Ann Rehabil Med.
2020 Aug;44(4):273-283. 10.5535/arm.19125.
Ultrasound Imaging of the Trunk Muscles in Acute Stroke Patients and Relations With Balance Scales
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Inje University Busan Paik Hospital, Inje University College of Medicine, Busan, Korea
- KMID: 2505387
- DOI: http://doi.org/10.5535/arm.19125
Abstract
Objective
To examine the correlation between ultrasonographic trunk muscle parameters and balance scales in mild acute stroke patients.
Methods
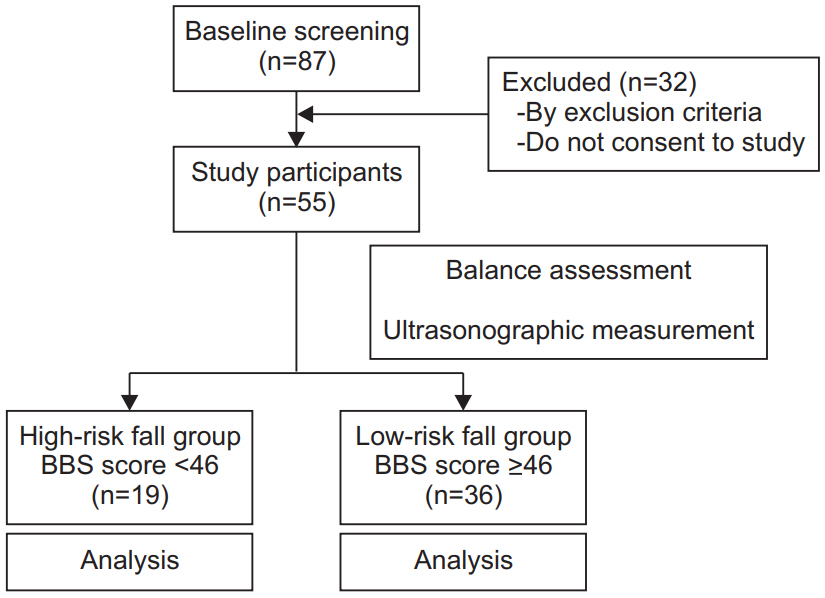
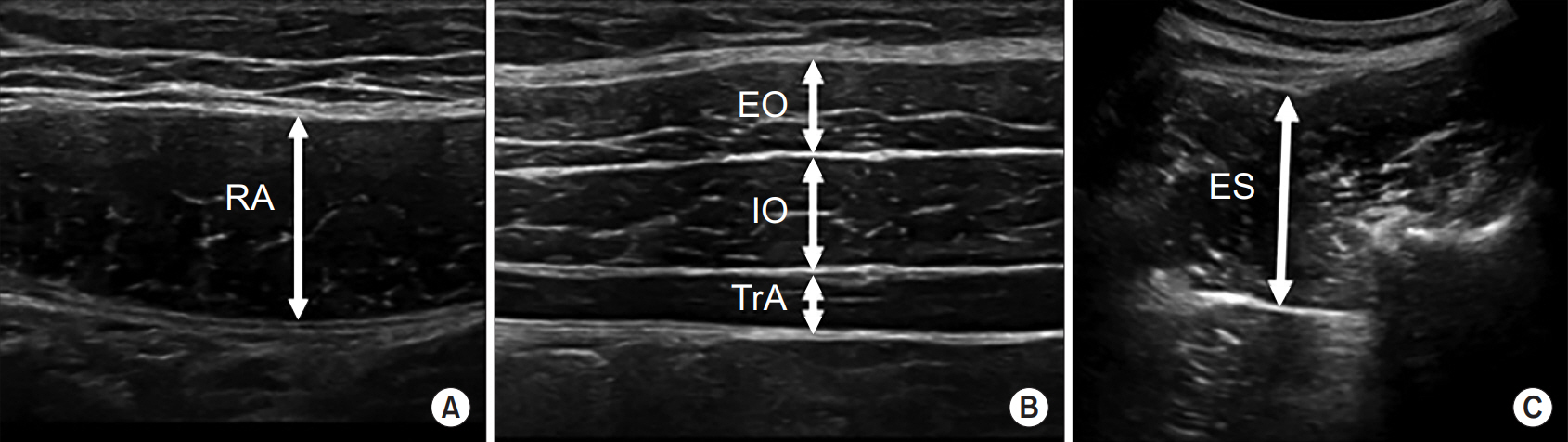
A total of 55 stroke patients with hemiparesis and motor power grade ≥4 in the manual motor test were included. The Scale for the Assessment and Rating of Ataxia (SARA), Berg Balance Scale (BBS), Timed Up and Go Test (TUG), and Trunk Control Test (TCT) were used to evaluate patient balance function. Ultrasonographic parameters were measured on both non-paretic and paretic sides of the rectus abdominis, external oblique, internal oblique, transversus abdominis, and erector spinae muscles. Resting thickness and contraction thickness were measured in all muscles, and contractility and contractility ratio were calculated based on measured thicknesses. The differences between paretic and non-paretic muscle parameters, and the correlation between ultrasonographic parameters and balance scales were analyzed. Stroke patients were divided into two groups according to their fall risk. Ultrasonographic measurements between the two groups were compared.
Results
All muscles’ contraction thickness and contractility were significantly different between paretic and non-paretic sides (p<0.001). Contractility ratios of all trunk muscles showed a significant correlation with SARA, BBS, TUG, and TCT (p<0.05). Contractility ratios of all muscles were significantly different between high- and low-risk fall groups (p<0.05).
Conclusion
The contractility ratio in stroke patients reflects their balance disturbance and fall risk and it may serve as a new parameter for ultrasound imaging of trunk muscles.
Figure
Reference
-
1. Ryerson S, Byl NN, Brown DA, Wong RA, Hidler JM. Altered trunk position sense and its relation to balance functions in people post-stroke. J Neurol Phys Ther. 2008; 32:14–20.
Article2. Yu SH, Park SD. The effects of core stability strength exercise on muscle activity and trunk impairment scale in stroke patients. J Exerc Rehabil. 2013; 9:362–7.
Article3. Karatas M, Cetin N, Bayramoglu M, Dilek A. Trunk muscle strength in relation to balance and functional disability in unihemispheric stroke patients. Am J Phys Med Rehabil. 2004; 83:81–7.
Article4. Juneja G, Czyrny JJ, Linn RT. Admission balance and outcomes of patients admitted for acute inpatient rehabilitation. Am J Phys Med Rehabil. 1998; 77:388–93.5. Sandin KJ, Smith BS. The measure of balance in sitting in stroke rehabilitation prognosis. Stroke. 1990; 21:82–6.
Article6. Bohannon RW, Leary KM. Standing balance and function over the course of acute rehabilitation. Arch Phys Med Rehabil. 1995; 76:994–6.
Article7. Hsieh CL, Sheu CF, Hsueh IP, Wang CH. Trunk control as an early predictor of comprehensive activities of daily living function in stroke patients. Stroke. 2002; 33:2626–30.
Article8. Verheyden G, Vereeck L, Truijen S, Troch M, Herregodts I, Lafosse C, et al. Trunk performance after stroke and the relationship with balance, gait and functional ability. Clin Rehabil. 2006; 20:451–8.
Article9. Winser SJ, Smith C, Hale LA, Claydon LS, Whitney SL. Balance outcome measures in cerebellar ataxia: a Delphi survey. Disabil Rehabil. 2015; 37:165–70.
Article10. Kim BR, Lim JH, Lee SA, Park S, Koh SE, Lee IS, et al. Usefulness of the scale for the assessment and rating of ataxia (SARA) in ataxic stroke patients. Ann Rehabil Med. 2011; 35:772–80.
Article11. Richardson CA, Jull GA. Muscle control-pain control. What exercises would you prescribe? Man Ther. 1995; 1:2–10.
Article12. Marshall PW, Murphy BA. Core stability exercises on and off a Swiss ball. Arch Phys Med Rehabil. 2005; 86:242–9.
Article13. McMeeken JM, Beith ID, Newham DJ, Milligan P, Critchley DJ. The relationship between EMG and change in thickness of transversus abdominis. Clin Biomech (Bristol, Avon). 2004; 19:337–42.
Article14. Hodges PW, Pengel LH, Herbert RD, Gandevia SC. Measurement of muscle contraction with ultrasound imaging. Muscle Nerve. 2003; 27:682–92.
Article15. Ferreira PH, Ferreira ML, Hodges PW. Changes in recruitment of the abdominal muscles in people with low back pain: ultrasound measurement of muscle activity. Spine (Phila Pa 1976). 2004; 29:2560–6.16. Ferreira PH, Ferreira ML, Nascimento DP, Pinto RZ, Franco MR, Hodges PW. Discriminative and reliability analyses of ultrasound measurement of abdominal muscles recruitment. Man Ther. 2011; 16:463–9.
Article17. Kiesel KB, Uhl TL, Underwood FB, Rodd DW, Nitz AJ. Measurement of lumbar multifidus muscle contraction with rehabilitative ultrasound imaging. Man Ther. 2007; 12:161–6.
Article18. Peurala SH, Karttunen AH, Sjogren T, Paltamaa J, Heinonen A. Evidence for the effectiveness of walking training on walking and self-care after stroke: a systematic review and meta-analysis of randomized controlled trials. J Rehabil Med. 2014; 46:387–99.
Article19. Hatem SM, Saussez G, Della Faille M, Prist V, Zhang X, Dispa D, et al. Rehabilitation of motor function after stroke: a multiple systematic review focused on techniques to stimulate upper extremity recovery. Front Hum Neurosci. 2016; 10:442.
Article20. Bogle Thorbahn LD, Newton RA. Use of the Berg Balance Test to predict falls in elderly persons. Phys Ther. 1996; 76:576–83.
Article21. Kim HD, Jeon DM, Bae HW, Kim JG, Han N, Eom MJ. Changes in activation of abdominal muscles at selected angles during trunk exercise by using ultrasonography. Ann Rehabil Med. 2015; 39:950–6.
Article22. Teyhen DS, Gill NW, Whittaker JL, Henry SM, Hides JA, Hodges P. Rehabilitative ultrasound imaging of the abdominal muscles. J Orthop Sports Phys Ther. 2007; 37:450–66.
Article23. Watanabe K, Miyamoto K, Masuda T, Shimizu K. Use of ultrasonography to evaluate thickness of the erector spinae muscle in maximum flexion and extension of the lumbar spine. Spine (Phila Pa 1976). 2004; 29:1472–7.
Article24. Kim HD, You JM, Han N, Eom MJ, Kim JG. Ultrasonographic measurement of transverse abdominis in stroke patients. Ann Rehabil Med. 2014; 38:317–26.
Article25. Stokes M, Hides J, Elliott J, Kiesel K, Hodges P. Rehabilitative ultrasound imaging of the posterior paraspinal muscles. J Orthop Sports Phys Ther. 2007; 37:581–95.
Article26. Horak FB. Clinical measurement of postural control in adults. Phys Ther. 1987; 67:1881–5.
Article27. Paulus WM, Straube A, Brandt T. Visual stabilization of posture. Physiological stimulus characteristics and clinical aspects. Brain. 1984; 107(Pt 4):1143–63.28. Granata KP, England SA. Stability of dynamic trunk movement. Spine (Phila Pa 1976). 2006; 31:E271–6.
Article29. Niam S, Cheung W, Sullivan PE, Kent S, Gu X. Balance and physical impairments after stroke. Arch Phys Med Rehabil. 1999; 80:1227–33.
Article30. English C, McLennan H, Thoirs K, Coates A, Bernhardt J. Loss of skeletal muscle mass after stroke: a systematic review. Int J Stroke. 2010; 5:395–402.
Article31. Jorgensen L, Jacobsen BK. Changes in muscle mass, fat mass, and bone mineral content in the legs after stroke: a 1 year prospective study. Bone. 2001; 28:655–9.
Article32. Carin-Levy G, Greig C, Young A, Lewis S, Hannan J, Mead G. Longitudinal changes in muscle strength and mass after acute stroke. Cerebrovasc Dis. 2006; 21:201–7.
Article33. Stetts DM, Freund JE, Allison SC, Carpenter G. A rehabilitative ultrasound imaging investigation of lateral abdominal muscle thickness in healthy aging adults. J Geriatr Phys Ther. 2009; 32:60–6.
Article34. Rankin G, Stokes M, Newham DJ. Abdominal muscle size and symmetry in normal subjects. Muscle Nerve. 2006; 34:320–6.
Article35. Park HJ, Oh DW, Shin WS. The study of asymmetrical contraction of the lateral abdominal muscles in stroke patients using ultrasound imaging. J Korean Soc Phys Med. 2012; 7:319–27.
Article36. Tahan N, Khademi-Kalantari K, Mohseni-Bandpei MA, Mikaili S, Baghban AA, Jaberzadeh S. Measurement of superficial and deep abdominal muscle thickness: an ultrasonography study. J Physiol Anthropol. 2016; 35:17.
Article37. Kasukawa Y, Miyakoshi N, Hongo M, Ishikawa Y, Noguchi H, Kamo K, et al. Relationships between falls, spinal curvature, spinal mobility and back extensor strength in elderly people. J Bone Miner Metab. 2010; 28:82–7.
Article38. Belavy DL, Armbrecht G, Felsenberg D. Real-time ultrasound measures of lumbar erector spinae and multifidus: reliability and comparison to magnetic resonance imaging. Physiol Meas. 2015; 36:2285–99.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effects of Clam Exercise on the Trunk Control and Balance of Stroke Patients
- The Additive Effects of Core Muscle Strengthening and Trunk NMES on Trunk Balance in Stroke Patients
- Trunk Impairment Scale for Evaluation of Functional Improvement in Acute Stroke Patients
- The Effects of Isokinetic Strengthening of Trunk Muscles on Balance in Hemiplegic Patients
- The Effect of Neuromuscular Electrical Stimulation on Trunk Control in Hemiparetic Stroke Patients