Korean Circ J.
2020 Sep;50(9):791-800. 10.4070/kcj.2020.0037.
Early Surgery versus Watchful Waiting in Patients with Moderate Aortic Stenosis and Left Ventricular Systolic Dysfunction
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Soonchunhyang University Bucheon Hospital, Bucheon, Korea
- 2Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- 3Department of Cardiovascular Thoracic Surgery, Seoul National University Hospital, Seoul, Korea
- KMID: 2505734
- DOI: http://doi.org/10.4070/kcj.2020.0037
Abstract
- Background and Objectives
Severe aortic stenosis (AS) with left ventricular systolic dysfunction (LVSD) is a class I indication for aortic valve replacement (AVR) but this recommendation is not well established in those at the stage of moderate AS. We investigate the clinical impact of AVR among patients with moderate AS and LVSD.
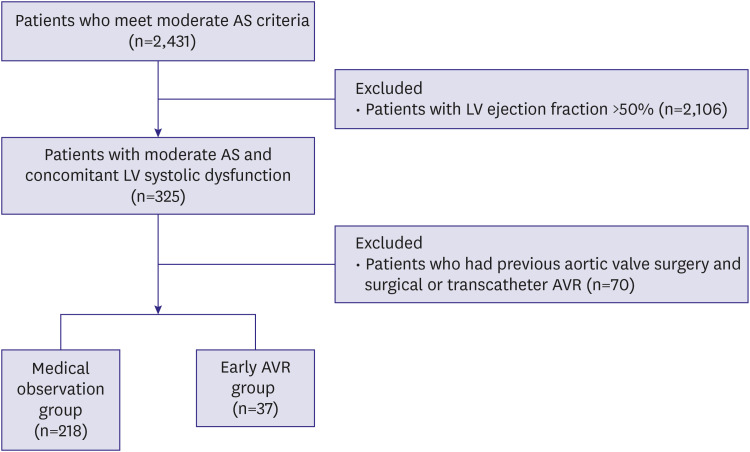
Methods
From 2001 to 2017, we consecutively identified patients with moderate AS and LVSD, defined as aortic valve area 1.0–1.5 cm2 and left ventricular ejection fraction <50%. The primary outcome was all-cause death. The outcomes were compared between those who underwent early surgical AVR (within 2 years of index echocardiography) at the stage of moderate AS versus those who were followed medically without AVR at the outpatient clinic.
Results
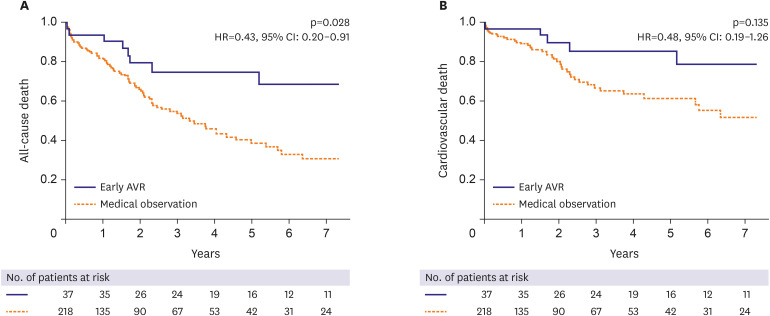
Among 255 patients (70.1±11.3 years, male 62%), 37 patients received early AVR. The early AVR group was younger than the medical observation group (63.1±7.9 vs. 71.3±11.4) with a lower prevalence of hypertension and chronic kidney disease. During a median 1.8-year follow up, 121 patients (47.5%) died, and the early AVR group showed a significantly lower all-cause death rate than the medical observation group (5.03PY vs. 18.80PY, p<0.001). After multivariable Cox-proportional hazard regression adjusting for age, sex, comorbidities, and laboratory data, early AVR at the stage of moderate AS significantly reduced the risk of death (hazard ratio, 0.43; 95% confidence interval 0.20–0.91; p=0.028).
Conclusions
In patients with moderate AS and LVSD, AVR reduces the risk of all-cause death. A prospective randomized trial is warranted to confirm our findings.
Figure
Cited by 3 articles
-
Moderate Aortic Valve Stenosis with Left Ventricular Systolic Dysfunction: Potential Role of Early Aortic Valve Replacement
Ju-Hee Lee
Korean Circ J. 2020;50(9):801-803. doi: 10.4070/kcj.2020.0301.Long-term Prognosis of Mild to Moderate Aortic Stenosis and Coronary Artery Disease
Wonjae Lee, Wonsuk Choi, Si-Hyuck Kang, In-Chang Hwang, Hong-Mi Choi, Yeonyee E. Yoon, Goo-Yeong Cho
J Korean Med Sci. 2021;36(6):e47. doi: 10.3346/jkms.2021.36.e47.Expanding Role of Left Atrial Strain in Valvular Heart Disease
Jah Yeon Choi
Korean Circ J. 2022;52(3):218-219. doi: 10.4070/kcj.2022.0004.
Reference
-
1. Osnabrugge RL, Mylotte D, Head SJ, et al. Aortic stenosis in the elderly: disease prevalence and number of candidates for transcatheter aortic valve replacement: a meta-analysis and modeling study. J Am Coll Cardiol. 2013; 62:1002–1012. PMID: 23727214.2. Baumgartner H, Falk V, Bax JJ, et al. 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2017; 38:2739–2791. PMID: 28886619.3. Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2014; 63:e57–185. PMID: 24603191.4. Ito S, Pislaru C, Miranda WR, et al. Left ventricular contractility and wall stress in patients with aortic stenosis with preserved or reduced ejection fraction. JACC Cardiovasc Imaging. 2020; 13:357–369. PMID: 30878438.5. Strange G, Stewart S, Celermajer D, et al. Poor long-term survival in patients with moderate aortic stenosis. J Am Coll Cardiol. 2019; 74:1851–1863. PMID: 31491546.
Article6. van Gils L, Clavel MA, Vollema EM, et al. Prognostic implications of moderate aortic stenosis in patients with left ventricular systolic dysfunction. J Am Coll Cardiol. 2017; 69:2383–2392. PMID: 28494976.7. B Bastos M, Schreuder JJ, Daemen J, Van Mieghem NM. Hemodynamic effects of transcatheter aortic valve replacement for moderate aortic stenosis with reduced left ventricular ejection fraction. JACC Cardiovasc Interv. 2019; 12:684–686. PMID: 30878476.8. Narang N, Lang RM, Liarski VM, Jeevanandam V, Hofmann Bowman MA. Aortic valve replacement for moderate aortic stenosis with severe calcification and left ventricualr dysfunction-a case report and review of the literature. Front Cardiovasc Med. 2017; 4:14. PMID: 28396860.
Article9. Mitchell C, Rahko PS, Blauwet LA, et al. Guidelines for performing a comprehensive transthoracic echocardiographic examination in adults: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. 2019; 32:1–64. PMID: 30282592.
Article10. Gillinov AM, Garcia MJ. When is concomitant aortic valve replacement indicated in patients with mild to moderate stenosis undergoing coronary revascularization? Curr Cardiol Rep. 2005; 7:101–104. PMID: 15717955.
Article11. Pereira JJ, Balaban K, Lauer MS, Lytle B, Thomas JD, Garcia MJ. Aortic valve replacement in patients with mild or moderate aortic stenosis and coronary bypass surgery. Am J Med. 2005; 118:735–742. PMID: 15989907.
Article12. Smith WT 4th, Ferguson TB Jr, Ryan T, Landolfo CK, Peterson ED. Should coronary artery bypass graft surgery patients with mild or moderate aortic stenosis undergo concomitant aortic valve replacement? A decision analysis approach to the surgical dilemma. J Am Coll Cardiol. 2004; 44:1241–1247. PMID: 15364326.
Article13. Mosterd A, Hoes AW. Clinical epidemiology of heart failure. Heart. 2007; 93:1137–1146. PMID: 17699180.
Article14. Pibarot P, Messika-Zeitoun D, Ben-Yehuda O, et al. Moderate aortic stenosis and heart failure with reduced ejection fraction: can imaging guide us to therapy? JACC Cardiovasc Imaging. 2019; 12:172–184. PMID: 30621989.15. Alter P, Koczulla AR, Nell C, Figiel JH, Vogelmeier CF, Rominger MB. Wall stress determines systolic and diastolic function--characteristics of heart failure. Int J Cardiol. 2016; 202:685–693. PMID: 26454537.16. Feygin J, Hu Q, Swingen C, Zhang J. Relationships between regional myocardial wall stress and bioenergetics in hearts with left ventricular hypertrophy. Am J Physiol Heart Circ Physiol. 2008; 294:H2313–H2321. PMID: 18326803.
Article17. Ng AC, Delgado V, Bertini M, et al. Alterations in multidirectional myocardial functions in patients with aortic stenosis and preserved ejection fraction: a two-dimensional speckle tracking analysis. Eur Heart J. 2011; 32:1542–1550. PMID: 21447510.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Early Surgery in Valvular Heart Disease
- Moderate Aortic Valve Stenosis with Left Ventricular Systolic Dysfunction: Potential Role of Early Aortic Valve Replacement
- Multimodality Imaging for the Assessment of Severe Aortic Stenosis
- Multiplane Transesophageal Echocardiographic Findings of Two Cases of Discrete Subvalvular Aortic Stenosis
- Alterations in Left ventricular End-systolic Wall Stress During Short-term Follow-up After Correction of Isolated Congenital Aortic Stenosis