Obstet Gynecol Sci.
2020 Sep;63(5):605-614. 10.5468/ogs.20080.
Perspective of the comparative effectiveness of non-pharmacologic managements on postpartum hemorrhage using a network meta-analysis
- Affiliations
-
- 1Department of Public Health, Korea University Graduate School, Seoul, Korea
- 2Department of Obstetrics and Gynecology, Korea University, Seoul, Korea
- 3Department of Preventive Medicine, Korea University College of Medicine, Seoul, Korea
- 4Department of Epidemiology and Health Informatics, Graduate School of Public Health, Korea University, Seoul, Korea
- 5Graduate School of Integrative Medicine, CHA University, Pocheon, Korea
- KMID: 2506503
- DOI: http://doi.org/10.5468/ogs.20080
Abstract
Objective
Postpartum hemorrhage (PPH) is the leading cause of maternal mortality worldwide and is both unpredictable and inevitable. While uterotonic drugs are routinely recommended, there is ongoing debate on the ideal intervention to control uterine bleeding. This review aims to compare the use of non-pharmacologic treatments with peripartum hysterectomy in cases of life-threatening uncontrolled obstetric hemorrhage. The review’s objective is to use a network meta-analysis to help prevent maternal deaths and rank the treatments according to success rates.
Methods
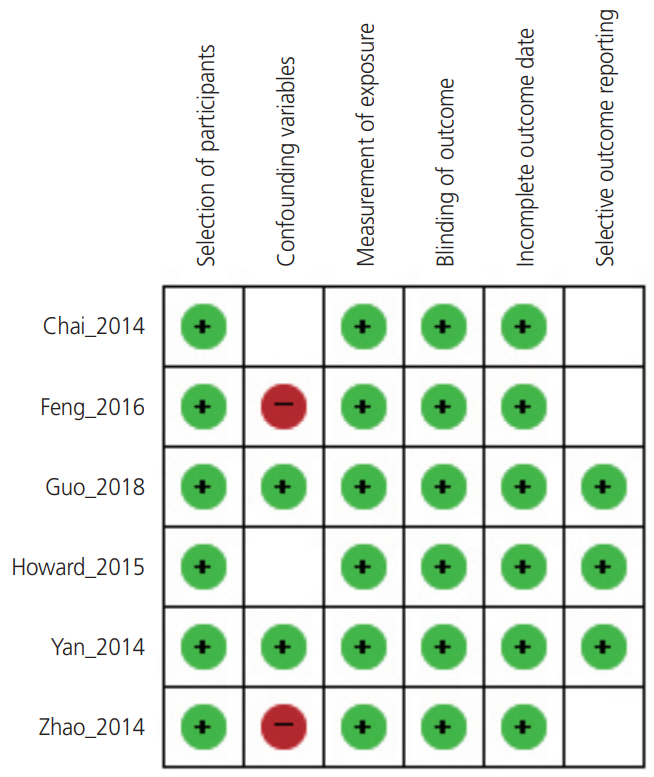
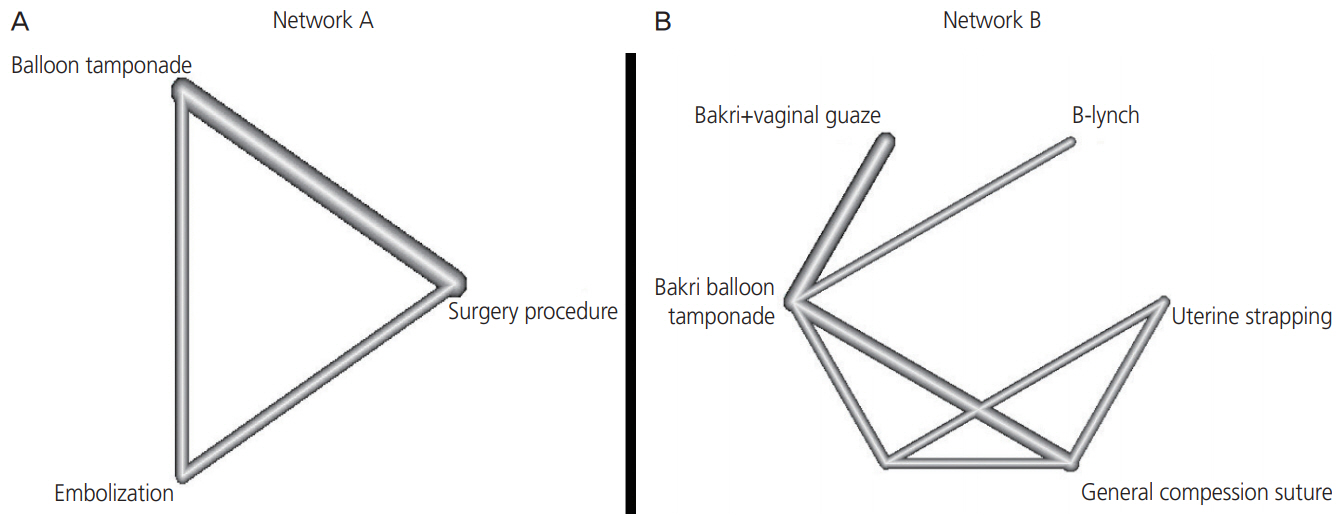
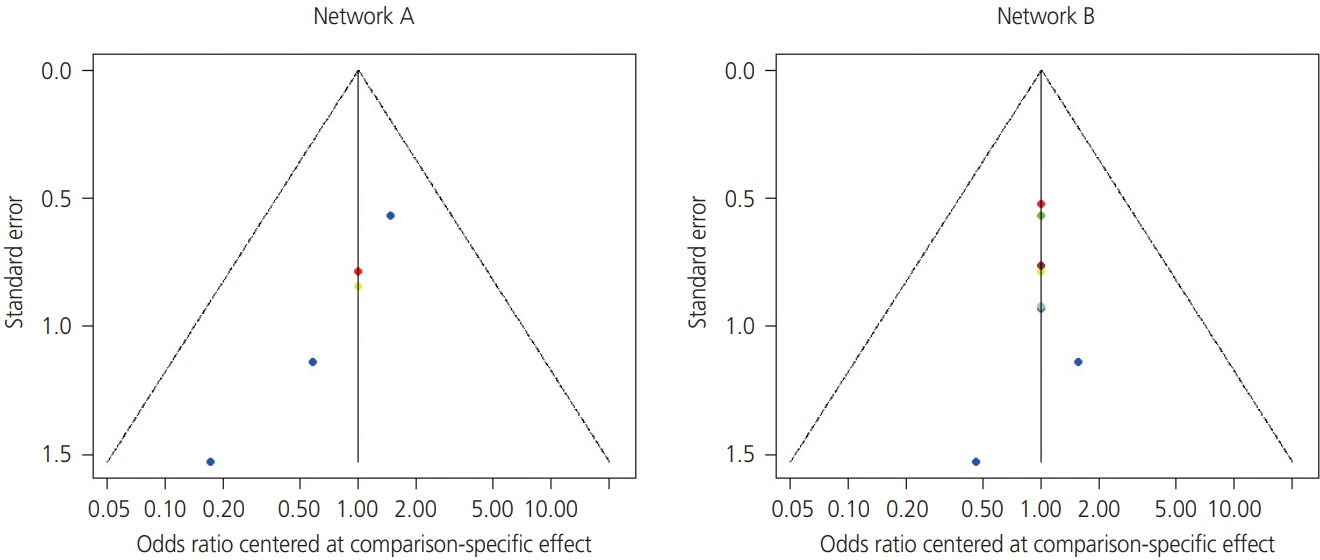
We searched MEDLINE (PubMed), Embase, and the Cochrane Library, from January 2014 until December 2018. A second search was carried out in April 2019 before the final data analysis. Network meta-analysis allows for the calculation of the effect size between treatment groups through indirect treatment comparison.
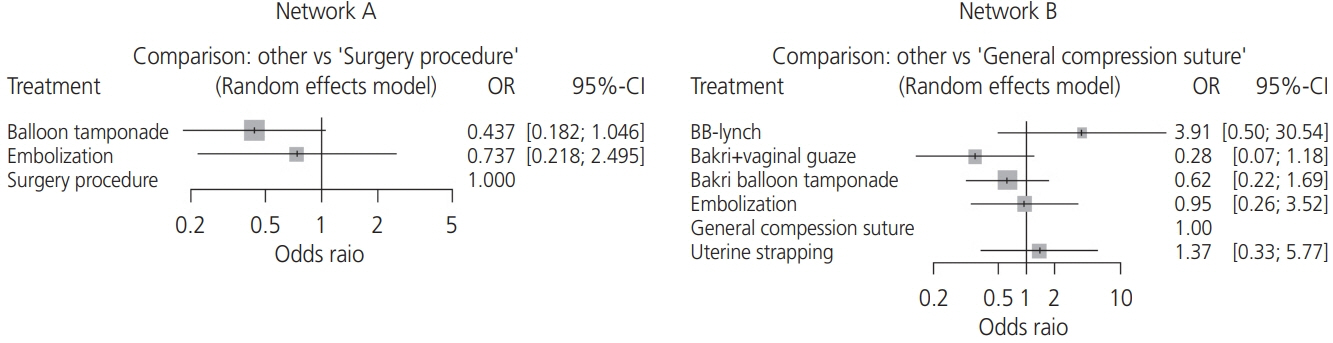
Results
We confirmed that balloon-assisted management is the best intervention for uncontrolled postpartum bleeding with pharmacologic treatment. This is followed by uterine artery embolization and surgical procedures, which can help avoid the need for a hysterectomy. The balloon tamponade demonstrated lower failure rate than the surgical procedure with odds ratio (OR) of 0.44 and 95% confidence intervals (CIs) 0.50–30.54. Uterine artery embolization had a lower risk for hysterectomy than the surgical procedure group (OR, 0.74; 95% CI, 0.22–2.50).
Conclusion
For the quick treatment of postpartum bleeding, balloon tamponade is the best method for uncontrolled postpartum bleeding with pharmacologic treatment, followed by uterine artery embolization and surgical procedures.
Keyword
Figure
Reference
-
References
1. Alkema L, Chou D, Hogan D, Zhang S, Moller AB, Gemmill A, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation InterAgency Group. Lancet. 2016; 387:462–74.
Article2. von Herrath MG, Oldstone MB. Virus-induced autoimmune disease. Curr Opin Immunol. 1996; 8:878–85.3. Say L, Chou D, Gemmill A, Tunçalp Ö, Moller AB, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014; 2:e323–33.
Article4. Romero-Gutiérrez G, Espitia-Vera A, Ponce-Ponce de León AL, Huerta-Vargas LF. Risk factors of maternal death in Mexico. Birth. 2007; 34:21–5.
Article5. Maraschini A, Lega I, D’Aloja P, Buoncristiano M, Dell’Oro S, Donati S, et al. Women undergoing peripartum hysterectomy due to obstetric hemorrhage: a prospective population-based study. Acta Obstet Gynecol Scand. 2020; 99:274–82.
Article6. Rouse DJ, MacPherson C, Landon M, Varner MW, Leveno KJ, Moawad AH, et al. Blood transfusion and cesarean delivery. Obstet Gynecol. 2006; 108:891–7.
Article7. World Health Organization. Guideline: delayed umbilical cord clamping for improved maternal and infant health and nutrition outcomes. Geneva: World Health Organization;2014.8. Begley CM, Gyte GM, Devane D, McGuire W, Weeks A, Biesty LM. Active versus expectant management for women in the third stage of labour. Cochrane Database Syst Rev. 2019; 2:CD007412.
Article9. Frolova AI, Stout MJ, Tuuli MG, López JD, Macones GA, Cahill AG. Duration of the third stage of labor and risk of postpartum hemorrhage. Obstet Gynecol. 2016; 127:951–6.
Article10. Say L, Souza JP, Pattinson RC; WHO working group on Maternal Mortality and Morbidity classifications. Maternal near miss--towards a standard tool for monitoring quality of maternal health care. Best Pract Res Clin Obstet Gynaecol. 2009; 23:287–96.11. Byun JM, Kim YN, Jeong DH, Seo YJ, Jeong EJ, Kang JY, et al. Prognosis and indication of emergency hysterectomy following postpartum hemorrhage. Korean J Obstet Gynecol. 2012; 55:901–6.
Article12. Mercier FJ, Van de Velde M. Major obstetric hemorrhage. Anesthesiol Clin. 2008; 26:53–66.
Article13. Drucker M, Wallach RC. Uterine packing: a reappraisal. Mt Sinai J Med. 1979; 46:191–4.14. Bakri YN, Amri A, Abdul Jabbar F. Tamponade-balloon for obstetrical bleeding. Int J Gynaecol Obstet. 2001; 74:139–42.
Article15. Tamizian O, Arulkumaran S. The surgical management of postpartum haemorrhage. Curr Opin Obstet Gynecol. 2001; 13:127–31.
Article16. B-Lynch C, Coker A, Lawal AH, Abu J, Cowen MJ. The B‐Lynch surgical technique for the control of massive postpartum haemorrhage: an alternative to hysterectomy? Five cases reported. BJOG. 1997; 104:372–5.
Article17. Yucel O, Ozdemir I, Yucel N, Somunkiran A. Emergency peripartum hysterectomy: a 9-year review. Arch Gynecol Obstet. 2006; 274:84–7.
Article18. Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015; 162:777–84.
Article19. Chai VY, To WW. Uterine compression sutures for management of severe postpartum haemorrhage: five-year audit. Hong Kong Med J. 2014; 20:113–20.20. Feng B, Zhai J, Cai Y. Results of surgical intervention in treating post-cesarean intractable postpartum hemorrhage. Int J Clin Exp Med. 2016; 9:5154–60.21. Guo Y, Hua R, Bian S, Xie X, Ma J, Cai Y, et al. Intrauterine Bakri balloon and vaginal tamponade combined with abdominal compression for the management of postpartum hemorrhage. J Obstet Gynaecol Can. 2018; 40:561–5.
Article22. Howard TF, Grobman WA. The relationship between timing of postpartum hemorrhage interventions and adverse outcomes. Am J Obstet Gynecol. 2015; 213:239.e1–3.
Article23. Shim SR, Kim SJ, Lee J, Rücker G. Network meta-analysis: application and practice using R software. Epidemiol Health. 2019; 41:e2019013.
Article24. Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016; 355:i4919.
Article25. Bilandzic A, Fitzpatrick T, Rosella L, Henry D. Risk of bias in systematic reviews of non-randomized studies of adverse cardiovascular effects of thiazolidinediones and cyclooxygenase-2 inhibitors: application of a new Cochrane risk of bias tool. PLoS Med. 2016; 13:e1001987.
Article26. Zhang YJ, Wang N, Gu ZC, Wei AH, Cheng AN, Fang SS, et al. A network meta-analysis for safety of endothelin receptor antagonists in pulmonary arterial hypertension. Cardiovasc Diagn Ther. 2019; 9:239–49.
Article27. Gallos ID, Papadopoulou A, Man R, Athanasopoulos N, Tobias A, Price MJ, et al. Uterotonic agents for preventing postpartum haemorrhage: a network meta-analysis. Cochrane Database Syst Rev. 2018; 12:CD011689.
Article28. Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011; 343:d4002.
Article29. Rücker G, Schwarzer G. Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med Res Methodol. 2015; 15:58.
Article30. Yan JY, Zhou ZM, Xu X, Huang XY, Xu RL, Lin SH. Risk factors and surgical interventions associated with primary postpartum haemorrhage unresponsive to first-line therapies. J Obstet Gynaecol. 2014; 34:588–92.
Article31. Zhao Y, Zhang Y, Li Z. Appropriate second-line therapies for management of severe postpartum hemorrhage. Int J Gynaecol Obstet. 2014; 127:180–2.
Article32. Dahlke JD, Mendez-Figueroa H, Maggio L, Hauspurg AK, Sperling JD, Chauhan SP, et al. Prevention and management of postpartum hemorrhage: a comparison of 4 national guidelines. Am J Obstet Gynecol. 2015; 213:76.e1–10.
Article33. California Maternal Quality Care Collaborative. OB hemorrhage toolkit V20. [Internet]. Stanford (CA): California Maternal Quality Care Collaborative;c2015. [cited 2020 March 30]. Available from: https://www.cmqcc.org/resources-tool-kits/toolkits/ob-hemorrhage-toolkit.34. Kaya B, Tuten A, Daglar K, Misirlioglu M, Polat M, Yildirim Y, et al. Balloon tamponade for the management of postpartum uterine hemorrhage. J Perinat Med. 2014; 42:745–53.
Article35. Chen C, Lee SM, Kim JW, Shin JH. Recent update of embolization of postpartum hemorrhage. Korean J Radiol. 2018; 19:585–96.
Article36. Oyelese Y, Ananth CV. Postpartum hemorrhage: epidemiology, risk factors, and causes. Clin Obstet Gynecol. 2010; 53:147–56.
Article