Arch Hand Microsurg.
2020 Sep;25(3):238-247. 10.12790/ahm.20.0018.
Neuropathic Pain: How to Assess and Treat a Maladaptive Pain Response
- Affiliations
-
- 1Department of Orthopaedic Surgery, Ewha Womans University Mokdong Hospital, Ewha Womans University College of Medicine, Seoul, Korea
- KMID: 2505906
- DOI: http://doi.org/10.12790/ahm.20.0018
Abstract
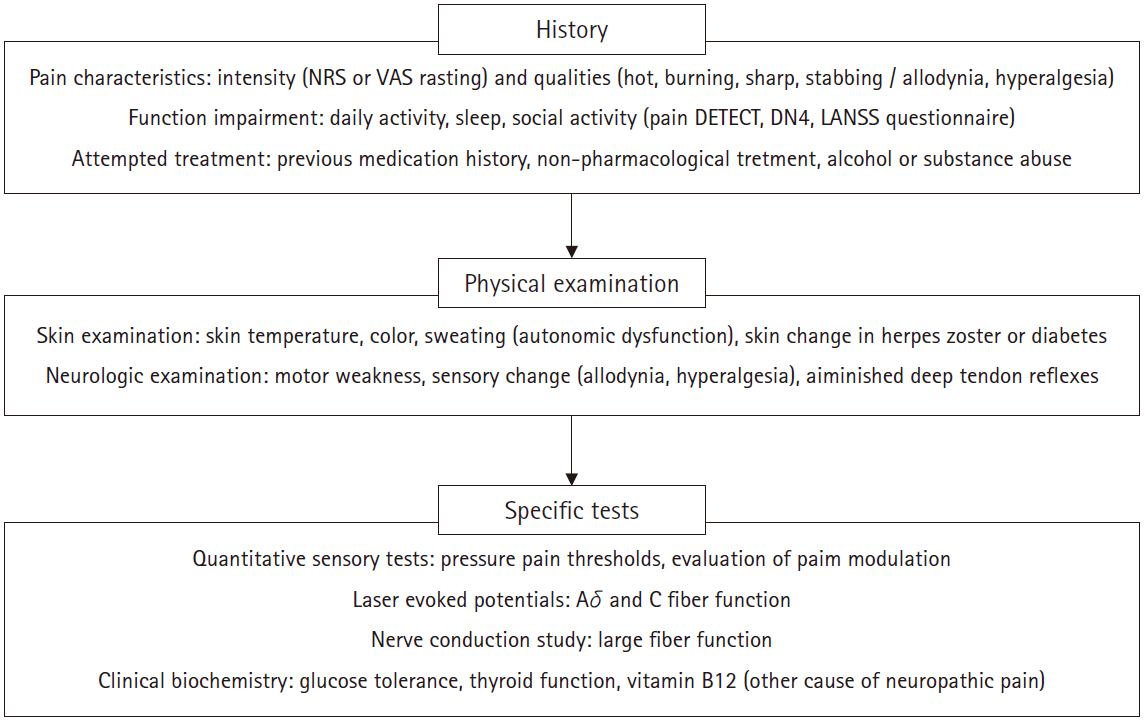
- Neuropathic pain is associated with primary lesion or dysfunction of the peripheral and central nerve systems, affecting up to 10% of the general population. Although both nociceptive pain and neuropathic pain utilize the same nervous system pathways, physiologic differences exist in the pathologic mechanism, clinical presentation, and treatments. Ectopic activity in primary afferent fibers, excitatory and inhibitory somatosensory signaling, nociceptive neuron alterations, and central pain modulation have been implicated in neuropathic pain. These neuropathic mechanisms are associated with the complexity of symptoms, difficult treatment decisions, and challenging poor outcomes. Treatment options include pharmacologic (e.g., anticonvulsants, antidepressants, lidocaine, N-methyl-D-aspartate antagonist, opioids), physical, psychological (e.g., cognitive behavioral therapy), or interventional management (e.g., peripheral or neuro-axial nerve blockade, spinal cord stimulators, intrathecal medications). Medication selection should be individualized, considering patients’ symptoms and potential beneficial or deleterious effects (side effects) on comorbidities. The interventional management of chronic neuropathic pain should be considered for patients who have not responded to pharmacologic and non-interventional treatments, as an integral component of a more comprehensive approach. This article presents an overview of physiological mechanisms, clinical presentation, and assessment of neuropathic pain, and discusses treatment options for neuropathic pain.
Keyword
Figure
Reference
-
1. Jensen TS, Baron R, Haanpaa M, et al. A new definition of neuropathic pain. Pain. 2011; 152:2204–5.
Article2. Giske L, Bautz-Holter E, Sandvik L, Roe C. Relationship between pain and neuropathic symptoms in chronic musculoskeletal pain. Pain Med. 2009; 10:910–7.
Article3. Nakamura M, Nishiwaki Y, Sumitani M, et al. Investigation of chronic musculoskeletal pain (third report): with special reference to the importance of neuropathic pain and psychogenic pain. J Orthop Sci. 2014; 19:667–75.
Article4. Smart KM, Blake C, Staines A, Thacker M, Doody C. Mechanisms-based classifications of musculoskeletal pain: part 1 of 3: symptoms and signs of central sensitisation in patients with low back (+/- leg) pain. Man Ther. 2012; 17:336–44.5. Colloca L, Ludman T, Bouhassira D, et al. Neuropathic pain. Nat Rev Dis Primers. 2017; 3:17002.
Article6. Smart KM, Blake C, Staines A, Doody C. The discriminative validity of "nociceptive," "peripheral neuropathic," and "central sensitization" as mechanisms-based classifications of musculoskeletal pain. Clin J Pain. 2011; 27:655–63.
Article7. Dworkin RH, O'Connor AB, Backonja M, et al. Pharmacologic management of neuropathic pain: evidence-based recommendations. Pain. 2007; 132:237–51.
Article8. Zusman M. Mechanisms of peripheral neuropathic pain: implications for musculoskeletal physiotherapy. Physical Therapy Reviews. 2008; 13:313–23.
Article9. Meacham K, Shepherd A, Mohapatra DP, Haroutounian S. Neuropathic pain: central vs. peripheral mechanisms. Curr Pain Headache Rep. 2017; 21:28.
Article10. Gilron I, Watson CP, Cahill CM, Moulin DE. Neuropathic pain: a practical guide for the clinician. CMAJ. 2006; 175:265–75.
Article11. Melzack R. The short-form McGill Pain Questionnaire. Pain. 1987; 30:191–7.
Article12. Osman A, Barrios FX, Gutierrez PM, Kopper BA, Merrifield T, Grittmann L. The Pain Catastrophizing Scale: further psychometric evaluation with adult samples. J Behav Med. 2000; 23:351–65.13. Galer BS, Jensen MP. Development and preliminary validation of a pain measure specific to neuropathic pain: the Neuropathic Pain Scale. Neurology. 1997; 48:332–8.
Article14. Freynhagen R, Baron R, Gockel U, Tolle TR. painDETECT: a new screening questionnaire to identify neuropathic components in patients with back pain. Curr Med Res Opin. 2006; 22:1911–20.
Article15. Chatila N, Pereira B, Maarrawi J, Dallel R. Validation of a new Arabic version of the Neuropathic Pain Diagnostic Questionnaire (DN4). Pain Pract. 2017; 17:78–87.
Article16. Bennett M. The LANSS Pain Scale: the Leeds assessment of neuropathic symptoms and signs. Pain. 2001; 92:147–57.
Article17. Tampin B, Briffa NK, Goucke R, Slater H. Identification of neuropathic pain in patients with neck/upper limb pain: application of a grading system and screening tools. Pain. 2013; 154:2813–22.
Article18. Gursoy AE, Kolukisa M, Yildiz GB, Kocaman G, Celebi A, Kocer A. Relationship between electrodiagnostic severity and neuropathic pain assessed by the LANSS pain scale in carpal tunnel syndrome. Neuropsychiatr Dis Treat. 2013; 9:65–71.19. Ceceli E, Gumruk S, Okumus M, Kocaoglu S, Goksu H, Karagoz A. Comparison of 2 methods of neuropathic pain assessment in carpal tunnel syndrome and hand functions. Neurosciences (Riyadh). 2018; 23:23–8.
Article20. Rolke R, Baron R, Maier C, et al. Quantitative sensory testing in the German Research Network on Neuropathic Pain (DFNS): standardized protocol and reference values. Pain. 2006; 123:231–43.
Article21. Garcia-Larrea L. Objective pain diagnostics: clinical neurophysiology. Neurophysiol Clin. 2012; 42:187–97.
Article22. Haanpaa M, Attal N, Backonja M, et al. NeuPSIG guidelines on neuropathic pain assessment. Pain. 2011; 152:14–27.23. Fuzier R, Rousset J, Bataille B, Salces-y-Nedeo A, Magues JP. One half of patients reports persistent pain three months after orthopaedic surgery. Anaesth Crit Care Pain Med. 2015; 34:159–64.
Article24. Kurien T, Arendt-Nielsen L, Petersen KK, Graven-Nielsen T, Scammell BE. Preoperative neuropathic pain-like symptoms and central pain mechanisms in knee osteoarthritis predicts poor outcome 6 months after total knee replacement surgery. J Pain. 2018; 19:1329–41.
Article25. Sadler A, Wilson J, Colvin L. Acute and chronic neuropathic pain in the hospital setting: use of screening tools. Clin J Pain. 2013; 29:507–11.26. Phillips JR, Hopwood B, Arthur C, Stroud R, Toms AD. The natural history of pain and neuropathic pain after knee replacement: a prospective cohort study of the point prevalence of pain and neuropathic pain to a minimum three-year follow-up. Bone Joint J. 2014; 96:1227–33.27. Roh YH, Kim S, Gong HS, Baek GH. Influence of centrally mediated symptoms on functional outcomes after carpal tunnel release. Sci Rep. 2018; 8:11134.
Article28. Roh YH, Koh YD, Kim JO, Lee KH, Gong HS, Baek GH. Preoperative pain sensitization is associated with postoperative pillar pain after open carpal tunnel release. Clin Orthop Relat Res. 2018; 476:734–40.
Article29. Roh YH, Noh JH, Oh JH, Gong HS, Baek GH. To what degree do pain-coping strategies affect joint stiffness and functional outcomes in patients with hand fractures? Clin Orthop Relat Res. 2015; 473:3484–90.
Article30. Roh YH, Gong HS, Baek GH. The prognostic value of pain sensitization in patients with lateral epicondylitis. J Hand Surg Am. 2019; 44:250. e1-7.
Article31. Roh YH, Gong HS, Baek GH. Prognostic value of pain sensitization during early recovery after distal radius fracture in complex regional pain syndrome. Pain Med. 2019; 20:1066–71.
Article32. Namaka M, Gramlich CR, Ruhlen D, Melanson M, Sutton I, Major J. A treatment algorithm for neuropathic pain. Clin Ther. 2004; 26:951–79.
Article33. Galluzzi KE. Management of neuropathic pain. J Am Osteopath Assoc. 2005; 105(9 Suppl 4):S12–9.34. Katz NP, Gammaitoni AR, Davis MW, Dworkin RH; Lidoderm Patch Study Group. Lidocaine patch 5% reduces pain intensity and interference with quality of life in patients with postherpetic neuralgia: an effectiveness trial. Pain Med. 2002; 3:324–32.
Article35. Backonja M, Beydoun A, Edwards KR, et al. Gabapentin for the symptomatic treatment of painful neuropathy in patients with diabetes mellitus: a randomized controlled trial. JAMA. 1998; 280:1831–6.
Article36. Raja SN, Haythornthwaite JA, Pappagallo M, et al. Opioids versus antidepressants in postherpetic neuralgia: a randomized, placebo-controlled trial. Neurology. 2002; 59:1015–21.
Article37. Rowbotham MC, Twilling L, Davies PS, Reisner L, Taylor K, Mohr D. Oral opioid therapy for chronic peripheral and central neuropathic pain. N Engl J Med. 2003; 348:1223–32.
Article38. Bates D, Schultheis BC, Hanes MC, et al. A comprehensive algorithm for management of neuropathic pain. Pain Med. 2019; 20:S2–S12.
Article39. Thieme H, Morkisch N, Rietz C, Dohle C, Borgetto B. The efficacy of movement representation techniques for treatment of limb pain--a systematic review and meta-analysis. J Pain. 2016; 17:167–80.
Article40. Dobson JL, McMillan J, Li L. Benefits of exercise intervention in reducing neuropathic pain. Front Cell Neurosci. 2014; 8:102.
Article41. Eccleston C, Hearn L, Williams AC. Psychological therapies for the management of chronic neuropathic pain in adults. Cochrane Database Syst Rev. 2015; 2015:CD011259.
Article42. Hurley RW, Adams MC, Benzon HT. Neuropathic pain: treatment guidelines and updates. Curr Opin Anaesthesiol. 2013; 26:580–7.43. Otis JD, Sanderson K, Hardway C, Pincus M, Tun C, Soumekh S. A randomized controlled pilot study of a cognitive-behavioral therapy approach for painful diabetic peripheral neuropathy. J Pain. 2013; 14:475–82.
Article44. Dworkin RH, O'Connor AB, Kent J, et al. Interventional management of neuropathic pain: NeuPSIG recommendations. Pain. 2013; 154:2249–61.
Article45. Nee RJ, Butler D. Management of peripheral neuropathic pain: integrating neurobiology, neurodynamics, and clinical evidence. Physical Therapy in sport. 2006; 7:36–49.
Article46. Stacey BR. Management of peripheral neuropathic pain. Am J Phys Med Rehabil. 2005; 84(3 Suppl):S4–16.
Article47. North RB, Kumar K, Wallace MS, et al. Spinal cord stimulation versus re-operation in patients with failed back surgery syndrome: an international multicenter randomized controlled trial (EVIDENCE study). Neuromodulation. 2011; 14:330–5.
Article48. Kumar K, Rizvi S. Cost-effectiveness of spinal cord stimulation therapy in management of chronic pain. Pain Med. 2013; 14:1631–49.
Article49. Lefaucheur JP. Cortical neurostimulation for neuropathic pain: state of the art and perspectives. Pain. 2016; 157 Suppl 1:S81–9.50. Sukul VV, Slavin KV. Deep brain and motor cortex stimulation. Curr Pain Headache Rep. 2014; 18:427.
Article51. Stearns L, Boortz-Marx R, Du Pen S, et al. Intrathecal drug delivery for the management of cancer pain: a multidisciplinary consensus of best clinical practices. J Support Oncol. 2005; 3:399–408.52. Pope JE, Deer TR, Bruel BM, Falowski S. Clinical uses of intrathecal therapy and its placement in the pain care algorithm. Pain Pract. 2016; 16:1092–106.
Article