Korean Circ J.
2018 Nov;48(11):964-973. 10.4070/kcj.2018.0308.
Early Surgery in Valvular Heart Disease
- Affiliations
-
- 1Division of Cardiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. dhkang@amc.seoul.kr
- KMID: 2422544
- DOI: http://doi.org/10.4070/kcj.2018.0308
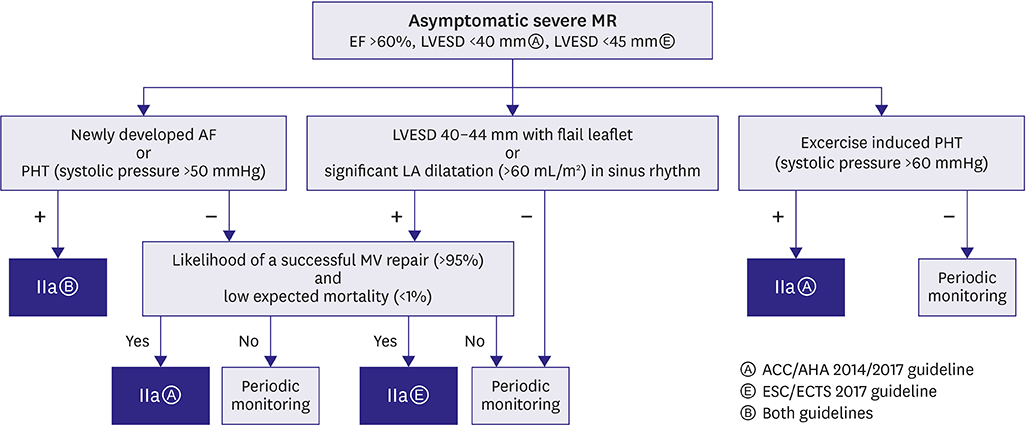
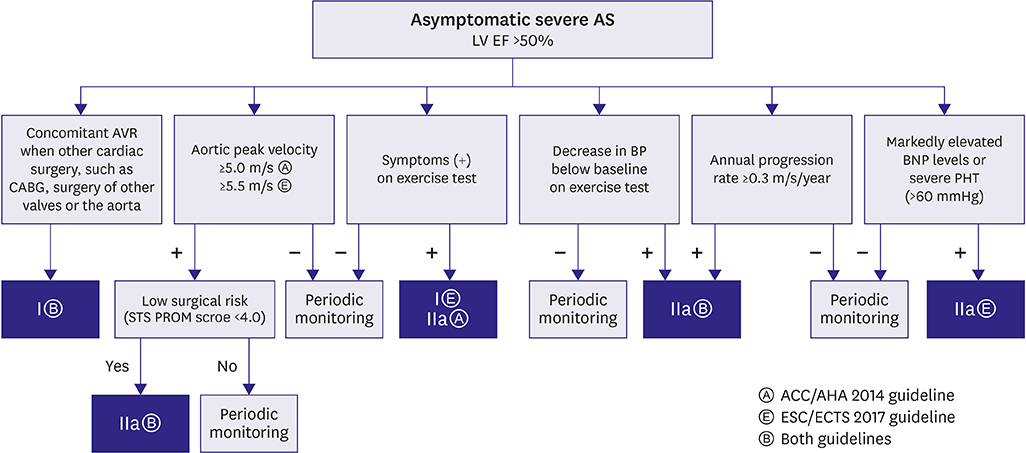
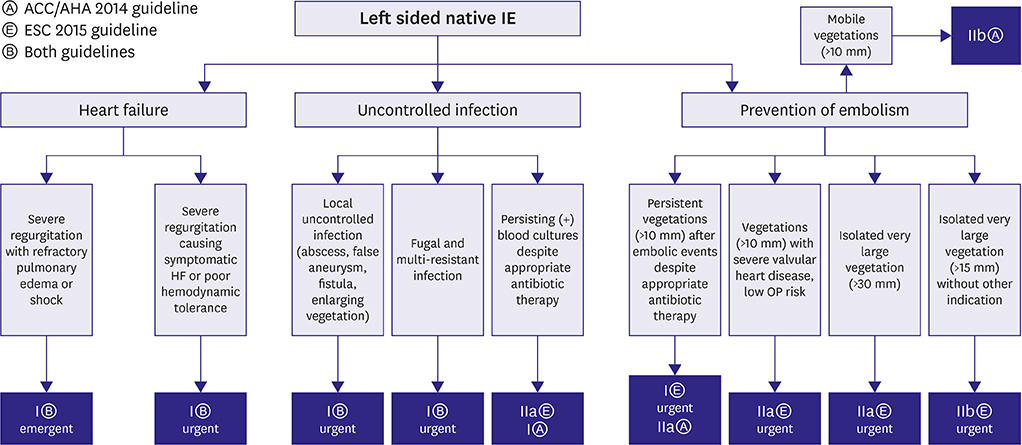
Abstract
- The burden of valvular heart disease (VHD) is increasing with age, and the elderly patients with moderate or severe VHD are notably common. When to operate in asymptomatic patients with VHD remains controversial. The controversy is whether early surgical intervention should be preferred, or a watchful waiting approach should be followed. The beneficial effects of early surgery should be balanced against operative mortality and long-term results. Indications of early surgery in each of the VHD will be discussed in this review on the basis of the latest American and European guidelines.
Keyword
MeSH Terms
Figure
Reference
-
1. Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart diseases: a population-based study. Lancet. 2006; 368:1005–1011.
Article2. Iung B, Vahanian A. Epidemiology of valvular heart disease in the adult. Nat Rev Cardiol. 2011; 8:162–172.
Article3. Benjamin EJ, Virani SS, Callaway CW, et al. Heart disease and stroke statistics-2018 update: a report from the American Heart Association. Circulation. 2018; 137:e67–e492.
Article4. Enriquez-Sarano M, Avierinos JF, Messika-Zeitoun D, et al. Quantitative determinants of the outcome of asymptomatic mitral regurgitation. N Engl J Med. 2005; 352:875–883.
Article5. Kang DH, Kim JH, Rim JH, et al. Comparison of early surgery versus conventional treatment in asymptomatic severe mitral regurgitation. Circulation. 2009; 119:797–804.
Article6. Kang DH, Park SJ, Sun BJ, et al. Early surgery versus conventional treatment for asymptomatic severe mitral regurgitation: a propensity analysis. J Am Coll Cardiol. 2014; 63:2398–2407.7. Suri RM, Vanoverschelde JL, Grigioni F, et al. Association between early surgical intervention vs watchful waiting and outcomes for mitral regurgitation due to flail mitral valve leaflets. JAMA. 2013; 310:609–616.
Article8. Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. J Thorac Cardiovasc Surg. 2014; 148:e1–e132.9. Baumgartner H, Falk V, Bax JJ, et al. 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2017; 38:2739–2791.10. Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 2017; 70:252–289.11. Le Tourneau T, Richardson M, Juthier F, et al. Echocardiography predictors and prognostic value of pulmonary artery systolic pressure in chronic organic mitral regurgitation. Heart. 2010; 96:1311–1317.
Article12. La Canna G, Arendar I, Maisano F, et al. Real-time three-dimensional transesophageal echocardiography for assessment of mitral valve functional anatomy in patients with prolapse-related regurgitation. Am J Cardiol. 2011; 107:1365–1374.
Article13. Ross J Jr, Braunwald E. Aortic stenosis. Circulation. 1968; 38:Suppl. 61–67.
Article14. Pellikka PA, Sarano ME, Nishimura RA, et al. Outcome of 622 adults with asymptomatic, hemodynamically significant aortic stenosis during prolonged follow-up. Circulation. 2005; 111:3290–3295.
Article15. Edwards FH, Peterson ED, Coombs LP, et al. Prediction of operative mortality after valve replacement surgery. J Am Coll Cardiol. 2001; 37:885–892.
Article16. Rosenhek R, Binder T, Porenta G, et al. Predictors of outcome in severe, asymptomatic aortic stenosis. N Engl J Med. 2000; 343:611–617.
Article17. Pai RG, Kapoor N, Bansal RC, Varadarajan P. Malignant natural history of asymptomatic severe aortic stenosis: benefit of aortic valve replacement. Ann Thorac Surg. 2006; 82:2116–2122.
Article18. Kang DH, Park SJ, Rim JH, et al. Early surgery versus conventional treatment in asymptomatic very severe aortic stenosis. Circulation. 2010; 121:1502–1509.
Article19. Taniguchi T, Morimoto T, Shiomi H, et al. Initial surgical versus conservative strategies in patients with asymptomatic severe aortic stenosis. J Am Coll Cardiol. 2015; 66:2827–2838.20. Généreux P, Stone GW, O'Gara PT, et al. Natural history, diagnostic approaches, and therapeutic strategies for patients with asymptomatic severe aortic stenosis. J Am Coll Cardiol. 2016; 67:2263–2288.
Article21. Pellikka PA, Nishimura RA, Bailey KR, Tajik AJ. The natural history of adults with asymptomatic, hemodynamically significant aortic stenosis. J Am Coll Cardiol. 1990; 15:1012–1017.
Article22. Lim WY, Ramasamy A, Lloyd G, Bhattacharyya S. Meta-analysis of the impact of intervention versus symptom-driven management in asymptomatic severe aortic stenosis. Heart. 2017; 103:268–272.
Article23. The United States National Library of Medicine. Early surgery versus conventional treatment in very severe aortic stenosis [Internet]. Bethesda (MD): The United States National Library of Medicine;2018. July. cited 2018 Oct 5. Available from: https://ClinicalTrials.gov/show/NCT01161732.24. Banovic M, Iung B, Bartunek J, et al. Rationale and design of the Aortic Valve replAcemenT versus conservative treatment in Asymptomatic seveRe aortic stenosis (AVATAR trial): a randomized multicenter controlled event-driven trial. Am Heart J. 2016; 174:147–153.
Article25. Bonow RO, Lakatos E, Maron BJ, Epstein SE. Serial long-term assessment of the natural history of asymptomatic patients with chronic aortic regurgitation and normal left ventricular systolic function. Circulation. 1991; 84:1625–1635.
Article26. de Meester C, Gerber BL, Vancraeynest D, et al. Early surgical intervention versus watchful waiting and outcomes for asymptomatic severe aortic regurgitation. J Thorac Cardiovasc Surg. 2015; 150:1100–1108.
Article27. Murdoch DR, Corey GR, Hoen B, et al. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the international collaboration on endocarditis-prospective cohort study. Arch Intern Med. 2009; 169:463–473.28. Kang DH. Timing of surgery in infective endocarditis. Heart. 2015; 101:1786–1791.
Article29. Tornos P, Iung B, Permanyer-Miralda G, et al. Infective endocarditis in Europe: lessons from the Euro heart survey. Heart. 2005; 91:571–575.
Article30. Prendergast BD, Tornos P. Surgery for infective endocarditis: who and when? Circulation. 2010; 121:1141–1152.31. Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC guidelines for the management of infective endocarditis: the task force for the management of infective endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015; 36:3075–3128.32. D'Agostino RB Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998; 17:2265–2281.33. Vikram HR, Buenconsejo J, Hasbun R, Quagliarello VJ. Impact of valve surgery on 6-month mortality in adults with complicated, left-sided native valve endocarditis: a propensity analysis. JAMA. 2003; 290:3207–3214.34. Kiefer T, Park L, Tribouilloy C, et al. Association between valvular surgery and mortality among patients with infective endocarditis complicated by heart failure. JAMA. 2011; 306:2239–2247.
Article35. López J, Sevilla T, Vilacosta I, et al. Prognostic role of persistent positive blood cultures after initiation of antibiotic therapy in left-sided infective endocarditis. Eur Heart J. 2013; 34:1749–1754.
Article36. Leung DY, Cranney GB, Hopkins AP, Walsh WF. Role of transoesophageal echocardiography in the diagnosis and management of aortic root abscess. Br Heart J. 1994; 72:175–181.
Article37. Anguera I, Miro JM, Vilacosta I, et al. Aorto-cavitary fistulous tract formation in infective endocarditis: clinical and echocardiographic features of 76 cases and risk factors for mortality. Eur Heart J. 2005; 26:288–297.
Article38. Mylonakis E, Calderwood SB. Infective endocarditis in adults. N Engl J Med. 2001; 345:1318–1330.
Article39. Dickerman SA, Abrutyn E, Barsic B, et al. The relationship between the initiation of antimicrobial therapy and the incidence of stroke in infective endocarditis: an analysis from the ICE Prospective Cohort Study (ICE-PCS). Am Heart J. 2007; 154:1086–1094.
Article40. García-Cabrera E, Fernández-Hidalgo N, Almirante B, et al. Neurological complications of infective endocarditis: risk factors, outcome, and impact of cardiac surgery: a multicenter observational study. Circulation. 2013; 127:2272–2284.41. Delahaye F. Is early surgery beneficial in infective endocarditis? a systematic review. Arch Cardiovasc Dis. 2011; 104:35–44.
Article42. Kim DH, Kang DH, Lee MZ, et al. Impact of early surgery on embolic events in patients with infective endocarditis. Circulation. 2010; 122:Suppl. S17–S22.
Article43. Kang DH, Kim YJ, Kim SH, et al. Early surgery versus conventional treatment for infective endocarditis. N Engl J Med. 2012; 366:2466–2473.
Article44. Kang DH, Lee S, Kim YJ, et al. Long-term results of early surgery versus conventional treatment for infective endocarditis trial. Korean Circ J. 2016; 46:846–850.
Article45. King RM, Schaff HV, Danielson GK, et al. Surgery for tricuspid regurgitation late after mitral valve replacement. Circulation. 1984; 70:I193–I197.46. Staab ME, Nishimura RA, Dearani JA. Isolated tricuspid valve surgery for severe tricuspid regurgitation following prior left heart valve surgery: analysis of outcome in 34 patients. J Heart Valve Dis. 1999; 8:567–574.