Ann Hepatobiliary Pancreat Surg.
2020 Aug;24(3):269-276. 10.14701/ahbps.2020.24.3.269.
Clinical outcomes of pancreaticoduodenectomy for pancreatic ductal adenocarcinoma depending on preservation or resection of pylorus
- Affiliations
-
- 1Division of Hepatobiliary-Pancreatic Surgery, Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2505339
- DOI: http://doi.org/10.14701/ahbps.2020.24.3.269
Abstract
- Backgrounds/Aims
The comparative effectiveness of pylorus-resecting pancreaticoduodenectomy (PRPD) and pylorus-preserving pancreaticoduodenectomy (PPPD) in pancreatic head cancer is still disputed. The aim of this study was to analyze the data obtained from a large, single center with PPPD compared with PRPD in terms of postoperative outcomes, including blood glucose levels and survival in patients with pancreatic head cancer.
Methods
Between January 2007 and December 2016, a total of 556 patients with pancreatic head cancer underwent either PPPD or PRPD. We analyzed the clinicopathologic data to assess short- and long-term outcomes retrospectively.
Results
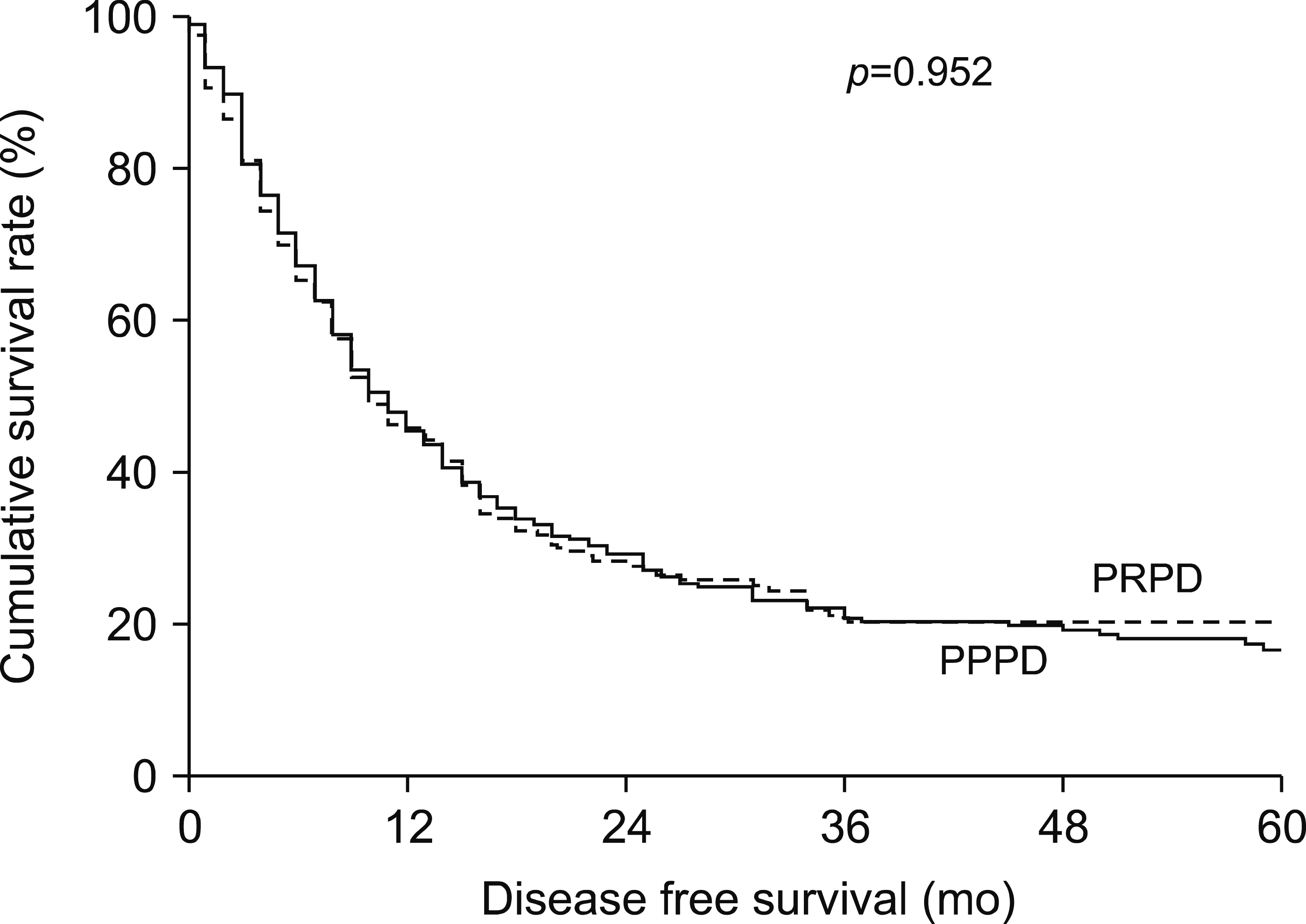
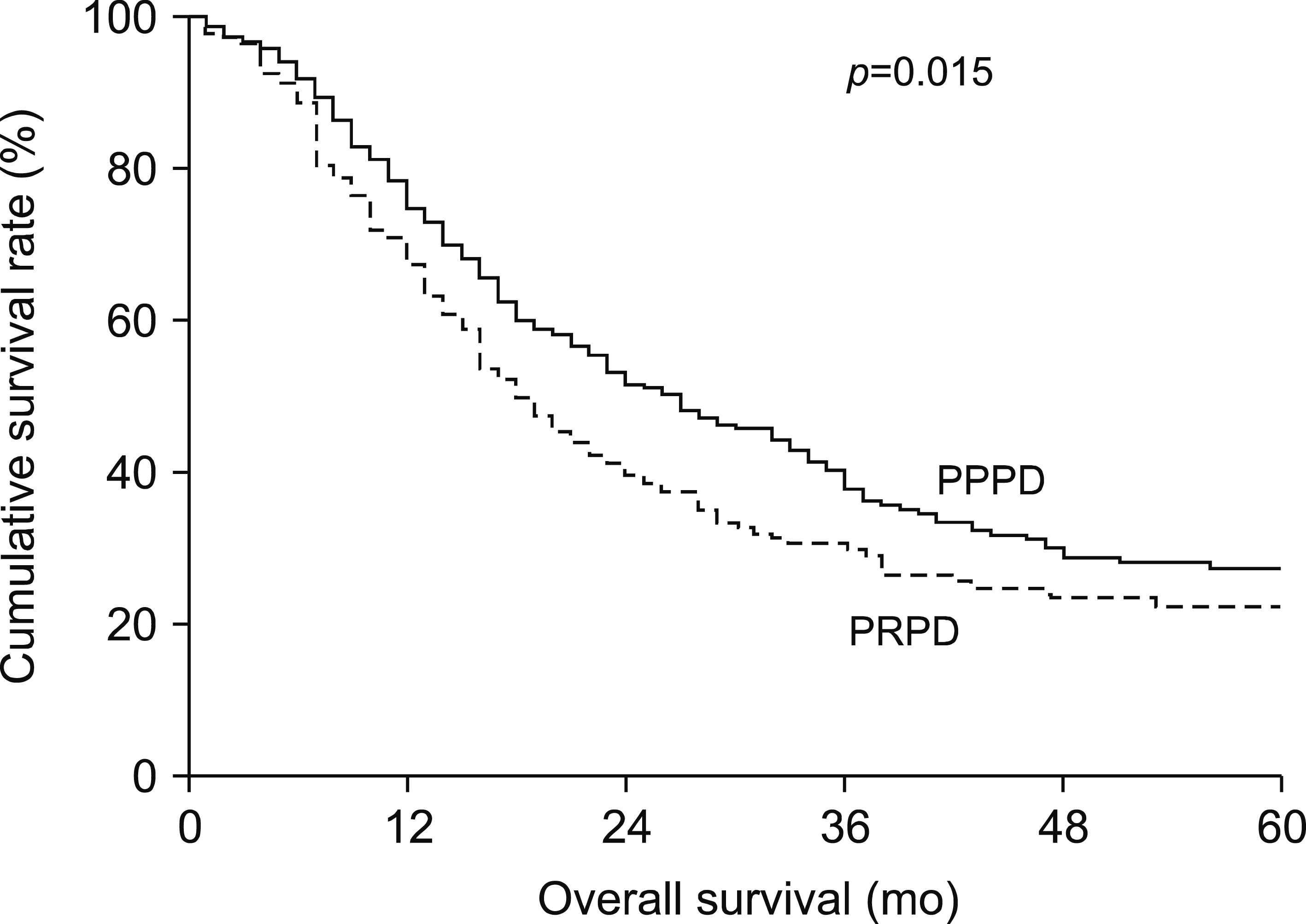
For underlying disease, patients with DM in PPPD were fewer than in PRPD (33.0% vs. 46.2%, p=0.002). The median value of CA19-9 was significantly higher in PRPD than in PPPD (129.36 vs. 86.47, p=0.037). The incidence of Clavien-Dindo grade III to V major complications in PPPD was significantly higher than in PRPD (20.4% vs. 13.4%, p=0.032). Resection of pylorus was shown to reduce complications in univariate and multivariate analyses (p=0.032 and = 0.021, respectively). The 5-year survival rates were 27.6% in the PPPD group and 22.4% in the PRPD group (p=0.015).
Conclusions
The results of PPPD and PRPD showed no significant differences from those reported conventionally in previous studies. Although further well-designed studies are needed, it is more important to select the range of surgical resection for the patient’s disease regardless of resection of pylorus.
Keyword
Figure
Reference
-
1. Iqbal N, Lovegrove RE, Tilney HS, Abraham AT, Bhattacharya S, Tekkis PP, et al. 2008; A comparison of pancreaticoduodenectomy with pylorus preserving pancreaticoduodenectomy: a meta-analysis of 2822 patients. Eur J Surg Oncol. 34:1237–1245. DOI: 10.1016/j.ejso.2007.12.004. PMID: 18242943.
Article2. Yang C, Wu HS, Chen XL, Wang CY, Gou SM, Xiao J, et al. 2014; Pylorus-preserving versus pylorus-resecting pancreaticoduodenectomy for periampullary and pancreatic carcinoma: a meta-analysis. PLoS One. 9:e90316. DOI: 10.1371/journal.pone.0090316. PMID: 24603478. PMCID: PMC3946060.
Article3. Watson K. 1944; Carcinoma of the ampulla of vater successful radical resection. Br J Surg. 31:368–373. DOI: 10.1002/bjs.18003112406.4. Doyle DJ, Garmon EH. 2020. American Society of Anesthesiologists Classification (ASA Class). StatPearls. StatPearls Publishing LLC;Treasure Island (FL):5. Verbeke CS, Leitch D, Menon KV, McMahon MJ, Guillou PJ, Anthoney A. 2006; Redefining the R1 resection in pancreatic cancer. Br J Surg. 93:1232–1237. DOI: 10.1002/bjs.5397. PMID: 16804874.
Article6. Esposito I, Kleeff J, Bergmann F, Reiser C, Herpel E, Friess H, et al. 2008; Most pancreatic cancer resections are R1 resections. Ann Surg Oncol. 15:1651–1660. DOI: 10.1245/s10434-008-9839-8. PMID: 18351300.
Article7. You Y, Choi DW, Heo JS, Han IW, Choi SH, Jang KT, et al. 2019; Clinical significance of revised microscopic positive resection margin status in ductal adenocarcinoma of pancreatic head. Ann Surg Treat Res. 96:19–26. DOI: 10.4174/astr.2019.96.1.19. PMID: 30603630. PMCID: PMC6306502.
Article8. Cong L, Liu Q, Zhang R, Cui M, Zhang X, Gao X, et al. 2018; Tumor size classification of the 8th edition of TNM staging system is superior to that of the 7th edition in predicting the survival outcome of pancreatic cancer patients after radical resection and adjuvant chemotherapy. Sci Rep. 8:10383. DOI: 10.1038/s41598-018-28193-4. PMID: 29991730. PMCID: PMC6039534.
Article9. Dindo D, Demartines N, Clavien PA. 2004; Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 240:205–213. DOI: 10.1097/01.sla.0000133083.54934.ae. PMID: 15273542. PMCID: PMC1360123.10. Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. 2017; The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 161:584–591. DOI: 10.1016/j.surg.2016.11.014. PMID: 28040257.11. Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, et al. 2007; Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 142:761–768. DOI: 10.1016/j.surg.2007.05.005. PMID: 17981197.
Article12. Chen QJ, He ZQ, Yang Y, Zhang YS, Chen XL, Yang HJ, et al. 2015; Is there comparable morbidity in pylorus-preserving and pylorus- resecting pancreaticoduodenectomy? A meta-analysis. J Huazhong Univ Sci Technolog Med Sci. 35:793–800. DOI: 10.1007/s11596-015-1509-z. PMID: 26670427.13. Lin PW, Lin YJ. 1999; Prospective randomized comparison between pylorus-preserving and standard pancreaticoduodenectomy. Br J Surg. 86:603–607. DOI: 10.1046/j.1365-2168.1999.01074.x. PMID: 10361177.
Article14. Seiler CA, Wagner M, Sadowski C, Kulli C, Büchler MW. 2000; Randomized prospective trial of pylorus-preserving vs. classic duodenopancreatectomy (Whipple procedure): initial clinical results. J Gastrointest Surg. 4:443–452. DOI: 10.1016/S1091-255X(00)80084-0. PMID: 11077317.
Article15. Tran KT, Smeenk HG, van Eijck CH, Kazemier G, Hop WC, Greve JW, et al. 2004; Pylorus preserving pancreaticoduodenectomy versus standard Whipple procedure: a prospective, randomized, multicenter analysis of 170 patients with pancreatic and periampullary tumors. Ann Surg. 240:738–745. DOI: 10.1097/01.sla.0000143248.71964.29. PMID: 15492552. PMCID: PMC1356476.16. Seiler CA, Wagner M, Bachmann T, Redaelli CA, Schmied B, Uhl W, et al. 2005; Randomized clinical trial of pylorus-preserving duodenopancreatectomy versus classical Whipple resection-long term results. Br J Surg. 92:547–556. DOI: 10.1002/bjs.4881. PMID: 15800958.
Article17. Lin PW, Shan YS, Lin YJ, Hung CJ. 2005; Pancreaticoduodenectomy for pancreatic head cancer: PPPD versus Whipple procedure. Hepatogastroenterology. 52:1601–1604. PMID: 16201125.18. Diener MK, Knaebel HP, Heukaufer C, Antes G, Büchler MW, Seiler CM. 2007; A systematic review and meta-analysis of pylorus-preserving versus classical pancreaticoduodenectomy for surgical treatment of periampullary and pancreatic carcinoma. Ann Surg. 245:187–200. DOI: 10.1097/01.sla.0000242711.74502.a9. PMID: 17245171. PMCID: PMC1876989.
Article19. Eeson G, Chang N, McGahan CE, Khurshed F, Buczkowski AK, Scudamore CH, et al. 2012; Determination of factors predictive of outcome for patients undergoing a pancreaticoduodenectomy of pancreatic head ductal adenocarcinomas. HPB (Oxford). 14:310–316. DOI: 10.1111/j.1477-2574.2012.00448.x. PMID: 22487068. PMCID: PMC3384850.
Article20. Gouma DJ, van Geenen RC, van Gulik TM, de Haan RJ, de Wit LT, Busch OR, et al. 2000; Rates of complications and death after pancreaticoduodenectomy: risk factors and the impact of hospital volume. Ann Surg. 232:786–795. DOI: 10.1097/00000658-200012000-00007. PMID: 11088073. PMCID: PMC1421271.
Article21. El Nakeeb A, Salah T, Sultan A, El Hemaly M, Askr W, Ezzat H, et al. 2013; Pancreatic anastomotic leakage after pancreaticoduodenectomy. Risk factors, clinical predictors, and management (single center experience). World J Surg. 37:1405–1418. DOI: 10.1007/s00268-013-1998-5. PMID: 23494109.
Article22. Klaiber U, Probst P, Hüttner FJ, Bruckner T, Strobel O, Diener MK, et al. 2020; Randomized trial of pylorus-preserving vs. pylorus-resecting pancreatoduodenectomy: long-term morbidity and quality of life. J Gastrointest Surg. 24:341–352. DOI: 10.1007/s11605-018-04102-y. PMID: 30671796.
Article23. Khadka R, Tian W, Hao X, Koirala R. 2018; Risk factor, early diagnosis and overall survival on outcome of association between pancreatic cancer and diabetes mellitus: changes and advances, a review. Int J Surg. 52:342–346. DOI: 10.1016/j.ijsu.2018.02.058. PMID: 29535016.
Article24. Kwon JH, Kim SC, Shim IK, Song KB, Lee JH, Hwang DW, et al. 2015; Factors affecting the development of diabetes mellitus after pancreatic resection. Pancreas. 44:1296–1303. DOI: 10.1097/MPA.0000000000000404. PMID: 26390413.
Article25. White MA, Agle SC, Fuhr HM, Mehaffey JH, Waibel BH, Zervos EE. 2011; Impact of pancreatic cancer and subsequent resection on glycemic control in diabetic and nondiabetic patients. Am Surg. 77:1032–1037. DOI: 10.1177/000313481107700823. PMID: 21944519.
Article26. Wang F, Gupta S, Holly EA. 2006; Diabetes mellitus and pancreatic cancer in a population-based case-control study in the San Francisco Bay Area, California. Cancer Epidemiol Biomarkers Prev. 15:1458–1463. DOI: 10.1158/1055-9965.EPI-06-0188. PMID: 16896032.
Article27. Fogar P, Pasquali C, Basso D, Sperti C, Panozzo MP, Tessari G, et al. 1994; Diabetes mellitus in pancreatic cancer follow-up. Anticancer Res. 14:2827–2830. PMID: 7532931.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prognostic Factors and Survival Rate of Pancreatic Adenocarcinoma after Curative Surgery
- Pancreaticoduodenectomy of Pancreatic Ductal Adenocarcinoma in the Elderly
- A Result of Surgical Treatment for Ductal Adenocarcinoma of the Head of the Pancreas
- Surgical Extent and Types in Pancreatic Cancer
- Squamous Cell Carcinoma of the Pancreas with Invasion of Duodenum and Pylorus