Neonatal Med.
2020 Aug;27(3):105-110. 10.5385/nm.2020.27.3.105.
Sedation for Brain Magnetic Resonance Imaging in Preterm Infants: Using Propofol under Anesthesiologist Supervision
- Affiliations
-
- 1Department of Pediatrics, Hallym University Kangnam Sacred Heart Hospital, Seoul, Korea
- 2Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2505660
- DOI: http://doi.org/10.5385/nm.2020.27.3.105
Abstract
- Purpose
We aimed to compare two different sedation protocols for brain magnetic resonance imaging (MRI) in preterm infants. One protocol used chloral hydrate (CH) with monitoring conducted by non-anesthesiologists, and the other used a continuous infusion of propofol (PF) with monitoring by anesthesiologists.
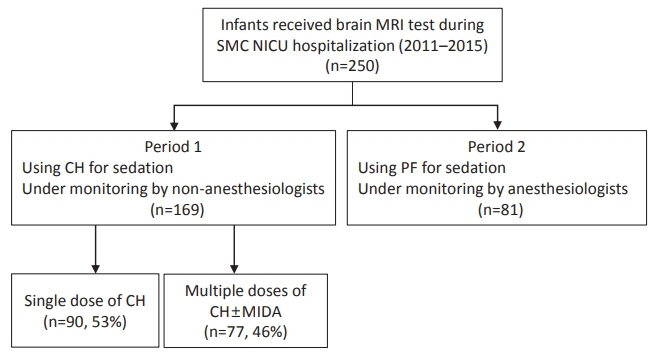
Methods
A total of 250 preterm infants born between January 2011 and December 2015 who received brain MRI during hospitalization in our neonatal intensive care unit (NICU) were included in this retrospective study. In period 1, sedation for brain MRI was done using a single dose or multiple doses of CH with monitoring conducted by NICU medical staff. In period 2, an anesthesiologist prescribed a continuous infusion of PF and titrated the dosage for minimal and adequate sedation. Data on the adverse events, including desaturation and bradycardia, were collected and compared between periods 1 and 2.
Results
Despite similar gestational ages of the patients in periods 1 and 2, the infants in period 1 showed a higher risk of developing bradycardia after sedation compared to those in period 2 (30.2% vs. 14.8%; an adjusted odds ratio of 2.35; 95% confidence interval of 1.12 to 4.91). Infants who had an adverse event after sedation had a lower gestational age and corrected age at the time of MRI (26.8 weeks vs. 27.9 weeks, P=0.004; 37.3 weeks vs. 38.3 weeks, P=0.023). The duration of MRI was significantly longer in infants that had an adverse event than those that did not (70.9 minutes vs. 64.3 minutes). After adjusting for various clinical factors, lower gestational age, lower corrected age at the time of MRI, and period 1 increased the risk of developing adverse events after sedation for MRI.
Conclusion
The use of a continuous PF infusion with dose titration and monitoring by an anesthesiologist is safe and feasible as a sedation protocol for brain MRI in prematurely born infants.
Figure
Reference
-
1. Slaughter LA, Bonfante-Mejia E, Hintz SR, Dvorchik I, Parikh NA. Early conventional MRI for prediction of neurodevelopmental impairment in extremely-low-birth-weight infants. Neonatology. 2016; 110:47–54.2. Pennock JM. Patient preparation, safety and hazards in imaging infants and children. In : Rutherford M, editor. MRI of the neonatal brain. London: W.B. Saunders;2002. p. 3–15.3. Hall RW, Shbarou RM. Drugs of choice for sedation and analgesia in the neonatal ICU. Clin Perinatol. 2009; 36:15–26.4. Litman RS, Soin K, Salam A. Chloral hydrate sedation in term and preterm infants: an analysis of efficacy and complications. Anesth Analg. 2010; 110:739–46.5. Finnemore A, Toulmin H, Merchant N, Arichi T, Tusor N, Cox D, et al. Chloral hydrate sedation for magnetic resonance imaging in newborn infants. Paediatr Anaesth. 2014; 24:190–5.6. Pershad J, Palmisano P, Nichols M. Chloral hydrate: the good and the bad. Pediatr Emerg Care. 1999; 15:432–5.7. Rigby-Jones AE, Nolan JA, Priston MJ, Wright PM, Sneyd JR, Wolf AR. Pharmacokinetics of propofol infusions in critically ill neonates, infants, and children in an intensive care unit. Anesthesiology. 2002; 97:1393–400.8. Machata AM, Willschke H, Kabon B, Kettner SC, Marhofer P. Propofol-based sedation regimen for infants and children undergoing ambulatory magnetic resonance imaging. Br J Anaesth. 2008; 101:239–43.9. Pershad J, Wan J, Anghelescu DL. Comparison of propofol with pentobarbital/midazolam/fentanyl sedation for magnetic resonance imaging of the brain in children. Pediatrics. 2007; 120:e629–36.10. Arthurs OJ, Sury M. Anaesthesia or sedation for paediatric MRI: advantages and disadvantages. Curr Opin Anaesthesiol. 2013; 26:489–94.11. Allegaert K, Daniels H, Naulaers G, Tibboel D, Devlieger H. Pharmacodynamics of chloral hydrate in former preterm infants. Eur J Pediatr. 2005; 164:403–7.12. Smallman B. Pediatric sedation: can it be safely performed by non-anesthesiologists? Curr Opin Anaesthesiol. 2002; 15:455–9.13. Chiaretti A, Benini F, Pierri F, Vecchiato K, Ronfani L, Agosto C, et al. Safety and efficacy of propofol administered by paediatricians during procedural sedation in children. Acta Paediatr. 2014; 103:182–7.14. Krauss BS, Krauss BA, Green SM. Procedural sedation and analgesia in children. N Engl J Med. 2014; 371:91.15. Cook-Sather SD, Litman RS. Modern fasting guidelines in children. Best Pract Res Clin Anaesthesiol. 2006; 20:471–81.16. Choi YS, Son YJ, Song ES, Cho YK, Kim YO, Kim CJ, et al. Effect of chloral hydrate used for pediatric sedation. J Korean Child Neurol Soc. 2008; 16:78–85.17. Delgado J, Toro R, Rascovsky S, Arango A, Angel GJ, Calvo V, et al. Chloral hydrate in pediatric magnetic resonance imaging:evaluation of a 10-year sedation experience administered by radiologists. Pediatr Radiol. 2015; 45:108–14.18. Allegaert K. The clinical pharmacology of short acting analgosedatives in neonates. Curr Clin Pharmacol. 2011; 6:222–6.19. Welzing L, Kribs A, Eifinger F, Huenseler C, Oberthuer A, Roth B. Propofol as an induction agent for endotracheal intubation can cause significant arterial hypotension in preterm neonates. Paediatr Anaesth. 2010; 20:605–11.20. Dalal PG, Murray D, Cox T, McAllister J, Snider R. Sedation and anesthesia protocols used for magnetic resonance imaging studies in infants: provider and pharmacologic considerations. Anesth Analg. 2006; 103:863–8.21. Cravero JP, Blike GT, Beach M, Gallagher SM, Hertzog JH, Havidich JE, et al. Incidence and nature of adverse events during pediatric sedation/anesthesia for procedures outside the operating room: report from the pediatric sedation research consortium. Pediatrics. 2006; 118:1087–96.22. Allegaert K, Peeters MY, Verbesselt R, Tibboel D, Naulaers G, de Hoon JN, et al. Inter-individual variability in propofol pharmacokinetics in preterm and term neonates. Br J Anaesth. 2007; 99:864–70.23. Havidich JE, Beach M, Dierdorf SF, Onega T, Suresh G, Cravero JP. Preterm versus term children: analysis of sedation/anesthesia adverse events and longitudinal risk. Pediatrics. 2016; 137:e20150463.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Procedural Sedation of Preterm Neonate with Frequent Apnea during Magnetic Resonance Imaging: A Case Report
- Repeated Sedation with Intravenous Propofol in a Brain Tumor Patient during ConsecutiveRadiation Therapy : A case report
- Endoscopist-Directed Propofol: Pros and Cons
- Sedation for Pediatric Patients Undergoing MRI
- Sedation using 5% lidocaine patches, midazolam and propofol in a combative, obese adolescent with severe autistic disorder undergoing brain magnetic resonance imaging: a case report