Acute Crit Care.
2020 Aug;35(3):189-196. 10.4266/acc.2020.00031.
Association between postoperative fluid balance and mortality and morbidity in critically ill patients with complicated intra-abdominal infections: a retrospective study
- Affiliations
-
- 1Department of Surgery, Ajou University School of Medicine, Suwon, Korea
- 2Department of Surgery, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea
- KMID: 2506098
- DOI: http://doi.org/10.4266/acc.2020.00031
Abstract
- Background
Postoperative fluid overload may increase the risk of developing pulmonary complications and other adverse outcomes. We evaluated the impact of excessive fluid administration on postoperative outcomes in critically ill patients.
Methods
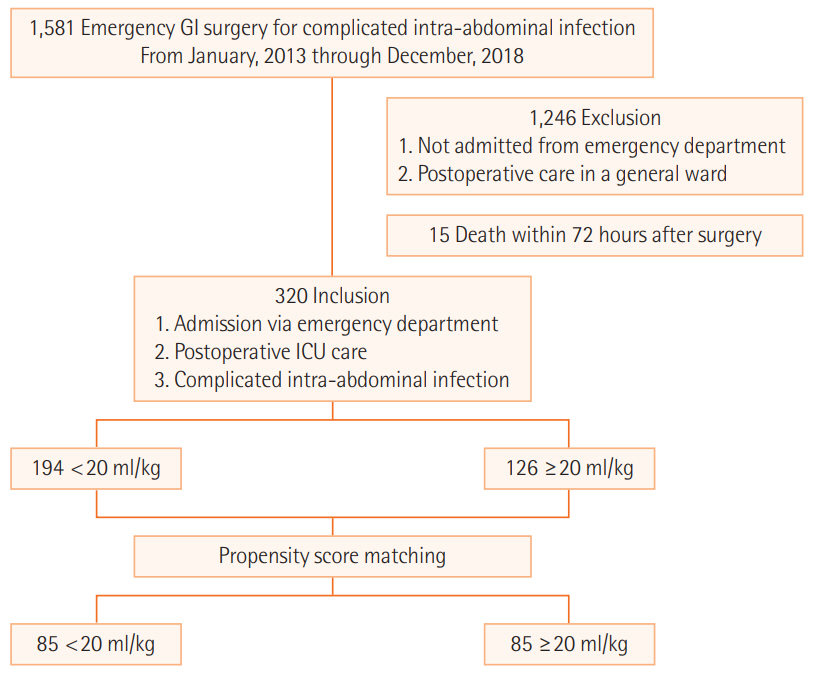
We reviewed the medical records of 320 patients admitted to intensive care unit (ICU) after emergency abdominal surgery for complicated intra-abdominal infection (cIAI) between January 2013 and December 2018. The fluid balance data of the patients were reviewed for a maximum of 7 days. The patients were grouped based on average daily fluid balance with a cutoff value of 20 ml/kg/day. Propensity score matching was performed to reduce the underlying differences between the groups.
Results
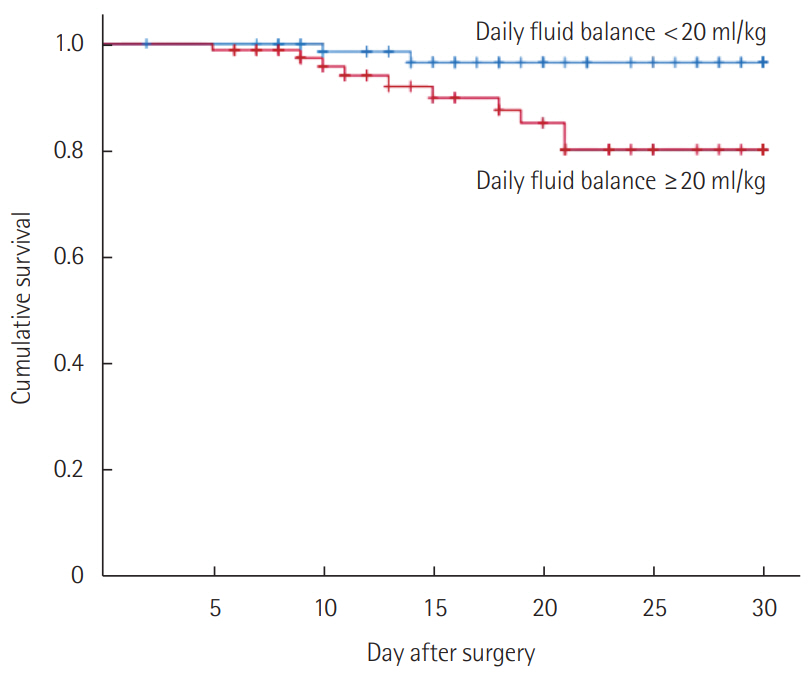
Patients with an average daily fluid balance of ≥ 20 ml/kg/day were associated with higher rates of 30-day mortality (11.8% vs. 2.4%; P = 0.036) than those with lower fluid balance ( < 20 ml/kg/day). Kaplan-Meier survival curves for 30-day mortality in these groups also showed a better survival rate in the lower fluid balance group with a statistical significance (P = 0.020). The percentage of patients who developed pulmonary consolidation during ICU stay (47.1% vs. 24.7%; P = 0.004) was higher in the fluid-overloaded group. Percentages of newly developed pleural effusion (61.2% vs. 57.7%; P = 0.755), reintubation (18.8% vs. 10.6%; P = 0.194), and infectious complications (55.3% vs. 49.4%; P = 0.539) showed no significant differences between the two groups.
Conclusions
Postoperative fluid overload in patients who underwent emergency surgery for cIAI was associated with higher 30-day mortality and more frequent occurrence of pulmonary consolidation. Postoperative fluid balance should be adjusted carefully to avoid adverse clinical outcomes.
Figure
Reference
-
1. Balakumar V, Murugan R, Sileanu FE, Palevsky P, Clermont G, Kellum JA. Both positive and negative fluid balance may be associated with reduced long-term survival in the critically ill. Crit Care Med. 2017; 45:e749–57.
Article2. Lee J, de Louw E, Niemi M, Nelson R, Mark RG, Celi LA, et al. Association between fluid balance and survival in critically ill patients. J Intern Med. 2015; 277:468–77.
Article3. Brandstrup B, Tønnesen H, Beier-Holgersen R, Hjortsø E, Ørding H, Lindorff-Larsen K, et al. Effects of intravenous fluid restriction on postoperative complications: comparison of two perioperative fluid regimens: a randomized assessor-blinded multicenter trial. Ann Surg. 2003; 238:641–8.4. Myles PS, Bellomo R, Corcoran T, Forbes A, Peyton P, Story D, et al. Restrictive versus liberal fluid therapy for major abdominal surgery. N Engl J Med. 2018; 378:2263–74.
Article5. Wang N, Jiang L, Zhu B, Wen Y, Xi XM; Beijing Acute Kidney Injury Trial (BAKIT) Workgroup. Fluid balance and mortality in critically ill patients with acute kidney injury: a multicenter prospective epidemiological study. Crit Care. 2015; 19:371.
Article6. Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017; 43:304–77.7. Zhu AC, Agarwala A, Bao X. Perioperative fluid management in the Enhanced Recovery after Surgery (ERAS) pathway. Clin Colon Rectal Surg. 2019; 32:114–20.
Article8. Sartelli M, Abu-Zidan FM, Catena F, Griffiths EA, Di Saverio S, Coimbra R, et al. Global validation of the WSES Sepsis Severity Score for patients with complicated intra-abdominal infections: a prospective multicentre study (WISS Study). World J Emerg Surg. 2015; 10:61.9. Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001; 345:1368–77.
Article10. Kelm DJ, Perrin JT, Cartin-Ceba R, Gajic O, Schenck L, Kennedy CC. Fluid overload in patients with severe sepsis and septic shock treated with early goal-directed therapy is associated with increased acute need for fluid-related medical interventions and hospital death. Shock. 2015; 43:68–73.
Article11. Barmparas G, Liou D, Lee D, Fierro N, Bloom M, Ley E, et al. Impact of positive fluid balance on critically ill surgical patients: a prospective observational study. J Crit Care. 2014; 29:936–41.
Article12. Shim HJ, Jang JY, Lee SH, Lee JG. The effect of positive balance on the outcomes of critically ill noncardiac postsurgical patients: a retrospective cohort study. J Crit Care. 2014; 29:43–8.
Article13. Mazuski JE, Tessier JM, May AK, Sawyer RG, Nadler EP, Rosengart MR, et al. The Surgical Infection Society Revised Guidelines on the Management of Intra-Abdominal Infection. Surg Infect (Larchmt). 2017; 18:1–76.
Article14. Sartelli M, Chichom-Mefire A, Labricciosa FM, Hardcastle T, Abu-Zidan FM, Adesunkanmi AK, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017; 12:29.15. McNarry AF, Goldhill DR. Simple bedside assessment of level of consciousness: comparison of two simple assessment scales with the Glasgow Coma scale. Anaesthesia. 2004; 59:34–7.
Article16. Calandra T, Cohen J; International Sepsis Forum Definition of Infection in the ICU Consensus Conference. The international sepsis forum consensus conference on definitions of infection in the intensive care unit. Crit Care Med. 2005; 33:1538–48.
Article17. Levy MM, Evans LE, Rhodes A. The surviving sepsis campaign bundle: 2018 update. Crit Care Med. 2018; 46:997–1000.
Article18. RENAL Replacement Therapy Study Investigators, Bellomo R, Cass A, Cole L, Finfer S, Gallagher M, et al. An observational study fluid balance and patient outcomes in the randomized evaluation of normal vs. augmented level of replacement therapy trial. Crit Care Med. 2012; 40:1753–60.19. Samoni S, Vigo V, Reséndiz LI, Villa G, De Rosa S, Nalesso F, et al. Impact of hyperhydration on the mortality risk in critically ill patients admitted in intensive care units: comparison between bioelectrical impedance vector analysis and cumulative fluid balance recording. Crit Care. 2016; 20:95.
Article20. Silversides JA, Fitzgerald E, Manickavasagam US, Lapinsky SE, Nisenbaum R, Hemmings N, et al. Deresuscitation of patients with iatrogenic fluid overload is associated with reduced mortality in critical illness. Crit Care Med. 2018; 46:1600–7.
Article21. Saugel B, Vincent JL, Wagner JY. Personalized hemodynamic management. Curr Opin Crit Care. 2017; 23:334–41.
Article22. Alvarado Sánchez JI, Amaya Zúñiga WF, Monge García MI. Predictors to intravenous fluid responsiveness. J Intensive Care Med. 2018; 33:227–40.
Article23. Saugel B, Ringmaier S, Holzapfel K, Schuster T, Phillip V, Schmid RM, et al. Physical examination, central venous pressure, and chest radiography for the prediction of transpulmonary thermodilution-derived hemodynamic parameters in critically ill patients: a prospective trial. J Crit Care. 2011; 26:402–10.
Article24. Monnet X, Teboul JL. Passive leg raising: five rules, not a drop of fluid! Crit Care. 2015; 19:18.
Article25. Jones SL, Tanaka A, Eastwood GM, Young H, Peck L, Bellomo R, et al. Bioelectrical impedance vector analysis in critically ill patients: a prospective, clinician-blinded investigation. Crit Care. 2015; 19:290.
Article26. Dewitte A, Carles P, Joannès-Boyau O, Fleureau C, Roze H, Combe C, et al. Bioelectrical impedance spectroscopy to estimate fluid balance in critically ill patients. J Clin Monit Comput. 2016; 30:227–33.
Article27. Murphy CV, Schramm GE, Doherty JA, Reichley RM, Gajic O, Afessa B, et al. The importance of fluid management in acute lung injury secondary to septic shock. Chest. 2009; 136:102–9.
Article28. Cordemans C, De Laet I, Van Regenmortel N, Schoonheydt K, Dits H, Huber W, et al. Fluid management in critically ill patients: the role of extravascular lung water, abdominal hypertension, capillary leak, and fluid balance. Ann Intensive Care. 2012; 2(Suppl 1 Diagnosis and management of intra-abdominal hyperten):S1.
Article29. Hjortrup PB, Haase N, Bundgaard H, Thomsen SL, Winding R, Pettilä V, et al. Restricting volumes of resuscitation fluid in adults with septic shock after initial management: the CLASSIC randomised, parallel-group, multicentre feasibility trial. Intensive Care Med. 2016; 42:1695–705.
Article30. Besen BA, Gobatto AL, Melro LM, Maciel AT, Park M. Fluid and electrolyte overload in critically ill patients: an overview. World J Crit Care Med. 2015; 4:116–29.
Article31. O’Connor ME, Prowle JR. Fluid overload. Crit Care Clin. 2015; 31:803–21.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Influence of Daily Fluid Balance prior to Continuous Renal Replacement Therapy on Outcomes in Critically Ill Patients
- Abdominal compartment syndrome in critically ill patients
- Relationship between Intake and Output Balance and Body Weight Changes in Intensive Care Unit Patients
- Clinical Effects of Intra-Abdominal Pressure in Critically Ill Trauma Patients
- Clinical Significance of Intra-Abdominal Hypertension