J Korean Med Sci.
2020 Aug;35(33):e279. 10.3346/jkms.2020.35.e279.
Epidemiological Study of Hereditary Hemolytic Anemia in the Korean Pediatric Population during 1997–2016: a Nationwide Retrospective Cohort Study
- Affiliations
-
- 1Department of Pediatrics, Keimyung University School of Medicine, Keimyung University Dongsan Medical Center, Daegu, Korea
- 2Deparment of Pediatrics, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Department of Pediatrics, Seoul National University College of Medicine, Seoul National University Cancer Research Institute, Seoul National University Children's Hospital, Seoul, Korea
- 4Department of Pediatrics, Daegu Fatima Hospital, Daegu, Korea
- 5Department of Pediatrics, Yeungnam University College of Medicine, Daegu, Korea
- 6Department of Pediatrics, Pusan National University School of Medicine, Pusan National University Children's Hospital, Yangsan, Korea
- 7Department of Pediatrics, Chonnam National University Hwasun Hospital, Chonnam National University Medical School, Gwangju, Korea
- 8Department of Pediatrics, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 9Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 10Department of Pediatrics, Ajou University School of Medicine, Suwon, Korea
- 11Department of Pediatrics, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 12Department of Pediatrics, School of Medicine, Kyungpook National University, Kyungpook National University Hospital, Daegu, Korea
- 13Department of Pediatrics, Gyeongsang National University College of Medicine, Gyeongsang National University Hospital, Jinju, Korea
- 14Department of Pediatrics, University of Ulsan College of Medicine, Asan Medical Center Children's Hospital, Seoul, Korea
- 15Department of Pediatrics, Dong-A University College of Medicine, Busan, Korea
- 16Department of Pediatrics, Inha University Hospital, Incheon, Korea
- 17Department of Pediatrics, Chosun University Hospital, Gwangju, Korea
- 18Department of Pediatrics, Ewha Womans University College of Medicine, Ewha Womans University Seoul Hospital, Seoul, Korea
- 19Department of Pediatrics, Center for Pediatric Cancer, National Cancer Center, Goyang, Korea
- 20Department of Pediatrics, Jeju National University Hospital, Jeju National University School of Medicine, Jeju, Korea
- 21Department of Pediatrics, Inje University College of Medicine, Busan Paik Hospital, Busan, Korea
- 22Department of Pediatrics, Cha Bundang Medical Center, Cha University, Seongnam, Korea
- 23Department of Pediatrics, University of Ulsan College of Medicine, Ulsan University Hospital, Ulsan, Korea
- 24Department of Pediatrics, Hanyang University Seoul Hospital, Seoul, Korea
- 25Department of Pediatrics, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- 26Department of Pediatrics, Daegu Catholic University School of Medicine, Daegu, Korea
- 27Department of Pediatrics, Kosin University College of Medicine, Kosin University Gospel Hospital, Busan, Korea
- KMID: 2505595
- DOI: http://doi.org/10.3346/jkms.2020.35.e279
Abstract
- Background
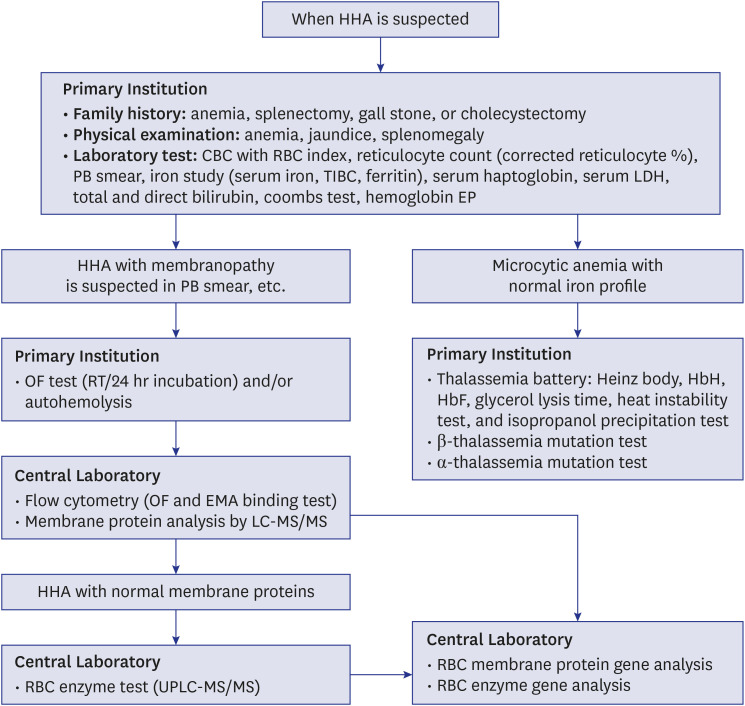
Hereditary hemolytic anemia (HHA) is a rare disease characterized by premature red blood cell (RBC) destruction due to intrinsic RBC defects. The RBC Disorder Working Party of the Korean Society of Hematology established and updated the standard operating procedure for making an accurate diagnosis of HHA since 2007. The aim of this study was to investigate a nationwide epidemiology of Korean HHA.
Methods
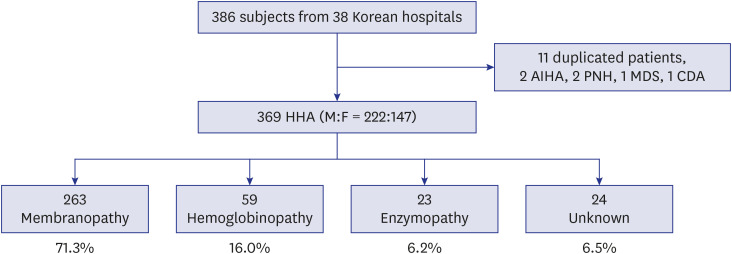
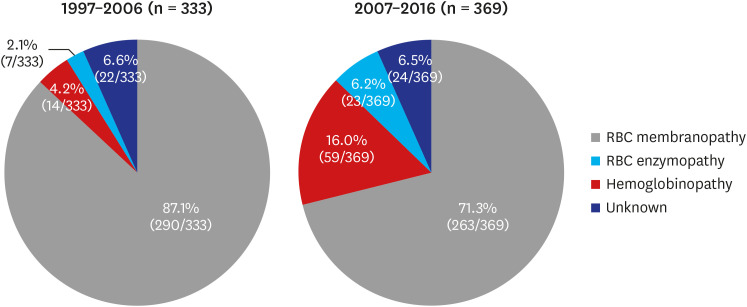
We collected the data of a newly diagnosed pediatric HHA cohort (2007–2016) and compared this cohort's characteristics with those of a previously surveyed pediatric HHA cohort (1997–2006) in Korea. Each participant's information was retrospectively collected by a questionnaire survey.
Results
A total of 369 children with HHA from 38 hospitals distributed in 16 of 17 districts of Korea were investigated. RBC membranopathies, hemoglobinopathies, RBC enzymopathies, and unknown etiologies accounted for 263 (71.3%), 59 (16.0%), 23 (6.2%), and 24 (6.5%) of the cases, respectively. Compared to the cohort from the previous decade, the proportions of hemoglobinopathies and RBC enzymopathies significantly increased (P < 0.001 and P = 0.008, respectively). Twenty-three of the 59 hemoglobinopathy patients had immigrant mothers, mostly from South-East Asia.
Conclusion
In Korea, thalassemia traits have increased over the past 10 years, reflecting both increased awareness of this disease and increased international marriages. The enhanced recognition of RBC enzymopathies is due to advances in diagnostic technique; however, 6.5% of HHA patients still do not have a clear diagnosis. It is necessary to improve accessibility of diagnosing HHA.
Keyword
Figure
Cited by 1 articles
-
Korean clinical practice guidelines for the diagnosis of hereditary hemolytic anemia
Hee Won Chueh, Sang Mee Hwang, Ye Jee Shim, Jae Min Lee, Hee Sue Park, Joon Hee Lee, Youngwon Nam, Namhee Kim, Hye Lim Jung, Hyoung Soo Choi, on behalf of Korean RBC Disorder Working Party
Blood Res. 2022;57(2):86-94. doi: 10.5045/br.2022.2021224.
Reference
-
1. Haley K. Congenital hemolytic anemia. Med Clin North Am. 2017; 101(2):361–374. PMID: 28189176.
Article2. Chueh HW. Treatment and management of late complications in hereditary hemolytic anemia. Clin Pediatr Hematol Oncol. 2016; 23(1):1–7.
Article3. Cho HS, Hah JO, Kang IJ, Kang HJ, Kwak JY, Koo HH, et al. Hereditary hemolytic anemia in Korea: a retrospective study from 1997 to 2006. Korean J Hematol. 2007; 42(3):197–205.
Article4. Angastiniotis M, Modell B. Global epidemiology of hemoglobin disorders. Ann N Y Acad Sci. 1998; 850:251–269. PMID: 9668547.
Article5. Jung HL. A new paradigm in the diagnosis of hereditary hemolytic anemia. Blood Res. 2013; 48(4):237–239. PMID: 24466544.
Article6. Lee YK, Kim HJ, Lee K, Park SH, Song SH, Seong MW, et al. Recent progress in laboratory diagnosis of thalassemia and hemoglobinopathy: a study by the Korean Red Blood Cell Disorder Working Party of the Korean Society of Hematology. Blood Res. 2019; 54(1):17–22. PMID: 30956959.
Article7. Park SH, Park CJ, Lee BR, Cho YU, Jang S, Kim N, et al. Comparison study of the eosin-5′-maleimide binding test, flow cytometric osmotic fragility test, and cryohemolysis test in the diagnosis of hereditary spherocytosis. Am J Clin Pathol. 2014; 142(4):474–484. PMID: 25239414.
Article8. Shim YJ, Won DI. Flow cytometric osmotic fragility testing does reflect the clinical severity of hereditary spherocytosis. Cytometry B Clin Cytom. 2014; 86(6):436–443. PMID: 24243866.
Article9. Won DI, Suh JS. Flow cytometric detection of erythrocyte osmotic fragility. Cytometry B Clin Cytom. 2009; 76(2):135–141. PMID: 18727072.
Article10. Aguilar Martinez P, Angastiniotis M, Eleftheriou A, Gulbis B, Mañú Pereira MM, Petrova-Benedict R, et al. Haemoglobinopathies in Europe: health & migration policy perspectives. Orphanet J Rare Dis. 2014; 9(1):97. PMID: 24980780.11. Angastiniotis M, Vives Corrons JL, Soteriades ES, Eleftheriou A. The impact of migrations on the health services for rare diseases in Europe: the example of haemoglobin disorders. Sci World J. 2013; 2013:727905.
Article12. Venturelli D, Lodi M, Palazzi G, Bergonzini G, Doretto G, Zini A, et al. Sickle cell disease in areas of immigration of high-risk populations: a low cost and reproducible method of screening in northern Italy. Blood Transfus. 2014; 12(3):346–351. PMID: 24887233.13. Kim YP, Joh JY, Shin IS. Family function of the families consisting of Asian immigrant women living in South Korea: a 3-year longitudinal study. Asia Pac J Public Health. 2015; 27(2):NP2702–11. PMID: 22652245.14. Kim YP, Kim S, Joh JY. Family adaptability and cohesion in families consisting of Asian immigrant women living in South Korea: a 3-year longitudinal study. Asia-Pac Psychiatry. 2015; 7(2):206–214. PMID: 23857754.
Article15. Choi HS, Choi Q, Kim JA, Im KO, Park SN, Park Y, et al. Molecular diagnosis of hereditary spherocytosis by multi-gene target sequencing in Korea: matching with osmotic fragility test and presence of spherocyte. Orphanet J Rare Dis. 2019; 14(1):114. PMID: 31122244.
Article16. Park ES, Jung HL, Kim HJ, Park SS, Bae SH, Shin HY, et al. Hereditary hemolytic anemia in Korea from 2007 to 2011: a study by the Korean Hereditary Hemolytic Anemia Working Party of the Korean Society of Hematology. Blood Res. 2013; 48(3):211–216. PMID: 24086942.
Article17. Korean Statistical Information Service. Updated 2019. Accessed January 15, 2019. https://kosis.kr.18. Hong CR, Kang HJ, Lee JW, Kim H, Kim NH, Park KD, et al. Clinical characteristics of pediatric thalassemia in Korea: a single institute experience. J Korean Med Sci. 2013; 28(11):1645–1649. PMID: 24265529.
Article19. Lee HJ, Shin KH, Kim HH, Yang EJ, Park KH, Kim MJ, et al. Increased prevalence of thalassemia in young people in Korea: impact of increasing immigration. Ann Lab Med. 2019; 39(2):133–140. PMID: 30430775.
Article20. Koo MS, Kim SI, Cho HI, Hattori Y, Yamashiro Y, Hoshitani M, et al. A beta-thalassemia mutation found in Korea. Hemoglobin. 1992; 16(4):313–320. PMID: 1517111.21. Thein SL. The molecular basis of β-thalassemia. Cold Spring Harb Perspect Med. 2013; 3(5):a011700. PMID: 23637309.
Article22. Doro MG, Casu G, Frogheri L, Persico I, Triet LP, Hoa PT, et al. Molecular characterization of β-thalassemia mutations in Central Vietnam. Hemoglobin. 2017; 41(2):96–99. PMID: 28671035.
Article23. Bui Thi Kim L, Phu Chi D, Hoang Thanh C. Spectrum of common α-globin deletion mutations in the southern region of Vietnam. Hemoglobin. 2016; 40(3):206–207. PMID: 27117571.
Article24. Koralkova P, van Solinge WW, van Wijk R. Rare hereditary red blood cell enzymopathies associated with hemolytic anemia - pathophysiology, clinical aspects, and laboratory diagnosis. Int J Lab Hematol. 2014; 36(3):388–397. PMID: 24750686.
Article25. Gallagher PG, Glader B. Diagnosis of pyruvate kinase deficiency. Pediatr Blood Cancer. 2016; 63(5):771–772. PMID: 26836632.
Article26. Frank JE. Diagnosis and management of G6PD deficiency. Am Fam Physician. 2005; 72(7):1277–1282. PMID: 16225031.27. von Seidlein L, Auburn S, Espino F, Shanks D, Cheng Q, McCarthy J, et al. Review of key knowledge gaps in glucose-6-phosphate dehydrogenase deficiency detection with regard to the safe clinical deployment of 8-aminoquinoline treatment regimens: a workshop report. Malar J. 2013; 12(1):112. PMID: 23537118.
Article28. Lee J, Park J, Choi H, Kim J, Kwon A, Jang W, et al. Genetic profiles of Korean patients with glucose-6-phosphate dehydrogenase deficiency. Ann Lab Med. 2017; 37(2):108–116. PMID: 28028996.
Article29. Grace RF, Zanella A, Neufeld EJ, Morton DH, Eber S, Yaish H, et al. Erythrocyte pyruvate kinase deficiency: 2015 status report. Am J Hematol. 2015; 90(9):825–830. PMID: 26087744.
Article30. Zanella A, Bianchi P. Red cell pyruvate kinase deficiency: from genetics to clinical manifestations. Best Pract Res Clin Haematol. 2000; 13(1):57–81.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A new paradigm in the diagnosis of hereditary hemolytic anemia
- A Case of Hereditary Spherocytosis with Hemolytic Anemia due to Mycoplasma pneumonia
- Erythrocyte Band 7 Integral Protein Defect in Congenital Hemolytic Anemia: Hereditary Stomatocytosis
- Treatment and Management of Late Complications in Hereditary Hemolytic Anemia
- Hemolytic anemia in pediatrics