Yeungnam Univ J Med.
2020 Jul;37(3):179-185. 10.12701/yujm.2019.00451.
Clinical and histopathologic analysis of gynecological cancer: a single institute experience over 7 years
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Yeungnam University Hospital, Daegu, Korea
- 2Department of Obstetrics and Gynecology, Yeungnam University College of Medicine, Daegu, Korea
- KMID: 2506516
- DOI: http://doi.org/10.12701/yujm.2019.00451
Abstract
- Background
Approximately 100,000 women are diagnosed with cancer each year in Korea. According to a survey by the Korean central cancer registry in 2016, uterine cervical cancer, uterine corpus cancer, and ovarian cancer were the 5th, 7th, and 8th most prevalent cancers respectively among Korean women. The present study aims to review the clinico-pathologic characteristics of patients who were treated for major gynecological malignancies at Yeungnam University Medical Center.
Methods
Patients with invasive gynecological cancers from January 2012 to February 2019 were retrospectively identified. We analyzed the clinical features, demographic profiles, pathologic data, treatment modality used, adjuvant treatment used, complications, recurrence, and survival outcomes.
Results
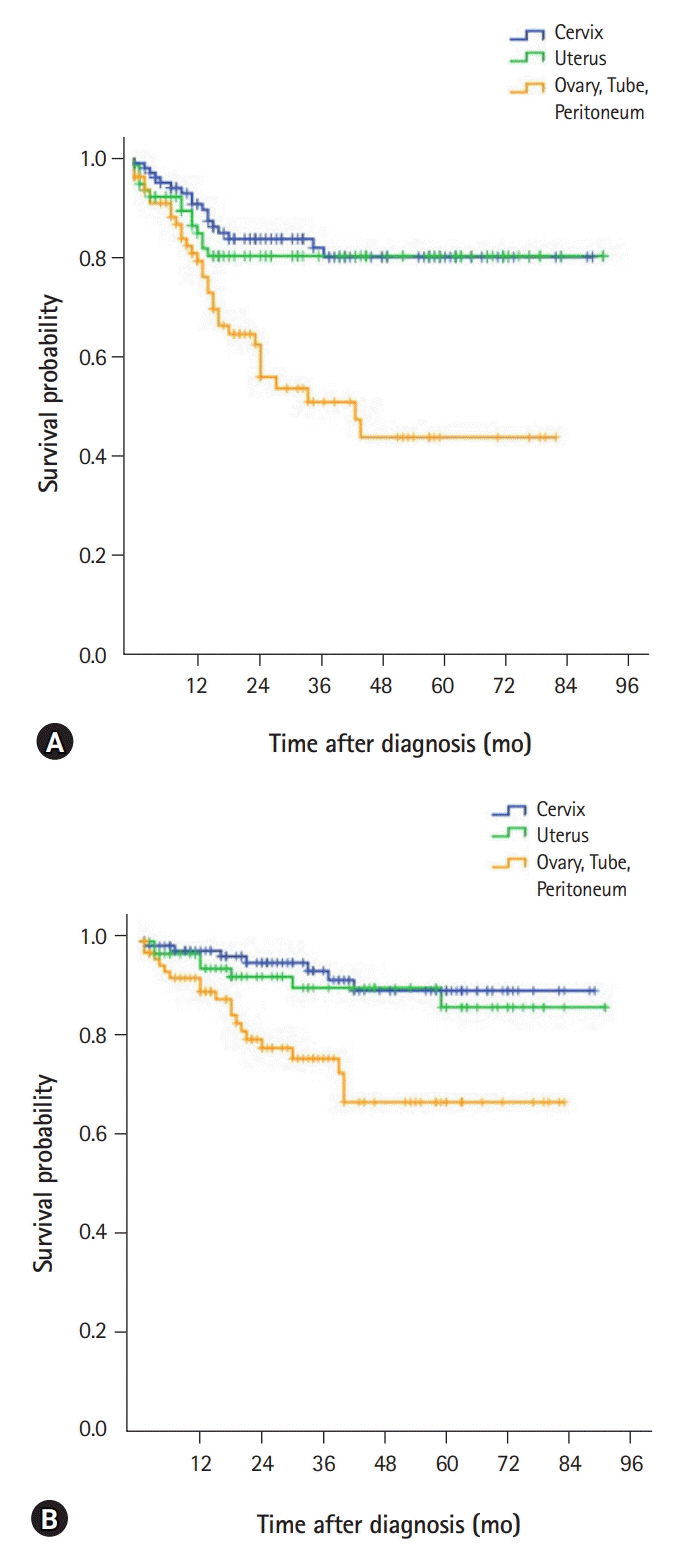
A total of 287 patients (cervical cancer 115; corporal cancer 86; and ovarian, tubal, or primary peritoneal cancer 90) were included. Most cervical (82.7%) and corporal cancers (89.5%) were diagnosed in the early stages (stage I or II), while more than half (58.9%) the cases of ovarian, tubal or peritoneal cancers were diagnosed in the advanced stages (stage III or IV). Surgical complications were observed in 12.2% of cervical cancers, 16.3% of uterine corpus cancers, and 11.1% of ovarian, tubal, and peritoneal cancers, respectively. The 5-year overall survival rate was 94.1%, 91.0%, and 77.1% for cervical, corporal, and ovarian, tubal, or peritoneal cancers, respectively.
Conclusion
Surgical treatment was satisfactory in terms of the incidence of complications, and survival outcomes were generally good. Clinicians should be aware of the clinical and histopathological characteristics of patients with gynecological cancers to be able to provide optimal strategies and counseling.
Keyword
Figure
Reference
-
References
1. Forman D, Ferlay J. The global and regional burden of cancer. In : Stewart BW, Wild CP, editors. World cancer report 2014. Lyon (FR): International Agency for Research on Cancer;2014. p. 16–53.2. Cohen PA, Jhingran A, Oaknin A, Denny L. Cervical cancer. Lancet. 2019; 393:169–82.
Article3. Morice P, Leary A, Creutzberg C, Abu-Rustum N, Darai E. Endometrial cancer. Lancet. 2016; 387:1094–108.
Article4. International Agency for Research on Cancer. Global cancer observatory: cancer today [Internet]. Lyon (FR): International Agency for Research on Cancer;2018. [cited 2020 Jan 22]. http://gco.iarc.fr/.5. Korea Central Cancer Registry; National Cancer Center. Annual report of cancer statistics in Korea in 2015. Sejong (KR): Ministry of Health and Welfare;2017.6. Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, et al. SEER cancer statistics review, 1975-2016: cancer of the cervix uteri (invasive) [Internet]. Bethesda (MD): National Cancer Institute;2019. [cited 2019 Sep 25]. https://seer.cancer.gov/csr/1975_2016/results_merged/sect_05_cervix_uteri.pdf.7. Dowdy SC, Mariani A, Lurain JR. Uterine cancer. In : Berek JS, editor. Berek & Novak's gynecology. 15th ed. Philadelphia (PA): Lippincott Williams & Wilkins;2012. p. 1250–303.8. Janda M, Gebski V, Brand A, Hogg R, Jobling TW, Land R, et al. Quality of life after total laparoscopic hysterectomy versus total abdominal hysterectomy for stage I endometrial cancer (LACE): a randomised trial. Lancet Oncol. 2010; 11:772–80.
Article9. Lu Q, Liu H, Liu C, Wang S, Li S, Guo S, et al. Comparison of laparoscopy and laparotomy for management of endometrial carcinoma: a prospective randomized study with 11-year experience. J Cancer Res Clin Oncol. 2013; 139:1853–9.
Article10. Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, et al. SEER cancer statistics review, 1975-2016: cancer of the corpus and uterus, NOS (invasive) [Internet]. Bethesda (MD): National Cancer Institute;2019. [cited 2019 Sep 25]. https://seer.cancer.gov/csr/1975_2016/results_merged/sect_07_corpus_uteri.pdf.11. Lakhani SR, Manek S, Penault-Llorca F, Flanagan A, Arnout L, Merrett S, et al. Pathology of ovarian cancers in BRCA1 and BRCA2 carriers. Clin Cancer Res. 2004; 10:2473–81.
Article12. Kwon BS, Byun JM, Lee HJ, Jeong DH, Lee TH, Shin KH, et al. Clinical and genetic characteristics of BRCA1/2 mutation in Korean ovarian cancer patients: a multicenter study and literature review. Cancer Res Treat. 2019; 51:941–50.
Article13. Berek JS, Longacre TA, Friedlander M. Ovarian, fallopian tube, and peritoneal cancer. In : Berek JS, editor. Berek & Novak's gynecology. 15th ed. Philadelphia: Lippincott Williams & Wilkins;2012. p. 1350–427.14. Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, et al. SEER cancer statistics review, 1975-2016: cancer of the ovary (invasive) [Internet]. Bethesda (MD): National Cancer Institute;2019. [cited 2019 Sep 25]. https://seer.cancer.gov/csr/1975_2016/results_merged/sect_21_ovary.pdf.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Descriptive Study on Sexuality for Women with Gynecological Cancer
- Current status of gynecological cancer care in India
- Decoding impact of human papillomavirus in gynecological oncology: a narrative review
- Initial Clinical Experience of Pure Single-Incision Robotic Right Hemicolectomy with da Vinci SP Platform
- Unmet Needs and Sexual Distress of Gynecological Cancer Patients according to the Period after Initial Treatment