Clinical Characteristics of COVID-19: Clinical Dynamics of Mild Severe Acute Respiratory Syndrome Coronavirus 2 Infection Detected by Early Active Surveillance
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea
- 2Department of Internal Medicine, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea
- 3Department of Internal Medicine, Gyeonggi Provincial Medical Center Paju Hospital, Paju, Korea
- 4Department of Internal Medicine, Jeonbuk National University Medical School, Jeonju, Korea
- 5Department of Internal Medicine, Gyeonggi Provincial Medical Center Suwon Hospital, Suwon, Korea
- 6Department of Internal Medicine, Kangwon National University School of Medicine, Chuncheon, Korea
- 7Department of Internal Medicine, Chung-Ang University Hospital, Seoul, Korea
- 8Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea
- 9Department of Internal Medicine, Gangwon-do Wonju Medical Center, Wonju, Korea
- 10Department of Internal Medicine, Kyung Hee University Hospital, Seoul, Korea
- 11Department of Internal Medicine, Inje University Busan Paik Hospital, Busan, Korea
- 12Department of Internal Medicine, Inje University Sanggye Paik Hospital, Seoul, Korea
- KMID: 2505585
- DOI: http://doi.org/10.3346/jkms.2020.35.e297
Abstract
- Background
There is limited information describing the presenting characteristics and dynamic clinical changes in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection diagnosed in the early phase of illness. This study is a case series of patients with coronavirus disease 2019 (COVID-19) admitted to 11 hospitals in Korea.
Methods
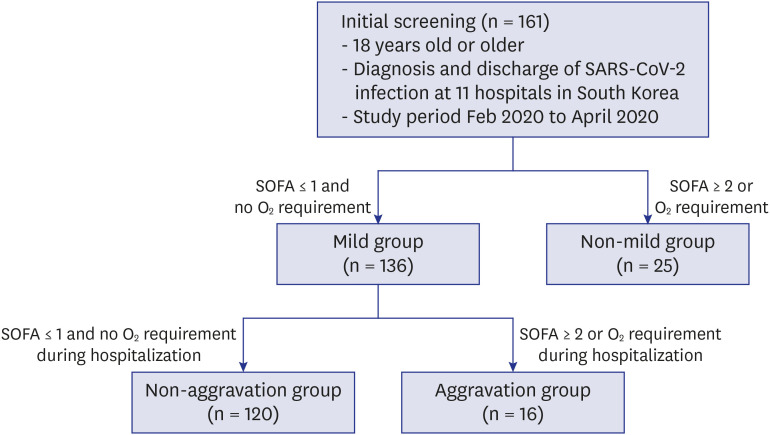
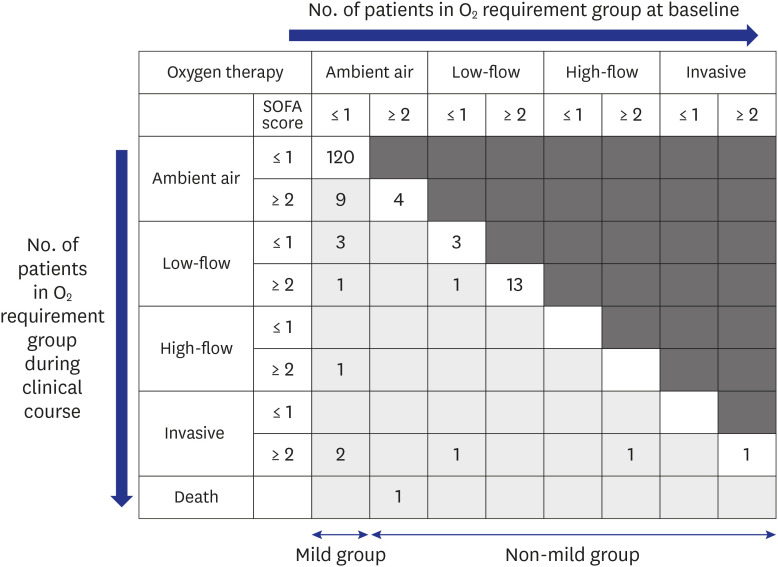
Patients with confirmed SARS-CoV-2 infection by positive polymerase chain reaction (PCR) testing of respiratory specimens by active surveillance that were finally discharged between February 20 and April 30, 2020 were included. Patients were classified into mild and non-mild groups on initial admission according to oxygen demand and Sequential Organ Failure Assessment score, and the mild group was followed up and subgrouped into non-aggravation and aggravation groups.
Results
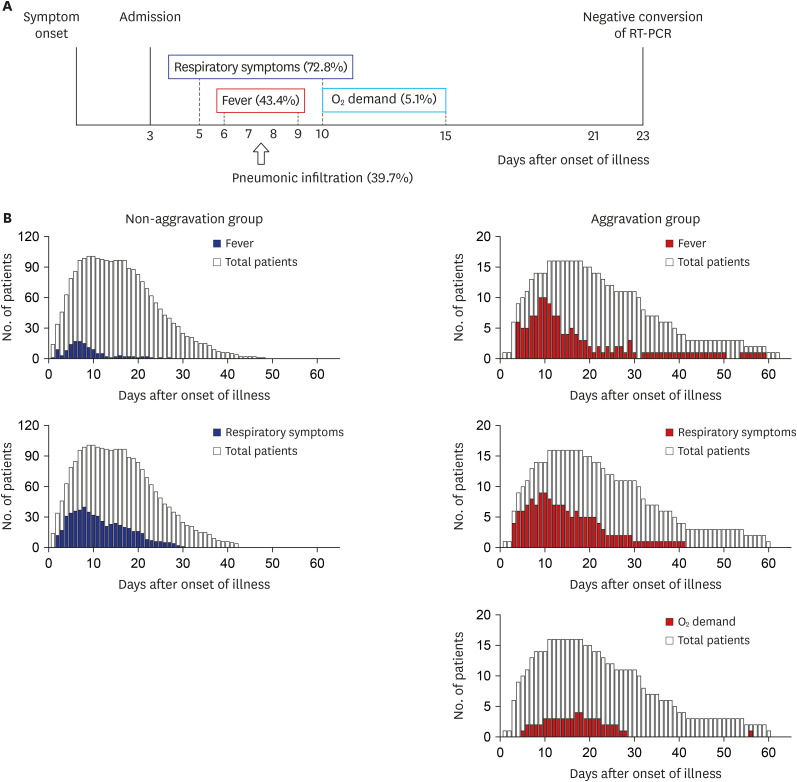
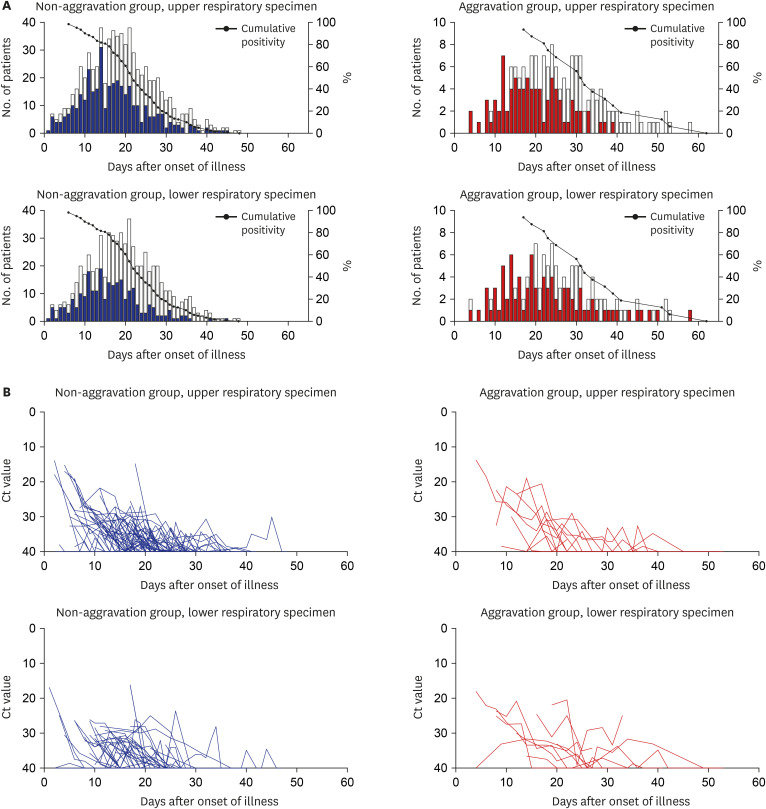
A total of 161 patients with SARS-CoV2 infection were enrolled. Among the mild group of 136 patients, 11.7% of patients experienced clinical aggravation during hospitalization, but there was no initial clinical parameter on admission predicting their aggravation. Fever (odds ratio [OR], 4.56), thrombocytopenia (OR, 12.87), fever (OR, 27.22) and lactate dehydrogenase (LDH) > 300 U/L (OR, 18.35), and CRP > 1 mg/dL (OR, 11.31) significantly indicated aggravation in the 1st, 2nd, 3rd, and 4th 5-day periods, respectively. PCR positivity lasted for a median of 22 days and 32 days after the onset of illness in the nonaggravation and aggravation groups, respectively.
Conclusion
Old age was associated with early severe presentation. Clinical aggravation among asymptomatic or mild patients could not be predicted initially but was heralded by fever and several laboratory markers during the clinical course.
Keyword
Figure
Cited by 4 articles
-
Clinical Characteristics of COVID-19: Risk Factors for Early Oxygen Requirement after Hospitalization
Hyeon Jeong Suh, Eunyoung Lee, Sang-Won Park
J Korean Med Sci. 2021;36(19):e139. doi: 10.3346/jkms.2021.36.e139.Impact of the Coronavirus Disease Pandemic on Patients with Head Injuries in South Korea
Taek Min Nam, Do-Hyung Kim, Ji Hwan Jang, Young Zoon Kim, Kyu Hong Kim, Seung Hwan Kim
J Korean Neurosurg Soc. 2022;65(2):269-275. doi: 10.3340/jkns.2021.0076.Breakthrough COVID-19 Infection During the Delta Variant Dominant Period: Individualized Care Based on Vaccination Status Is Needed
Chan Mi Lee, Eunyoung Lee, Wan Beom Park, Pyoeng Gyun Choe, Kyoung-Ho Song, Eu Suk Kim, Sang-Won Park
J Korean Med Sci. 2022;37(32):e252. doi: 10.3346/jkms.2022.37.e252.Risk Factors for the Prescription of Ineffective Antiviral Candidates for COVID-19 During the Early Pandemic Period in Korea
Eunyoung Lee, Seungyeon Kim, Sun Young Lee, Joo Jeong, Jihwan Bang, Juhwan Oh, Sang Do Shin, Nam Joong Kim, Pyoeng Gyun Choe, Myoung-don Oh
J Korean Med Sci. 2023;38(36):e280. doi: 10.3346/jkms.2023.38.e280.
Reference
-
1. World Health Organization. Coronavirus disease (COVID-2019) situation reports. Updated 2020. Accessed June 5, 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.2. Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 Patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020; 323(16):1574–1581.
Article3. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020; 323(13):1239–1242.4. Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA. 2020; 323(16):1545–1546.5. Choe PG, Kang EK, Lee SY, Oh B, Im D, Lee HY, et al. Selecting coronavirus disease 2019 patients with negligible risk of progression: early experience from non-hospital isolation facility in Korea. Korean J Intern Med. 2020; 35(4):765–770. PMID: 32460457.
Article6. Bedford J, Enria D, Giesecke J, Heymann DL, Ihekweazu C, Kobinger G, et al. COVID-19: towards controlling of a pandemic. Lancet. 2020; 395(10229):1015–1018. PMID: 32197103.
Article7. Kim JY, Choe PG, Oh Y, Oh KJ, Kim J, Park SJ, et al. The first case of 2019 novel coronavirus pneumonia imported into Korea from Wuhan, China: implication for infection prevention and control measures. J Korean Med Sci. 2020; 35(5):e61. PMID: 32030925.
Article8. Peck KR. Early diagnosis and rapid isolation: response to COVID-19 outbreak in Korea. Clin Microbiol Infect. 2020; 26(7):805–807. PMID: 32344168.
Article9. Park SY, Kim YM, Yi S, Lee S, Na BJ, Kim CB, et al. Coronavirus disease outbreak in call center, South Korea. Emerg Infect Dis. 2020; 26(8):1666–1670. PMID: 32324530.
Article10. Korea Centers for Disease Control and Prevention. COVID-19 response guideline version 8-1 (in Korean). Updated 2020. Access June 5, 2020. http://ncov.mohw.go.kr/duBoardList.do?brdId=2&brdGubun=28.11. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020; 395(10223):507–513. PMID: 32007143.
Article12. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020; 323(11):1061–1069.
Article13. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020; 395(10229):1054–1062. PMID: 32171076.
Article14. Gandhi RT, Lynch JB, Del Rio C, del Rio C. Mild or moderate Covid-19. N Engl J Med. Forthcoming. 2020; DOI: 10.1056/NEJMcp2009249.
Article15. Kim GU, Kim MJ, Ra SH, Lee J, Bae S, Jung J, et al. Clinical characteristics of asymptomatic and symptomatic patients with mild COVID-19. Clin Microbiol Infect. 2020; 26(7):948.e1–948.e3. PMID: 32360780.
Article16. Korea Centers for Disease Control and Prevention. COVID-19 response: Living and treatment centers guideline (in Korean). Updated 2020. Access June 5, 2020. http://ncov.mohw.go.kr/duBoardList.do?brdId=2&brdGubun=28.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Severe asthma exacerbation associated with COVID-19 in children: A case report
- Coronavirus Disease 2019: Reasons for Better Clinical Course for Children Compared to Adults
- COVID-19 Mimicking Acute Colitis
- Clinical and Epidemiological Characteristics of Coronavirus Disease 2019 in the Early Stage of Outbreak
- Epidemiology, Virology, and Clinical Features of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2; Coronavirus Disease-19)