Ann Surg Treat Res.
2020 Oct;99(4):205-212. 10.4174/astr.2020.99.4.205.
Reduced fasting time in patients who underwent totally laparoscopic distal gastrectomy
- Affiliations
-
- 1Department of Surgery, Pusan National University Yangsan Hospital, Yangsan, Korea
- 2Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea
- KMID: 2506651
- DOI: http://doi.org/10.4174/astr.2020.99.4.205
Abstract
- Purpose
The aim of this study was to analyze the effects of reduced fasting time on postoperative recovery in patients who underwent totally laparoscopic distal gastrectomy (TLDG).
Methods
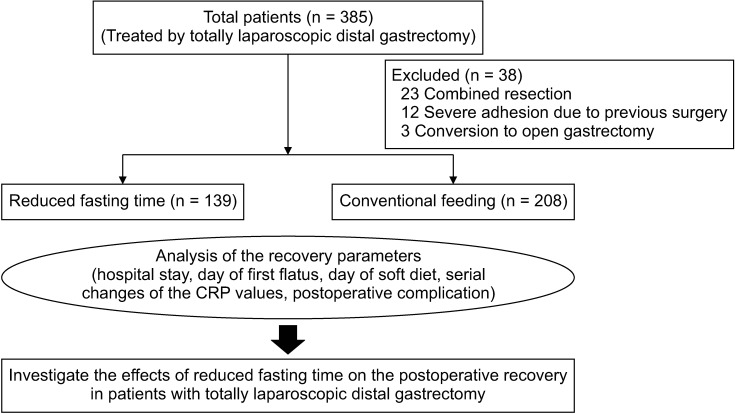
This retrospective study included 347 patients who underwent TLDG. Patients were divided into 2 groups: reduced fasting time group (n = 139) and conventional feeding group (n = 208). We compared the total hospital cost and recovery parameters, such as postoperative complications, mean hospital stay, day of first flatus, initiation of soft diet, and serum CRP levels, between the 2 groups.
Results
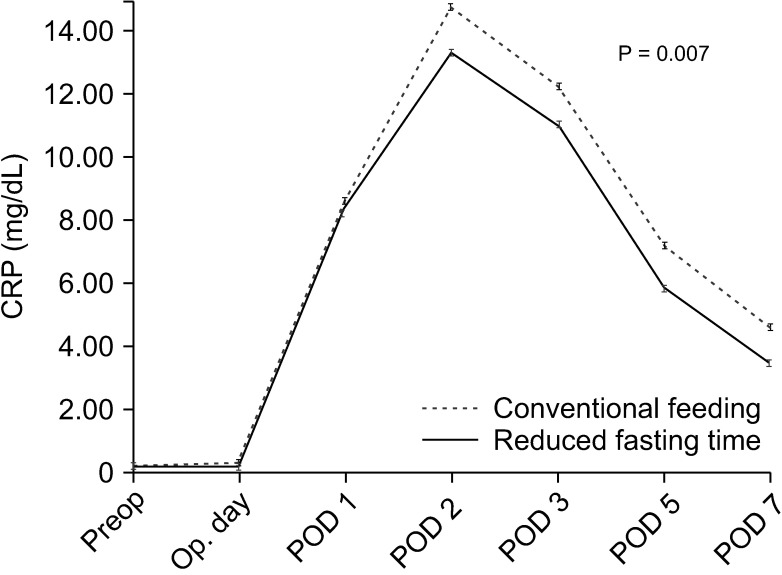
The reduced fasting time group had a lower total hospital cost (P < 0.001) than the conventional feeding group. Regarding postoperative complications, there was no significant difference between the 2 groups (P = 0.085). Patients in the reduced fasting time group had a significantly shorter duration of mean hospital stay (P < 0.001), an earlier first flatus (P = 0.002), an earlier initiation of soft diet (P < 0.001), and lower level of serum CRP concentration (day of surgery, P = 0.036; postoperative days 2, 5, and 7, P = 0.01, 0.009, and 0.012, respectively) than patients in the conventional feeding group.
Conclusion
Reduced fasting time can enhance postoperative recovery in patients who undergo TLDG and may reduce medical costs.
Figure
Reference
-
1. Park KB, Yu B, Park JY, Kwon OK, Yu W. Impact of body mass index on quality of life after distal gastrectomy for gastric cancer. Ann Surg Treat Res. 2019; 96:250–258. PMID: 31073515.2. Warner MA, Warner ME, Weber JG. Clinical significance of pulmonary aspiration during the perioperative period. Anesthesiology. 1993; 78:56–62. PMID: 8424572.3. de Aguilar-Nascimento JE, Dock-Nascimento DB. Reducing preoperative fasting time: a trend based on evidence. World J Gastrointest Surg. 2010; 2:57–60. PMID: 21160851.4. Ahn HS, Yook JH, Park CH, Park YK, Yu W, Lee MS, et al. General perioperative management of gastric cancer patients at high-volume centers. Gastric Cancer. 2011; 14:178–182. PMID: 21373856.5. Lassen K, Dejong CH, Ljungqvist O, Fearon K, Andersen J, Hannemann P, et al. Nutritional support and oral intake after gastric resection in five northern European countries. Dig Surg. 2005; 22:346–352. PMID: 16293965.6. Lobo DN, Bostock KA, Neal KR, Perkins AC, Rowlands BJ, Allison SP. Effect of salt and water balance on recovery of gastrointestinal function after elective colonic resection: a randomised controlled trial. Lancet. 2002; 359:1812–1818. PMID: 12044376.7. Li L, Wang Z, Ying X, Tian J, Sun T, Yi K, et al. Preoperative carbohydrate loading for elective surgery: a systematic review and meta-analysis. Surg Today. 2012; 42:613–624. PMID: 22581289.8. Lewis SJ, Andersen HK, Thomas S. Early enteral nutrition within 24 h of intestinal surgery versus later commencement of feeding: a systematic review and meta-analysis. J Gastrointest Surg. 2009; 13:569–575. PMID: 18629592.9. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196. PMID: 19638912.10. Kim YW, Baik YH, Yun YH, Nam BH, Kim DH, Choi IJ, et al. Improved quality of life outcomes after laparoscopy-assisted distal gastrectomy for early gastric cancer: results of a prospective randomized clinical trial. Ann Surg. 2008; 248:721–727. PMID: 18948798.11. Li MZ, Wu WH, Li L, Zhou XF, Zhu HL, Li JF, et al. Is ERAS effective and safe in laparoscopic gastrectomy for gastric carcinoma? A meta-analysis. World J Surg Oncol. 2018; 16:17. PMID: 29373978.12. Wang D, Kong Y, Zhong B, Zhou X, Zhou Y. Fast-track surgery improves postoperative recovery in patients with gastric cancer: a randomized comparison with conventional postoperative care. J Gastrointest Surg. 2010; 14:620–627. PMID: 20108171.13. Ljungqvist O, Jonathan E. Rhoads lecture 2011: insulin resistance and enhanced recovery after surgery. JPEN J Parenter Enteral Nutr. 2012; 36:389–398. PMID: 22577121.14. Thorell A, Nygren J, Ljungqvist O. Insulin resistance: a marker of surgical stress. Curr Opin Clin Nutr Metab Care. 1999; 2:69–78. PMID: 10453333.15. Goyal RK, Guo Y, Mashimo H. Advances in the physiology of gastric emptying. Neurogastroenterol Motil. 2019; 31:e13546. PMID: 30740834.16. American Society of Anesthesiologists Committee. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists Committee on Standards and Practice Parameters. Anesthesiology. 2011; 114:495–511. PMID: 21307770.17. Soop M, Nygren J, Myrenfors P, Thorell A, Ljungqvist O. Preoperative oral carbohydrate treatment attenuates immediate postoperative insulin resistance. Am J Physiol Endocrinol Metab. 2001; 280:E576–E583. PMID: 11254464.18. Jeong O, Ryu SY, Jung MR, Choi WW, Park YK. The safety and feasibility of early postoperative oral nutrition on the first postoperative day after gastrectomy for gastric carcinoma. Gastric Cancer. 2014; 17:324–331. PMID: 23771588.19. Gabor S, Renner H, Matzi V, Ratzenhofer B, Lindenmann J, Sankin O, et al. Early enteral feeding compared with parenteral nutrition after oesophageal or oesophagogastric resection and reconstruction. Br J Nutr. 2005; 93:509–513. PMID: 15946413.20. Schroeder D, Gillanders L, Mahr K, Hill GL. Effects of immediate postoperative enteral nutrition on body composition, muscle function, and wound healing. JPEN J Parenter Enteral Nutr. 1991; 15:376–383. PMID: 1910100.21. Sato N, Koeda K, Ikeda K, Kimura Y, Aoki K, Iwaya T, et al. Randomized study of the benefits of preoperative corticosteroid administration on the postoperative morbidity and cytokine response in patients undergoing surgery for esophageal cancer. Ann Surg. 2002; 236:184–190. PMID: 12170023.22. Lee SH, Kim KH, Choi CW, Kim SJ, Kim DH, Choi CI, et al. Reduction rate of C-reactive protein as an early predictor of postoperative complications and a reliable discharge indicator after gastrectomy for gastric cancer. Ann Surg Treat Res. 2019; 97:65–73. PMID: 31384611.23. Hoover HC Jr, Ryan JA, Anderson EJ, Fischer JE. Nutritional benefits of immediate postoperative jejunal feeding of an elemental diet. Am J Surg. 1980; 139:153–159. PMID: 6766049.24. Heyland DK, Cook DJ, Guyatt GH. Enteral nutrition in the critically ill patient: a critical review of the evidence. Intensive Care Med. 1993; 19:435–442. PMID: 8294625.25. Braga M, Gianotti L, Gentilini O, Parisi V, Salis C, Di Carlo V. Early postoperative enteral nutrition improves gut oxygenation and reduces costs compared with total parenteral nutrition. Crit Care Med. 2001; 29:242–248. PMID: 11246300.26. Beier-Holgersen R, Brandstrup B. Influence of early postoperative enteral nutrition versus placebo on cell-mediated immunity, as measured with the Multitest CMI. Scand J Gastroenterol. 1999; 34:98–102. PMID: 10048740.27. Ljungqvist O, Nygren J, Thorell A. Insulin resistance and elective surgery. Surgery. 2000; 128:757–760. PMID: 11056438.28. Johnson CD, Kudsk KA. Nutrition and intestinal mucosal immunity. Clin Nutr. 1999; 18:337–344. PMID: 10634917.29. Hadfield RJ, Sinclair DG, Houldsworth PE, Evans TW. Effects of enteral and parenteral nutrition on gut mucosal permeability in the critically ill. Am J Respir Crit Care Med. 1995; 152(5 Pt 1):1545–1548. PMID: 7582291.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Laparoscopy-Assisted and Totally Laparoscopic Distal Gastrectomy: The Short-Term Outcome at a Low Volume Center
- Comparison of laparoscopy-assisted and totally laparoscopic Billroth-II distal gastrectomy for gastric cancer
- Totally Laparoscopic Distal Gastrectomy after Learning Curve Completion: Comparison with Laparoscopy-Assisted Distal Gastrectomy
- Intracorporeal Anastomosis in Laparoscopic Gastric Cancer Surgery
- Comparison of a Postoperative Pain in Laparoscopy-Assisted Distal Gastrectomy and Totally Laparoscopic Distal Gastrectomy according to the Location of the Mini-Laparotomy Site