J Korean Acad Nurs.
2019 Dec;49(6):724-735. 10.4040/jkan.2019.49.6.724.
Path Analysis for Delirium on Patient Prognosis in Intensive Care Units
- Affiliations
-
- 1College of Nursing, The Catholic University of Korea, Seoul, Korea
- KMID: 2505801
- DOI: http://doi.org/10.4040/jkan.2019.49.6.724
Abstract
- Purpose
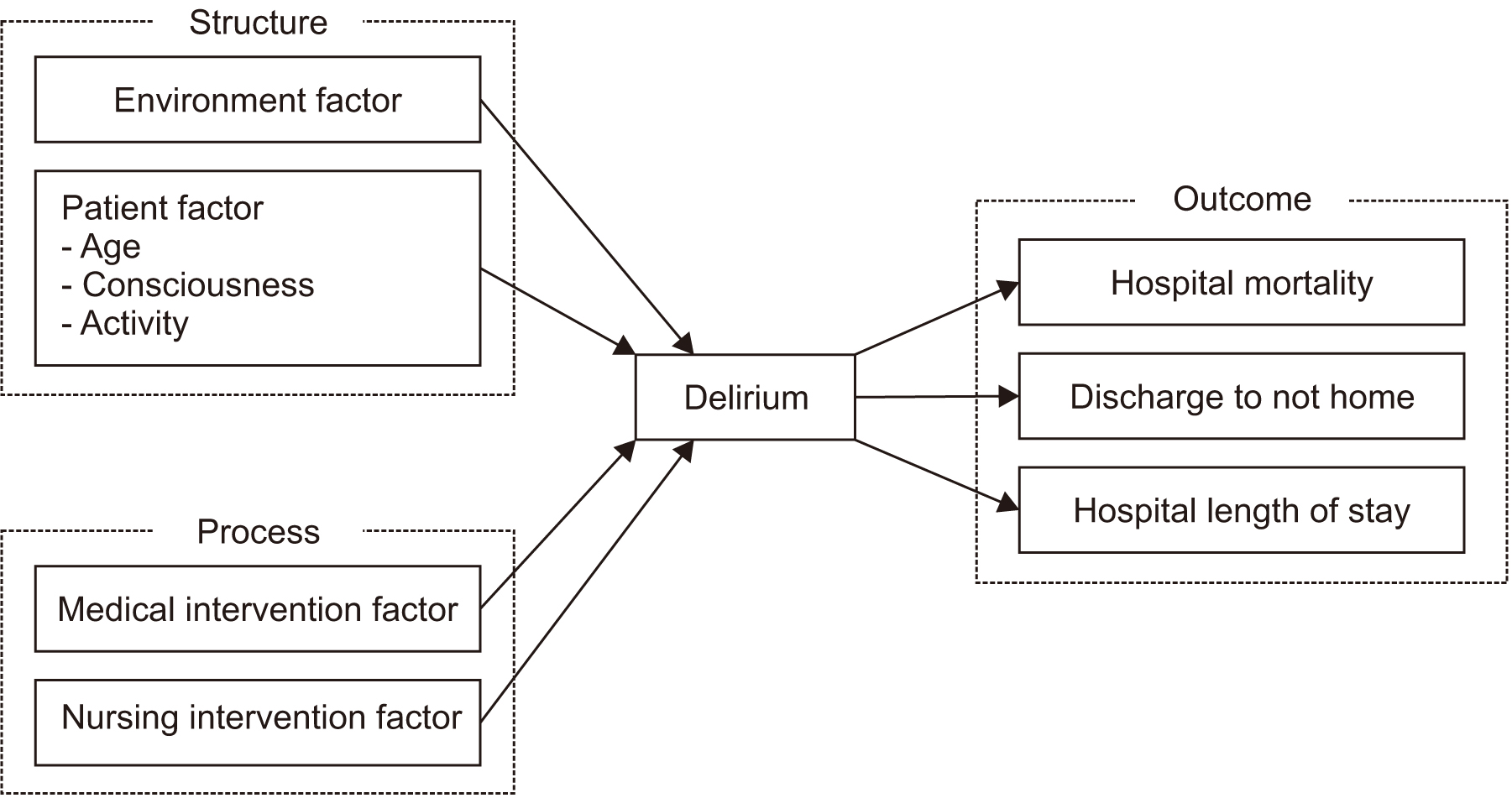
This study was conducted to investigate relationship between delirium, risk factors on delirium, and patient prognosis based on Donabedian’s structure–process–outcome model.
Methods
This study utilized a path analysis design. We extracted data from the electronic medical records containing delirium screening data. Each five hundred data in a delirium and a non-delirium group were randomly selected from electronic medical records of medical and surgical intensive care patients. Data were analyzed using SPSS 20 and AMOS 24.
Results
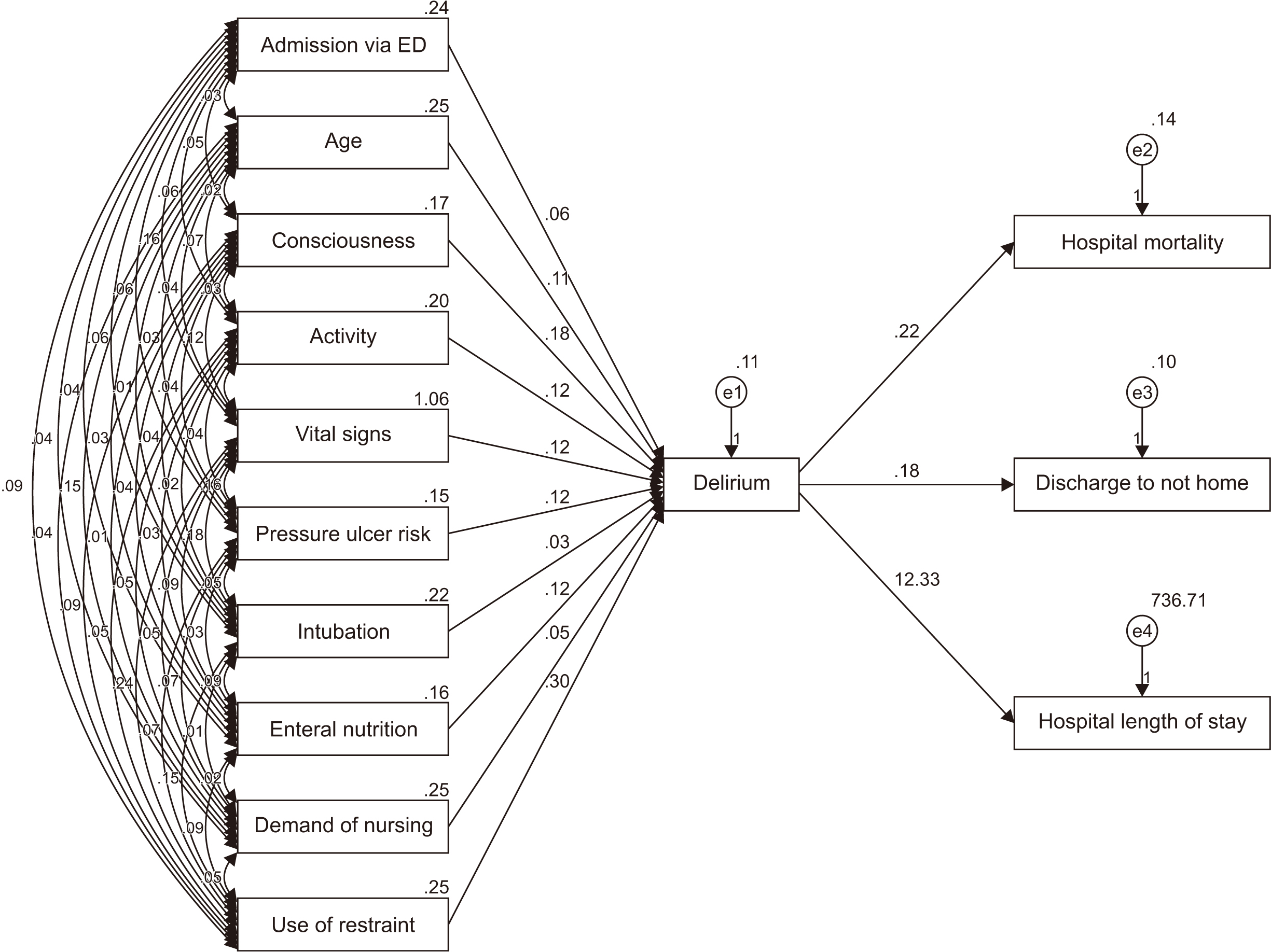
In the final model, admission via emergency department (Β=.06, p=.019), age over 65 years (Β=.11, p=.001), unconsciousness (Β=.18, p=.001), dependent activities (Β=.12, p=.001), abnormal vital signs (Β=.12, p=.001), pressure ulcer risk (Β=.12, p=.001), enteral nutrition (Β=.12, p=.001), and use of restraint (Β=.30, p=.001) directly affecting delirium accounted for 56.0% of delirium cases. Delirium had a direct effect on hospital mortality (Β=.06,p=.038), hospital length of stay (Β=5.06, p=.010), and discharge to another facility (not home) (Β=.12, p=.001), also risk factors on delirium indirectly affected patient prognosis through delirium.
Conclusion
The use of interventions to reduce delirium may improve patient prognosis. To improve the dependency activities and risk of pressure ulcers that directly affect delirium, early ambulation is encouraged, and treatment and nursing interventions to remove the ventilator and drainage tube quickly must be provided to minimize the application of restraint. Further, delirium can be prevented and patient prognosis improved through continuous intervention to stimulate cognitive awareness and monitoring of the onset of delirium. This study also discussed the effects of delirium intervention on the prognosis of patients with delirium and future research in this area.
Keyword
Figure
Reference
-
1. Moon KJ, Lee SM. Development of an evidence-based protocol for preventing delirium in intensive care unit patients. Journal of Korean Clinical Nursing Research. 2010; 16(3):175–186.2. Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell FE, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004; 291(14):1753–1762. DOI: 10.1001/jama.291.14.1753.3. van Eijk MM, van den Boogaard M, van Marum RJ, Benner P, Eikelenboom P, Honing ML, et al. Routine use of the confusion assessment method for the intensive care unit: A multicenter study. American Journal of Respiratory and Critical Care Medicine. 2011; 184(3):340–344. DOI: 10.1164/rccm.201101-0065OC.4. Reade MC, Finfer S. Sedation and delirium in the intensive care unit. The New England Journal of Medicine. 2014; 370(5):444–454. DOI: 10.1056/NEJMra1208705.5. Gusmao-Flores D, Salluh JIF, Chalhub RÁ, Quarantini LC. The confusion assessment method for the intensive care unit (CAM-ICU) and intensive care delirium screening checklist (ICDSC) for the diagnosis of delirium: A systematic review and meta-analysis of clinical studies. Critical Care (London, England). 2012; 16(4):R115. DOI: 10.1186/cc11407.6. Lee HS, Kim SS. Development of a delirium occurrence screening model for patients in medical intensive care units. Journal of Korean Clinical Nursing Research. 2013; 19(3):357–368. DOI: 10.22650/JKCNR.2013.19.3.357.7. Barr J, Fraser GL, Puntillo K, Ely EW, Gélinas C, Dasta JF, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Critical Care Medicine. 2013; 41(1):263–306. DOI: 10.1097/CCM.0b013e3182783b72.8. Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA. 1996; 275(11):852–857. DOI: 10.1001/jama.1996.03530350034031.9. Van Rompaey B, Schuurmans MJ, Shortridge-Baggett LM, Truijen S, Bossaert L. Risk factors for intensive care delirium: A systematic review. Intensive and Critical Care Nursing. 2008; 24(2):98–107. DOI: 10.1016/j.iccn.2007.08.005.10. Page V, Gough K. Management of delirium in the intensive care unit. British Journal of Hospital Medicine. 2010; 71(7):372–376. DOI: 10.12968/hmed.2010.71.7.48994.11. Jeon K, Jeong BH, Ko MG, Nam J, Yoo H, Chung CR, et al. Impact of delirium on weaning from mechanical ventilation in medical patients. Respirology. 2016; 21(2):313–320. DOI: 10.1111/resp.12673.12. Zhang Z, Pan L, Ni H. Impact of delirium on clinical outcome in critically ill patients: A meta-analysis. General Hospital Psychiatry. 2013; 35(2):105–111. DOI: 10.1016/j.genhosppsych.2012.11.003.13. van den Boogaard M, Peters SA, van der Hoeven JG, Dagnelie PC, Leffers P, Pickkers P, et al. The impact of delirium on the prediction of in-hospital mortality in intensive care patients. Critical Care (London, England). 2010; 14(4):R146. DOI: 10.1186/cc9214.14. Zaal IJ, Devlin JW, Peelen LM, Slooter AJ. A systematic review of risk factors for delirium in the ICU. Critical Care Medicine. 2015; 43(1):40–47. DOI: 10.1097/ccm.0000000000000625.15. Hsieh SJ, Soto GJ, Hope AA, Ponea A, Gong MN. The association between acute respiratory distress syndrome, delirium, and in-hospital mortality in intensive care unit patients. American Journal of Respiratory and Critical Care Medicine. 2015; 191(1):71–78. DOI: 10.1164/rccm.201409-1690OC.16. Choi SJ, Cho YA. Prevalence and related risk factors of delirium in intensive care units as detected by the CAM-ICU. Journal of Korean Clinical Nursing Research. 2014; 20(3):406–416.17. Girard TD, Shintani AK, Ely EW. Comment on “Incidence, risk factors and consequences of ICU delirium” by Ouimet et al. Intensive Care Medicine. 2007; 33(8):1479–1480. author reply 1481–1482. DOI: 10.1007/s00134-007-0698-8.18. Smulter N, Lingehall HC, Gustafson Y, Olofsson B, Engström KG. Delirium after cardiac surgery: Incidence and risk factors. Interactive Cardiovascular and Thoracic Surgery. 2013; 17(5):790–796. DOI: 10.1093/icvts/ivt323.19. Limpawattana P, Panitchote A, Tangvoraphonkchai K, Suebsoh N, Eamma W, Chanthonglarng B, et al. Delirium in critical care: A study of incidence, prevalence, and associated factors in the tertiary care hospital of older Thai adults. Aging & Mental Health. 2016; 20(1):74–80. DOI: 10.1080/13607863.2015.1035695.20. Pauley E, Lishmanov A, Schumann S, Gala GJ, van Diepen S, Katz JN. Delirium is a robust predictor of morbidity and mortality among critically ill patients treated in the cardiac intensive care unit. American Heart Journal. 2015; 170(1):79–86. DOI: 10.1016/j.ahj.2015.04.013.21. Lee EJ, Shim MY, Song SH, Lee MM, Kim HM, Kang BS, et al. Risk factors related to delirium development in patients in surgical intensive care unit. Journal of Korean Critical Care Nursing. 2010; 3(2):37–48.22. Yu MY, Park JW, Hyun MS, Lee YJ. Factors related to delirium occurrence among the patients in the intensive care units. Journal of Korean Clinical Nursing Research. 2008; 14(1):151–160.23. Salluh JIF, Wang H, Schneider EB, Nagaraja N, Yenokyan G, Damluji A, et al. Outcome of delirium in critically ill patients: Systematic review and meta-analysis. British Medical Journal. 2015; 350:h2538. DOI: 10.1136/bmj.h2538.24. Mehta S, Cook D, Devlin JW, Skrobik Y, Meade M, Fergusson D, et al. Prevalence, risk factors, and outcomes of delirium in mechanically ventilated adults. Critical Care Medicine. 2015; 43(3):557–566. DOI: 10.1097/ccm.0000000000000727.25. Donabedian A. The definition of quality and approaches to its assessment. . Ann Arbor (MI): Health Administration Press;1980. p. 1–163.26. Donabedian A. Methods for deriving criteria for assessing the quality of medical care. Medical Care Review. 1980; 37(7):653–698.27. Donabedian A. Quality assessment and assurance: Unity of purpose, diversity of means. Inquiry: A Journal of Medical Care Organization, Provision and Financing. 1988; 25(1):173–192.28. Mitchell PH, Ferketich S, Jennings BM. Quality health outcomes model. American Academy of Nursing Expert Panel on quality health care. Image: the Journal of Nursing Scholarship. 1998; 30(1):43–46.29. Jackson JC, Ely EW. The confusion assessment method (CAM). International Journal of Geriatric Psychiatry. 2003; 18(6):557–558.30. Critical Illness, Brain Dysfunction, and Survivorship (CIBS) Center. CAM-ICU Training Manual [Internet]. Nashville (TN): CIBS Center;c2008. cited 2008 June 23. Available from: http://www.icudelirium.org/docs/CAM_ICU_training_Korean.pdf.31. Yu JP. Concepts and application of structural equation modeling. Seoul: Hannarae;2016. p. 361–370.32. Siddiqi N. Credit risk scorecards: Developing and implementing intelligent credit scoring. Hoboken (NJ): John Wiley & Sons;2005. p. 78–82.33. Visser L, Prent A, van der Laan MJ, van Leeuwen BL, Izaks GJ, Zeebregts CJ, et al. Predicting postoperative delirium after vascular surgical procedures. Journal of Vascular Surgery. 2015; 62(1):183–189. DOI: 10.1016/j.jvs.2015.01.041.34. Schriger DL. Approach to the patient with abnormal vital signs. In : Cecil RL, Goldman L, Ausiello DA, editors. Cecil Textbook of Medicine. 23rd ed. Philadelphia (PA): Saunders Elsevier;2007. p. 27.35. Kline RB. Principles and practice of structural equation modeling. 2nd ed. New York: Guilford Press;2005. p. 74–77.36. Hong SH. The criteria for selecting appropriate fit indices in structural equation modeling and their rationales. Korean Journal of Clinical Psychology. 2000; 19(1):161–177.37. Moon SB. Basic concepts and applications of structural equation modeling: With AMOS19.0. Seoul: Hakjisa;2015. p. 382–383.38. van den Boogaard M, Pickkers P, Slooter AJC, Kuiper MA, Spronk PE, van der Voort PHJ, et al. Development and validation of PRE-DELIRIC (PREdiction of DELIRium in ICu patients) delirium prediction model for intensive care patients: Observational multicentre study. British Medical Journal. 2012; 344:e420. DOI: 10.1136/bmj.e420.39. Piao J, Jin Y, Lee SM. Triggers and nursing influences on delirium in intensive care units. Nursing in Critical Care. 2018; 23(1):8–15. DOI: 10.1111/nicc.12250.40. Pipanmekaporn T, Chittawatanarat K, Chaiwat O, Thawitsri T, Wacharasint P, Kongsayreepong S. Incidence and risk factors of delirium in multi-center Thai surgical intensive care units: A prospective cohort study. Journal of Intensive Care. 2015; 3:53. DOI: 10.1186/s40560-015-0118-z.41. Baik HW. Nutritional therapy in hospital. Journal of the Korean Medical Association. 2014; 57(6):491–495. DOI: 10.5124/jkma.2014.57.6.491.42. Mazzola P, Ward L, Zazzetta S, Broggini V, Anzuini A, Valcarcel B, et al. Association between preoperative malnutrition and postoperative delirium after hip fracture surgery in older adults. Journal of the American Geriatrics Society. 2017; 65(6):1222–1228. DOI: 10.1111/jgs.14764.43. Ringaitienė D, Gineitytė D, Vicka V, Žvirblis T, Šipylaitė J, Irnius A, et al. Impact of malnutrition on postoperative delirium development after on pump coronary artery bypass grafting. Journal of Cardiothoracic Surgery. 2015; 10:74. DOI: 10.1186/s13019-015-0278-x.44. Micek ST, Anand NJ, Laible BR, Shannon WD, Kollef MH. Delirium as detected by the CAM-ICU predicts restraint use among mechanically ventilated medical patients. Critical Care Medicine. 2005; 33(6):1260–1265.45. Pun BT, Ely EW. The importance of diagnosing and managing ICU delirium. Chest. 2007; 132(2):624–636. DOI: 10.1378/chest.06-1795.46. Jackson P, Khan A. Delirium in critically ill patients. Critical Care Clinics. 2015; 31(3):589–603. DOI: 10.1016/j.ccc.2015.03.011.47. Veiga D, Luis C, Parente D, Fernandes V, Botelho M, Santos P, et al. Postoperative delirium in intensive care patients: Risk factors and outcome. Brazilian Journal of Anesthesiology. 2012; 62(4):469–483. DOI: 10.1016/s0034-7094(12)70146-0.48. Sharma A, Malhotra S, Grover S, Jindal SK. Incidence, prevalence, risk factor and outcome of delirium in intensive care unit: A study from India. General Hospital Psychiatry. 2012; 34(6):639–646. DOI: 10.1016/j.genhosppsych.2012.06.009.49. Seol E, Suh YS, Ju DL, Bae HJ, Lee HJ. Characteristics and clinical course of patients who received enteral or parenteral nutrition in tertiary referral hospitals in Korea. Journal of Clinical Nutrition. 2016; 8(2):58–65. DOI: 10.15747/jcn.2016.8.2.58.50. Granberg A, Engberg IB, Lundberg D. Intensive care syndrome: A literature review. Intensive & Critical Care Nursing. 1996; 12(3):173–182. DOI: 10.1016/s0964-3397(96)80537-4.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Delirium in the intensive care unit
- Factors Influencing Intensive Care Unit Nurses’ Competency in Delirium Care in A Tertiary General Hospital
- Management of Pain, Agitation and Delirium in the Intensive Care Units
- Factors Influencing Delirium in Neurological Intensive Care Unit Patient
- Prevention and management of delirium in critically ill adult patients in the intensive care unit: a review based on the 2018 PADIS guidelines