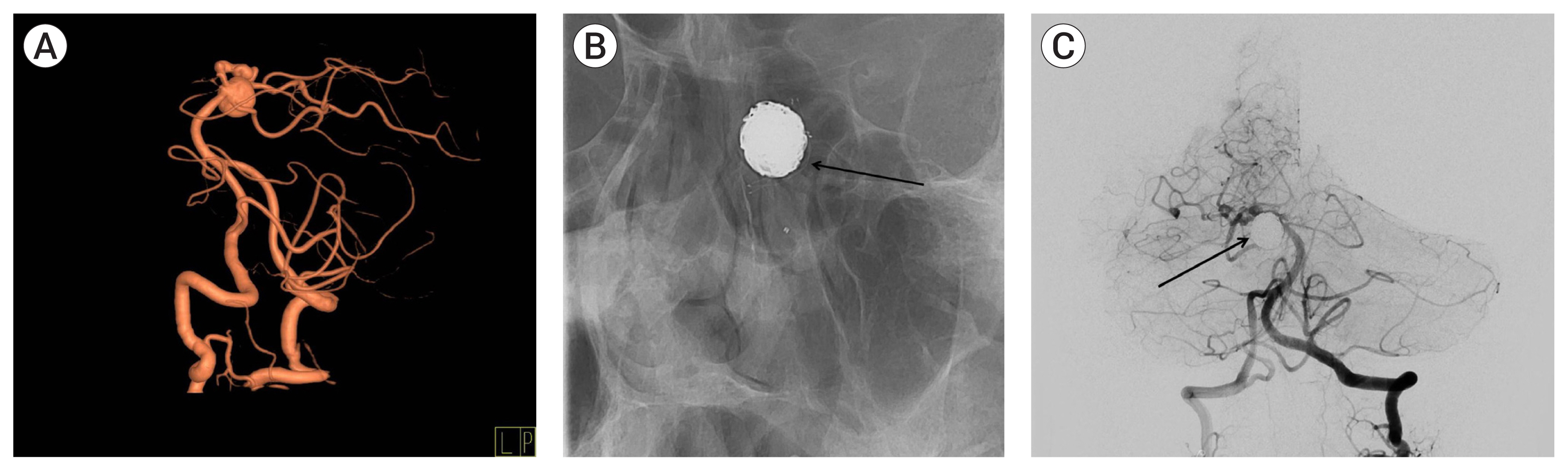
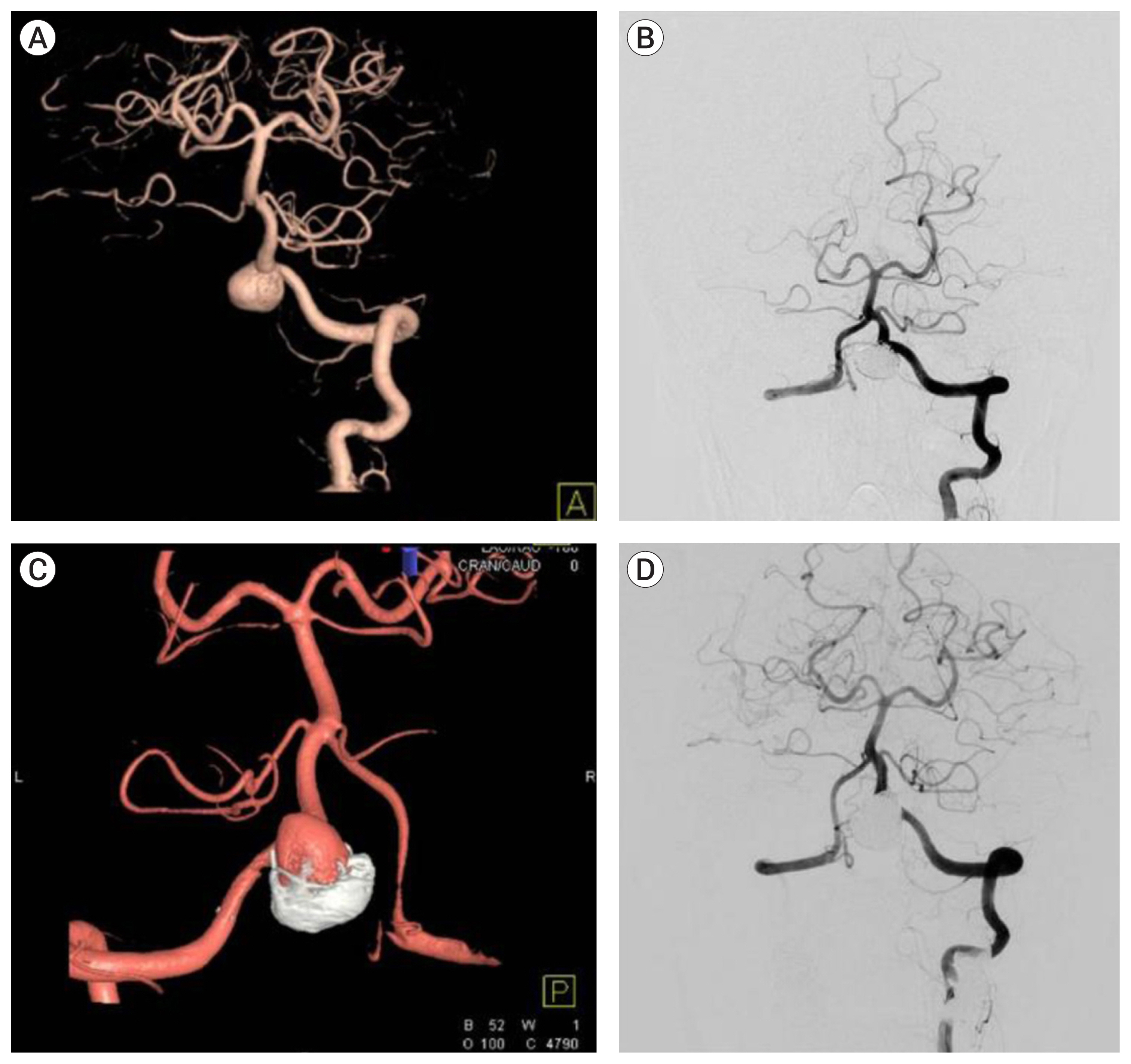
Several studies have reported that the outcomes of endovascular treatment were superior to those of microsurgical treatment for posterior circulation aneurysms. Thus, this study compared outcomes of endovascular and microsurgical treatment for posterior circulation aneurysms and assess the usefulness of microsurgery in these patients.
Methods
Outcomes were retrospectively evaluated after endovascular and microsurgical treatment of 621 posterior circulation aneurysms. The 621 aneurysms included 187 treated by surgical clipping and 434 treated by endovascular coiling.
Results
In patients with unruptured aneurysms the rates of residual lesions and retreatment were significantly lower in those who underwent microsurgical than endovascular treatment. However immediate postoperative and 6 month follow-up Glasgow outcome scale (GOS) scores did not differ significantly in the two groups. In patients with ruptured aneurysms, the rates of residual lesions and retreatment were significantly lower in the microsurgery than in the endovascular treatment group. Even so immediate postoperative and 6 month follow-up GOS scores did not differ significantly in the two groups.
Conclusions
Endovascular treatment has increasingly become an alternative modality for microsurgery in posterior circulation aneurysm, whereas the indication for microsurgery is greatly reduced. However, the absolute number of microsurgery is maintained showing that it is a still valuable technique, as advances in endovascular or stent-assisted coiling have not solved many of the challenges inherent in the management of complex aneurysms. Hence, the advantages and limitations of both modalities must be carefully concerned in posterior circulation aneurysm to obtain favorable outcome.
Keyword
Figure
Reference
-
1. Al-Khayat H, Al-Khayat H, White J, Manner D, Samson D. Upper basilar artery aneurysms: oculomotor outcomes in 163 cases. J Neurosurg. 2005; Mar. 102(3):482–8.
Article2. Al-Khayat H, Al-Khayat H, White J, Manner D, Samson D. Upper basilar artery aneurysms: oculomotor outcomes in 163 cases. J Neurosurg. 2005; Mar. 102(3):482–8.
Article3. Bebawy JF, Gupta DK, Bendok BR, Hemmer LB, Zeeni C, Avram MJ, et al. Adenosine-induced flow arrest to facilitate intracranial aneurysm clip ligation: dose-response data and safety profile. Anesth Analg. 2010; May. 110(5):1406–11.4. Bendok BR, Gupta DK, Rahme RJ, Eddleman CS, Adel JG, Sherma AK, et al. Adenosine for temporary flow arrest during intracranial aneurysm surgery: a single-center retrospective review. Neurosurgery. 2011; Oct. 69(4):815–20. discussion 820–1.
Article5. Bijlenga P, Ebeling C, Jaegersberg M, Summers P, Rogers A, Waterworth A, et al. Risk of rupture of small anterior communicating artery aneurysms is similar to posterior circulation aneurysms. Stroke. 2013; Nov. 44(11):3018–26.
Article6. Binh NT, Luu VD, Thong PM, Cuong NN, Anh NQ, Tuan TA, et al. Flow diverter stent for treatment of cerebral aneurysms: a report of 130 patients with 134 aneurysms. Heliyon. 2020; Feb. 6(2):e03356.
Article7. Briganti F, Leone G, Marseglia M, Mariniello G, Caranci F, Brunetti A, et al. Endovascular treatment of cerebral aneurysms using flow-diverter devices: a systematic review. Neuroradiol J. 2015; Aug. 28(4):365–75.
Article8. Day JD, Fukushima T, Giannotta SL. Cranial base approaches to posterior circulation aneurysms. J Neurosurg. 1997; Oct. 87(4):544–54.
Article9. Groff MW, Adams DC, Kahn RA, Kumbar UM, Yang BY, Bederson JB. Adenosine-induced transient asystole for management of a basilar artery aneurysm. Case report. J Neurosurg. 1999; Oct. 91(4):687–90.10. Horikoshi T, Nukui H, Yagishita T, Nishigaya K, Fukasawa I, Sasaki H. Oculomotor nerve palsy after surgery for upper basilar artery aneurysms. Neurosurgery. 1999; Apr. 44(4):705–10. discussion 710–1.
Article11. International Study of Unruptured Intracranial Aneurysms Investigators. Unruptured intracranial aneurysms — risk of rupture and risks of surgical intervention. N Engl J Med. 1998; Dec. 339(24):1725–33.12. Jamieson KG. Aneurysms of the vertebrobasilar system; surgical intervention in 19 cases. J Neurosurg. 1964; Sep. 21:781–97.13. Johnston SC, Dowd CF, Higashida RT, Lawton MT, Duckwiler GR, Gress DR, et al. Predictors of rehemorrhage after treatment of ruptured intracranial aneurysms: the Cerebral Aneurysm Rerupture After Treatment (CARAT) study. Stroke. 2008; Jan. 39(1):120–5.14. Kiyofuji S, Graffeo CS, Perry A, Murad MH, Flemming KD, Lanzino G, et al. Meta-analysis of treatment outcomes of posterior circulation non-saccular aneurysms by flow diverters. J Neurointerv Surg. 2018; May. 10(5):493–9.
Article15. Klemenc-Ketis Z, Bacovnik-Jansa U, Ogorevc M, Kersnik J. Outcome predictors of Glasgow Outcome Scale score in patients with severe traumatic brain injury. Ulus Travma Acil Cerrahi Derg. 2011; Nov. 17(6):509–15.
Article16. Krisht AF, Krayenbuhl N, Sercl D, Bikmaz K, Kadri PA. Results of microsurgical clipping of 50 high complexity basilar apex aneurysms. Neurosurgery. 2007; Feb. 60(2):242–50. discussion 250–2.17. Lanzino G, Murad MH, d’Urso PI, Rabinstein AA. Coil embolization versus clipping for ruptured intracranial aneurysms: a meta-analysis of prospective controlled published studies. AJNR Am J Neuroradiol. 2013; Sep. 34(9):1764–8.
Article18. Lee SH, Kwun BD, Kim JU, Choi JH, Ahn JS, Park W, et al. Adenosine-induced transient asystole during intracranial aneurysm surgery: indications, dosing, efficacy, and risks. Acta Neurochir (Wien). 2015; Nov. 157(11):1879–86. discussion 1886.
Article19. Lv X, Yang H, Liu P, Li Y. Flow-diverter devices in the treatment of intracranial aneurysms: a meta-analysis and systematic review. Neuroradiol J. 2016; Feb. 29(1):66–71.
Article20. Maus V, Mpotsaris A, Dorn F, Mohlenbruch M, Borggrefe J, Stavrinou P, et al. The use of flow diverter in ruptured, dissecting intracranial aneurysms of the posterior circulation. World Neurosurg. 2018; Mar. 111:e424–33.
Article21. McDougall CG, Spetzler RF, Zabramski JM, Partovi S, Hills NK, Nakaji P, et al. The barrow ruptured aneurysm trial. J Neurosurg. 2012; Jan. 116(1):135–44.
Article22. McMillan T, Wilson L, Ponsford J, Levin H, Teasdale G, Bond M. The Glasgow Outcome Scale - 40 years of application and refinement. Nat Rev Neurol. 2016; Aug. 12(8):477–85.
Article23. Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, et al. International Subarachnoid Aneurysm Trial (ISAT) Collaborative Group. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomized trial. J Stroke Cerebrovasc Dis. 2002; Nov–Dec. 11(6):304–14.
Article24. Munich SA, Cress MC, Rangel-Castilla L, Sonig A, Ogilvy CS, Lanzino G, et al. Neck remnants and the risk of aneurysm rupture after endovascular treatment with coiling or stent-assisted coiling: much ado about nothing? Neurosurgery. 2019; Feb. 84(2):421–7.
Article25. Nair P, Panikar D, Nair AP, Sundar S, Ayiramuthu P, Thomas A. Microsurgical management of aneurysms of the superior cerebellar artery - lessons learnt: An experience of 14 consecutive cases and review of the literature. Asian J Neurosurg. 2015; Jan–Mar. 10(1):47.
Article26. Pandey AS, Koebbe C, Rosenwasser RH, Veznedaroglu E. Endovascular coil embolization of ruptured and unruptured posterior circulation aneurysms: review of a 10-year experience. Neurosurgery. 2007; Apr. 60(4):626–36. discussion 636–7.27. Park W, Kwon DH, Ahn JS, Lee SH, Park JC, Kwun BD. Treatment strategies for dissecting aneurysms of the posterior cerebral artery. Acta Neurochir (Wien). 2015; Oct. 157(10):1633–43.
Article28. Raymond J, Guilbert F, Weill A, Georganos SA, Juravsky L, Lambert A, et al. Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils. Stroke. 2003; Jun. 34(6):1398–403.
Article29. Ries T, Siemonsen S, Thomalla G, Grzyska U, Zeumer H, Fiehler J. Long-term follow-up of cerebral aneurysms after endovascular therapy prediction and outcome of retreatment. AJNR Am J Neuroradiol. 2007; Oct. 28(9):1755–61.
Article30. Rinkel GJ, Djibuti M, Algra A, van Gijn J. Prevalence and risk of rupture of intracranial aneurysms: a systematic review. Stroke. 1998; Jan. 29(1):251–6.31. Rodríguez-Hernández A, Walcott BP, Birk H, Lawton MT. The superior cerebellar artery aneurysm: a posterior circulation aneurysm with favorable microsurgical outcomes. Neurosurgery. 2017; Jun. 80(6):908–16.
Article32. Sanai N, Tarapore P, Lee AC, Lawton MT. The current role of microsurgery for posterior circulation aneurysms: a selective approach in the endovascular era. Neurosurgery. 2008; Jun. 62(6):1236–49. discussion 1249–53.33. Solomon RA. Principles of aneurysm surgery: cerebral ischemic protection, hypothermia, and circulatory arrest. Clin Neurosurg. 1994; Jan. 41:351–63.34. Spetzler RF, McDougall CG, Albuquerque FC, Zabramski JM, Hills NK, Partovi S, et al. The barrow ruptured aneurysm trial: 3-year results. J Neurosurg. 2013; Jul. 119(1):146–57.
Article35. Spetzler RF, McDougall CG, Zabramski JM, Albuquerque FC, Hills NK, Russin JJ, et al. The barrow ruptured aneurysm trial: 6-year results. J Neurosurg. 2015; Sep. 123(3):609–17.
Article36. Straus DC, Brito da Silva H, McGrath L, Levitt MR, Kim LJ, Ghodke BV, et al. Cerebral revascularization for aneurysms in the flow-diverter era. Neurosurgery. 2017; May. 80(5):759–68.
Article37. Taki W, Sakai N, Suzuki H. Prospective Registry of Subarachnoid Aneurysms Treatment (PRESAT) group. Importance of independent evaluation of initial anatomic results after endovascular coiling for ruptured cerebral aneurysms. J Clin Neurosci. 2013; Apr. 20(4):527–31.
Article38. Taki W, Sakai N, Suzuki H. Prospective Registry of Subarachnoid Aneurysms Treatment (PRESAT) group. Importance of independent evaluation of initial anatomic results after endovascular coiling for ruptured cerebral aneurysms. J Clin Neurosci. 2013; Apr. 20(4):527–31.
Article39. Toccaceli G, Diana F, Cagnazzo F, Cannizzaro D, Lanzino G, Barbagallo GMV, et al. Microsurgical clipping compared with new and most advanced endovascular techniques in the treatment of unruptured middle cerebral artery aneurysms: a meta-analysis in the modern era. World Neurosurg. 2020; May. 137:451–64.e1.
Article40. Wang CB, Shi WW, Zhang GX, Lu HC, Ma J. Flow diverter treatment of posterior circulation aneurysms. A meta-analysis. Neuroradiology. 2016; Apr. 58(4):391–400.
Article41. Wermer MJ, van der Schaaf IC, Algra A, Rinkel GJ. Risk of rupture of unruptured intracranial aneurysms in relation to patient and aneurysm characteristics: an updated meta-analysis. Stroke. 2007; Apr. 38(4):1404–10.42. Wiebers DO, Whisnant JP, Huston J 3rd, Meissner I, Brown RD Jr, Piepgras DG, et al. Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 2003; Jul. 362(9378):103–10.
Article43. Young WL, Lawton MT, Gupta DK, Hashimoto T. Anesthetic management of deep hypothermic circulatory arrest for cerebral aneurysm clipping. Anesthesiology. 2002; Feb. 96(2):497–503.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of the Posterior Circulation Aneurysms
- Seven Intracranial Aneurysms in One Patient: Treatment and Review of Literature
- Endovascular Treatment of Posterior Circulation Aneurysms
- The Role of Neurosurgeons in the Era of Intra-Aneurysmal Treatment
- Microsurgical Strategies Following Failed Endovascular Treatment with the Pipeline Embolization Device: Case of a Giant Posterior Cerebral Artery Aneurysm