Ann Surg Treat Res.
2020 Oct;99(4):230-237. 10.4174/astr.2020.99.4.230.
Xanthogranulomatous cholecystitis: a rare gallbladder pathology from a single-center perspective
- Affiliations
-
- 1Department of General Surgery, Faculty of Medicine, Cukurova University, Adana, Turkey
- 2Department of Surgical Oncology, Faculty of Medicine, Cukurova University, Adana, Turkey
- KMID: 2506654
- DOI: http://doi.org/10.4174/astr.2020.99.4.230
Abstract
- Purpose
The aim of this study was to review patients with xanthogranulomatous cholecystitis (XGC).
Methods
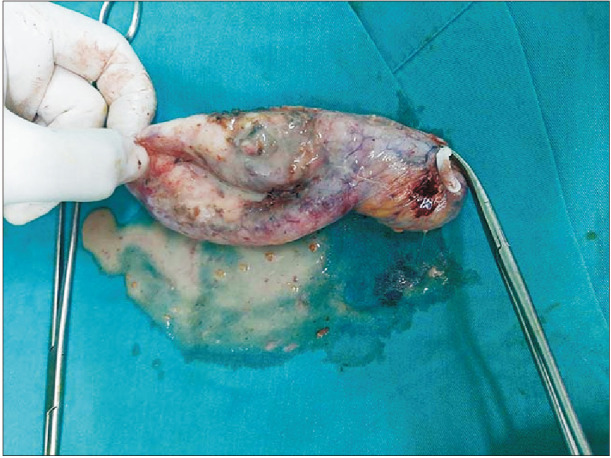
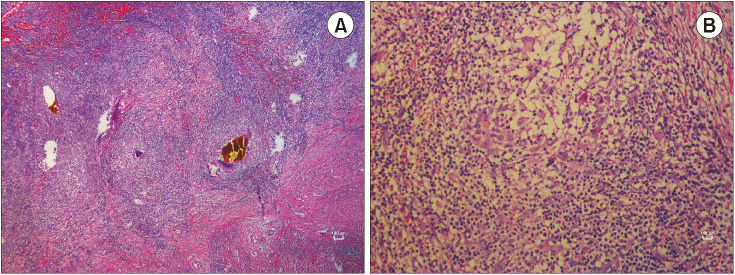
A total of 79 patients diagnosed with XGC were included in the study. The criteria for XGC in the pathology specimens were the presence of histiocytes, cholesterol deposits, lipids, and focal or widespread wall enlargement.
Results
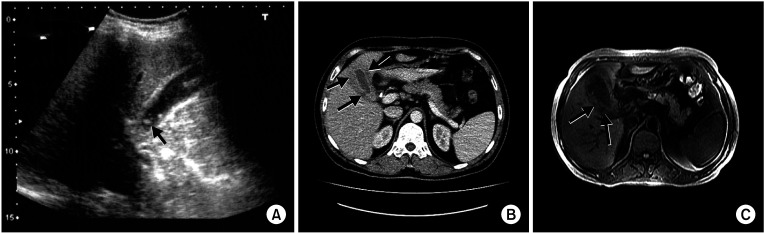
Patients were diagnosed with XGC, of which 52 (65.8%) were male and 27 (34.2%) were female, creating a male-to-female ratio of 2:1. The mean age was 65.8 ± 14.3 years (range, 36–97 years). The most common presenting symptom was abdominal pain (63.3%), and the least common presenting symptom was jaundice (8.9%). Of the total, 25 patients were found to have pathological conditions with the potential to obstruct the bile duct or to slow bile flow. A frozen section examination was performed on 20 patients due to suspicion of a tumor by intraoperative macroscopic examination. However, no malignancy was detected in the cases who underwent a frozen section examination. An increase in wall thickness of the gallbladder was observed in 81.6% (n = 31) of the patients on computed tomography scans and in 81.8% (n = 18) of the patients on magnetic resonance imaging scans in which possible tumor lesions were reported, but no tumor was detected.
Conclusion
It is difficult to diagnose XGC either preoperatively or intraoperatively, and further imaging methods are needed in the preoperative period other than ultrasonography. However, a definitive diagnosis depends exclusively on pathologic examination.
Keyword
Figure
Reference
-
1. Christensen AH, Ishak KG. Benign tumors and pseudotumors of the gallbladder. Report of 180 cases. Arch Pathol. 1970; 90:423–432. PMID: 4319984.2. Goodman ZD, Ishak KG. Xanthogranulomatous cholecystitis. Am J Surg Pathol. 1981; 5:653–659. PMID: 7337158.3. Yang T, Zhang BH, Zhang J, Zhang YJ, Jiang XQ, Wu MC. Surgical treatment of xanthogranulomatous cholecystitis: experience in 33 cases. Hepatobiliary Pancreat Dis Int. 2007; 6:504–508. PMID: 17897914.4. Sharma D, Babu R, Sood G, Kapoor G, Solanki RS, Thomas S. Xanthogranulomatous cholecystitis masquerading as malignancy with liver metastasis. ANZ J Surg. 2009; 79:946–947. PMID: 20003001.5. Goshima S, Chang S, Wang JH, Kanematsu M, Bae KT, Federle MP. Xanthogranulomatous cholecystitis: diagnostic performance of CT to differentiate from gallbladder cancer. Eur J Radiol. 2010; 74:e79–e83. PMID: 19446416.6. Zhao F, Lu PX, Yan SX, Wang GF, Yuan J, Zhang SZ, et al. CT and MR features of xanthogranulomatous cholecystitis: an analysis of consecutive 49 cases. Eur J Radiol. 2013; 82:1391–1397. PMID: 23726123.7. Levy AD, Murakata LA, Abbott RM, Rohrmann CA Jr. From the archives of the AFIP. Benign tumors and tumorlike lesions of the gallbladder and extrahepatic bile ducts: radiologic-pathologic correlation. Armed Forces Institute of Pathology. Radiographics. 2002; 22:387–413. PMID: 11896229.8. Casas D, Pérez-Andrés R, Jiménez JA, Mariscal A, Cuadras P, Salas M, et al. Xanthogranulomatous cholecystitis: a radiological study of 12 cases and a review of the literature. Abdom Imaging. 1996; 21:456–460. PMID: 8832871.9. Wang M, Zhang T, Zang L, Lu A, Mao Z, Li J, et al. Surgical treatment for xanthogranulomatous cholecystitis: a report of 74 cases. Surg Laparosc Endosc Percutan Tech. 2009; 19:231–233. PMID: 19542852.10. Guzmán-Valdivia G. Xanthogranulomatous cholecystitis: 15 years' experience. World J Surg. 2004; 28:254–257. PMID: 14961199.11. Fligiel S, Lewin KJ. Xanthogranulomatous cholecystitis: case report and review of the literature. Arch Pathol Lab Med. 1982; 106:302–304. PMID: 6896437.12. Solanki RL, Arora HL, Gaur SK, Anand VK, Gupta R. Xanthogranulomatous cholecystitis (XGC): a clinicopathological study of 21 cases. Indian J Pathol Microbiol. 1989; 32:256–260. PMID: 2632411.13. Han SH, Chen YL. Diagnosis and treatment of xanthogranulomatous cholecystitis: a report of 39 cases. Cell Biochem Biophys. 2012; 64:131–135. PMID: 22707297.14. Park JW, Kim KH, Kim SJ, Lee SK. Xanthogranulomatous cholecystitis: is an initial laparoscopic approach feasible? Surg Endosc. 2017; 31:5289–5294. PMID: 28593410.15. Kawana T, Suita S, Arima T, Hirayama Y, Ishii K, Minamishima I, et al. Xanthogranulomatous cholecystitis in an infant with obstructive jaundice. Eur J Pediatr. 1990; 149:765–767. PMID: 2121491.16. Kim H, Cho Y, Park J. Xanthogranulomatous cholecystitis not associated with gallstone in a 9-year-old girl. J Korean Surg Soc. 2009; 77:72–74.17. Goldar-Najafi A, Khettry U. Xanthogranulomatous choledochitis: a previously undescribed mass lesion of the hepatobiliary and ampullary region. Semin Liver Dis. 2003; 23:101–106. PMID: 12616455.18. Krishnani N, Shukla S, Jain M, Pandey R, Gupta RK. Fine needle aspiration cytology in xanthogranulomatous cholecystitis, gallbladder adenocarcinoma and coexistent lesions. Acta Cytol. 2000; 44:508–514. PMID: 10934941.19. Kocaöz S, Turan G. Preneoplastic and neoplastic gallbladder lesions detected after cholecystectomy. Prz Gastroenterol. 2019; 14:193–197. PMID: 31649791.20. Hale MD, Roberts KJ, Hodson J, Scott N, Sheridan M, Toogood GJ. Xanthogranulomatous cholecystitis: a European and global perspective. HPB (Oxford). 2014; 16:448–458. PMID: 23991684.21. Misra S, Chaturvedi A, Misra NC, Sharma ID. Carcinoma of the gallbladder. Lancet Oncol. 2003; 4:167–176. PMID: 12623362.22. Strom BL, Maislin G, West SL, Atkinson B, Herlyn M, Saul S, et al. Serum CEA and CA 19-9: potential future diagnostic or screening tests for gallbladder cancer? Int J Cancer. 1990; 45:821–824. PMID: 2335386.23. Chang BJ, Kim SH, Park HY, Lim SW, Kim J, Lee KH, et al. Distinguishing xanthogranulomatous cholecystitis from the wall-thickening type of early-stage gallbladder cancer. Gut Liver. 2010; 4:518–523. PMID: 21253302.24. Uchiyama K, Ozawa S, Ueno M, Hayami S, Hirono S, Ina S, et al. Xanthogranulomatous cholecystitis: the use of preoperative CT findings to differentiate it from gallbladder carcinoma. J Hepatobiliary Pancreat Surg. 2009; 16:333–338. PMID: 19280109.25. Zhang F, Chen W, Zhang L, Hou C, Zhang M. Usefulness of ultrasound in differentiating xanthogranulomatous cholecystitis from gallbladder carcinoma. Ultrasound Med Biol. 2019; 45:2925–2931. PMID: 31447238.26. Kang TW, Kim SH, Park HJ, Lim S, Jang KM, Choi D, et al. Differentiating xanthogranulomatous cholecystitis from wall-thickening type of gallbladder cancer: added value of diffusion-weighted MRI. Clin Radiol. 2013; 68:992–1001. PMID: 23622795.27. Lee ES, Kim JH, Joo I, Lee JY, Han JK, Choi BI. Xanthogranulomatous cholecystitis: diagnostic performance of US, CT, and MRI for differentiation from gallbladder carcinoma. Abdom Imaging. 2015; 40:2281–2292. PMID: 25952571.28. Seo SH, Park JI, Kim JS, Kim KH, Choi CS, Choi YK. Xanthogranulomatous cholecystitis: a retrospective analysis of 36 cases. J Korean Surg Soc. 2009; 76:371–377.29. Kim JH, Jeong IH, Yoo BM, Kim JH, Kim MW, Kim WH. Is xanthogranulomatous cholecystitis the most difficult for laparoscopic cholecystectomy? Hepatogastroenterology. 2009; 56:597–601. PMID: 19621662.30. Benbow EW. Xanthogranulomatous cholecystitis. Br J Surg. 1990; 77:255–256. PMID: 2182176.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Xanthogranulomatous cholecystitis
- A Case of Xanthogranulomatous Cholecystitis
- A Case of Xanthogranulomatous Cholecystitis Decreased in Size after Steroid Treatment and Avoided Extended Resection
- Xanthogranulomatous Cholecystitis Not Associated with Gallstone in a 9-year-old Girl
- Xanthogranulomatous Cholecystitis Mimicking Gallbladder Cancer