Korean Circ J.
2020 Aug;50(8):645-657. 10.4070/kcj.2020.0098.
Ethnic Differences in Oral Antithrombotic Therapy
- Affiliations
-
- 1Department of Internal Medicine, Cardiovascular Center, Seoul National University Hospital, Seoul, Korea
- KMID: 2505119
- DOI: http://doi.org/10.4070/kcj.2020.0098
Abstract
- Oral antithrombotic therapy (antiplatelet therapy and anticoagulation therapy) is a key element of pharmacotherapy in patients with cardiovascular (CV) disease. Several reports of ethnic differences have suggested that there may be difference therapeutic requirements and response to therapy for antithrombotic therapy. In particular for East Asians, there seems to be a lower incidence of ischemic outcomes and a higher incidence of bleeding outcomes compared to Westerners. The purpose of this review is to describe the ethnicity-related differences in antithrombotic therapy for CV disease and to discuss the need to establish a more effective and targeted antithrombotic treatment strategy in East Asians.
Figure
Cited by 1 articles
-
Percutaneous Patent Foramen Ovale Closure After Stroke
Oh-Hyun Lee, Jung-Sun Kim
Korean Circ J. 2022;52(11):801-807. doi: 10.4070/kcj.2022.0258.
Reference
-
1. Chaturvedi N. Ethnic differences in cardiovascular disease. Heart. 2003; 89:681–686. PMID: 12748237.
Article2. Gasevic D, Ross ES, Lear SA. Ethnic differences in cardiovascular disease risk factors: a systematic review of North American evidence. Can J Cardiol. 2015; 31:1169–1179. PMID: 26239006.
Article3. Henderson SO, Coetzee GA, Ross RK, Yu MC, Henderson BE. Elevated mortality rates from circulatory disease in African American men and women of Los Angeles County, California--a possible genetic susceptibility? Am J Med Sci. 2000; 320:18–23. PMID: 10910369.
Article4. Kimura K, Kimura T, Ishihara M, et al. JCS 2018 guideline on diagnosis and treatment of acute coronary syndrome. Circ J. 2019; 83:1085–1196. PMID: 30930428.5. Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 2016; 68:1082–1115. PMID: 27036918.6. Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018; 39:119–177. PMID: 28886621.7. Bhatt DL, Steg PG, Ohman EM, et al. International prevalence, recognition, and treatment of cardiovascular risk factors in outpatients with atherothrombosis. JAMA. 2006; 295:180–189. PMID: 16403930.
Article8. Steg PG, Bhatt DL, Wilson PW, et al. One-year cardiovascular event rates in outpatients with atherothrombosis. JAMA. 2007; 297:1197–1206. PMID: 17374814.
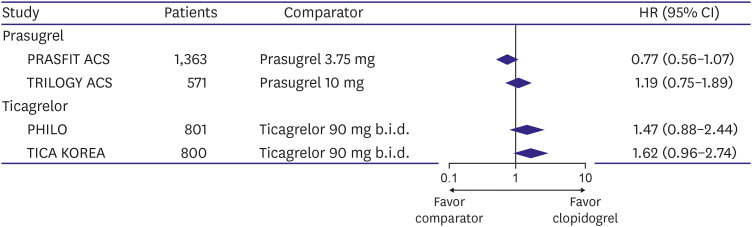
Article9. Kang J, Park KW, Palmerini T, et al. Racial differences in ischaemia/bleeding risk trade-off during anti-platelet therapy: individual patient level landmark meta-analysis from seven RCTs. Thromb Haemost. 2019; 119:149–162. PMID: 30597509.
Article10. Daemen J, Wenaweser P, Tsuchida K, et al. Early and late coronary stent thrombosis of sirolimus-eluting and paclitaxel-eluting stents in routine clinical practice: data from a large two-institutional cohort study. Lancet. 2007; 369:667–678. PMID: 17321312.
Article11. Kimura T, Morimoto T, Nakagawa Y, et al. Antiplatelet therapy and stent thrombosis after sirolimus-eluting stent implantation. Circulation. 2009; 119:987–995. PMID: 19204304.
Article12. Park DW, Yun SC, Lee SW, et al. Stent thrombosis, clinical events, and influence of prolonged clopidogrel use after placement of drug-eluting stent data from an observational cohort study of drug-eluting versus bare-metal stents. JACC Cardiovasc Interv. 2008; 1:494–503. PMID: 19463351.13. Price MJ, Nayak KR, Barker CM, Kandzari DE, Teirstein PS. Predictors of heightened platelet reactivity despite dual-antiplatelet therapy in patients undergoing percutaneous coronary intervention. Am J Cardiol. 2009; 103:1339–1343. PMID: 19427425.
Article14. Park KW, Park JJ, Jeon KH, et al. Clinical predictors of high posttreatment platelet reactivity to clopidogrel in Koreans. Cardiovasc Ther. 2012; 30:5–11. PMID: 21129165.
Article15. Shen AY, Yao JF, Brar SS, Jorgensen MB, Chen W. Racial/ethnic differences in the risk of intracranial hemorrhage among patients with atrial fibrillation. J Am Coll Cardiol. 2007; 50:309–315. PMID: 17659197.
Article16. Ma C. Current antithrombotic treatment in East Asia: some perspectives on anticoagulation and antiplatelet therapy. Thromb Haemost. 2012; 107:1014–1018. PMID: 22535432.
Article17. White RH, Keenan CR. Effects of race and ethnicity on the incidence of venous thromboembolism. Thromb Res. 2009; 123(Suppl 4):S11–7. PMID: 19303496.
Article18. Zakai NA, McClure LA. Racial differences in venous thromboembolism. J Thromb Haemost. 2011; 9:1877–1882. PMID: 21797965.
Article19. Collins SD, Torguson R, Gaglia MA Jr, et al. Does black ethnicity influence the development of stent thrombosis in the drug-eluting stent era? Circulation. 2010; 122:1085–1090. PMID: 20805432.
Article20. Mak KH, Bhatt DL, Shao M, et al. Ethnic variation in adverse cardiovascular outcomes and bleeding complications in the Clopidogrel for High Atherothrombotic Risk and Ischemic Stabilization, Management, and Avoidance (CHARISMA) study. Am Heart J. 2009; 157:658–665. PMID: 19332192.
Article21. Kitamura A, Nakagawa Y, Sato M, et al. Proportions of stroke subtypes among men and women > or =40 years of age in an urban Japanese city in 1992, 1997, and 2002. Stroke. 2006; 37:1374–1378. PMID: 16690900.22. Kwon TJ, Tantry US, Park Y, et al. Influence of platelet reactivity on BARC classification in East Asian patients undergoing percutaneous coronary intervention. Results of the ACCEL-BLEED study. Thromb Haemost. 2016; 115:979–992. PMID: 26790469.23. Guirguis-Blake JM, Evans CV, Senger CA, Rowland MG, O'Connor EA, Whitlock EP. Aspirin for the primary prevention of cardiovascular events: a systematic evidence review for the U.S. preventive services task force. Rockville (MD): Agency for Healthcare Research and Quality;2015.24. Lei H, Gao Q, Liu SR, Xu J. The benefit and safety of aspirin for primary prevention of ischemic stroke: a meta-analysis of randomized trials. Front Pharmacol. 2016; 7:440. PMID: 27917124.
Article25. Huang WY, Saver JL, Wu YL, Lin CJ, Lee M, Ovbiagele B. Frequency of intracranial hemorrhage with low-dose aspirin in individuals without symptomatic cardiovascular disease: a systematic review and meta-analysis. JAMA Neurol. 2019; 76:906–914.26. Patrono C, Coller B, Dalen JE, et al. Platelet-active drugs : the relationships among dose, effectiveness, and side effects. Chest. 2001; 119:39S–63S. PMID: 11157642.27. Koskinas KC, Räber L, Zanchin T, et al. Clinical impact of gastrointestinal bleeding in patients undergoing percutaneous coronary interventions. Circ Cardiovasc Interv. 2015; 8:e002053. PMID: 25910501.
Article28. Leong RW. Differences in peptic ulcer between the East and the West. Gastroenterol Clin North Am. 2009; 38:363–379. PMID: 19446264.
Article29. Derry S, Loke YK. Risk of gastrointestinal haemorrhage with long term use of aspirin: meta-analysis. BMJ. 2000; 321:1183–1187. PMID: 11073508.
Article30. Goto S, Ikeda Y, Chan JC, et al. Risk-factor profile, drug usage and cardiovascular events within a year in patients with and at high risk of atherothrombosis recruited from Asia as compared with those recruited from non-Asian regions: a substudy of the REduction of Atherothrombosis for Continued Health (REACH) registry. Heart Asia. 2011; 3:93–98. PMID: 27326003.31. Levine GN, Jeong YH, Goto S, et al. Expert consensus document: World Heart Federation expert consensus statement on antiplatelet therapy in East Asian patients with ACS or undergoing PCI. Nat Rev Cardiol. 2014; 11:597–606. PMID: 25154978.32. Jeong YH. “East asian paradox”: challenge for the current antiplatelet strategy of “one-guideline-fits-all races” in acute coronary syndrome. Curr Cardiol Rep. 2014; 16:485. PMID: 24668607.
Article33. Aradi D, Storey RF, Komócsi A, et al. Expert position paper on the role of platelet function testing in patients undergoing percutaneous coronary intervention. Eur Heart J. 2014; 35:209–215. PMID: 24067509.
Article34. Kim IS, Jeong YH, Tantry US, et al. Relation between the vasodilator-stimulated phosphoprotein phosphorylation assay and light transmittance aggregometry in East Asian patients after high-dose clopidogrel loading. Am Heart J. 2013; 166:95–103. PMID: 23816027.
Article35. Huo Y, Jeong YH, Gong Y, et al. 2018 update of expert consensus statement on antiplatelet therapy in East Asian patients with ACS or undergoing PCI. Sci Bull (Beijing). 2019; 64:166–179.
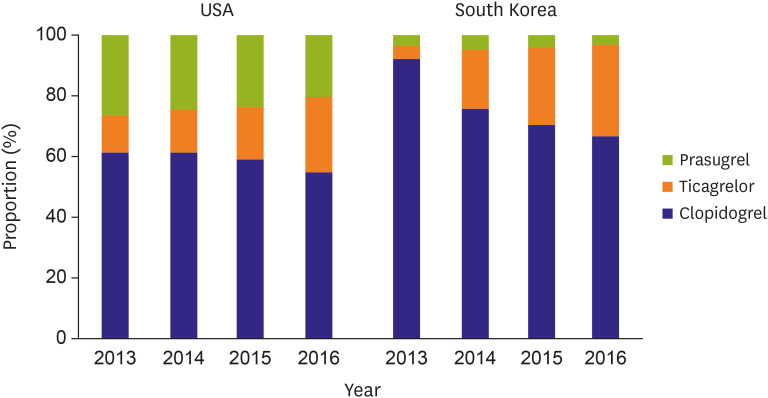
Article36. Dayoub EJ, Seigerman M, Tuteja S, et al. Trends in platelet adenosine diphosphate P2Y12 receptor inhibitor use and adherence among antiplatelet-naive patients after percutaneous coronary intervention, 2008–2016. JAMA Intern Med. 2018; 178:943–950. PMID: 29799992.
Article37. Kim C, Shin DH, Ahn CM, et al. The use pattern and clinical impact of new antiplatelet agents including prasugrel and ticagrelor on 30-day outcomes after acute myocardial infarction in Korea: Korean Health Insurance Review and Assessment Data. Korean Circ J. 2017; 47:888–897. PMID: 29035430.
Article38. Aradi D, Kirtane A, Bonello L, et al. Bleeding and stent thrombosis on P2Y12-inhibitors: collaborative analysis on the role of platelet reactivity for risk stratification after percutaneous coronary intervention. Eur Heart J. 2015; 36:1762–1771. PMID: 25896078.
Article39. Gurbel PA, Jeong YH, Navarese EP, Tantry US. Platelet-mediated thrombosis: from bench to bedside. Circ Res. 2016; 118:1380–1391. PMID: 27126648.40. Tantry US, Bonello L, Aradi D, et al. Consensus and update on the definition of on-treatment platelet reactivity to adenosine diphosphate associated with ischemia and bleeding. J Am Coll Cardiol. 2013; 62:2261–2273. PMID: 24076493.
Article41. Li J, Tang W, Storey RF, Husted S, Teng R. Population pharmacokinetics of ticagrelor in patients with acute coronary syndromes. Int J Clin Pharmacol Ther. 2016; 54:666–674. PMID: 27191766.
Article42. Lee YS, Jin CD, Kim MH, et al. Comparison of prasugrel and ticagrelor antiplatelet effects in korean patients presenting with ST-segment elevation myocardial infarction. Circ J. 2015; 79:1248–1254. PMID: 25959558.
Article43. Wallentin L, Becker RC, Budaj A, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009; 361:1045–1057. PMID: 19717846.44. Kang HJ, Clare RM, Gao R, et al. Ticagrelor versus clopidogrel in Asian patients with acute coronary syndrome: a retrospective analysis from the Platelet Inhibition and Patient Outcomes (PLATO) trial. Am Heart J. 2015; 169:899–905.e1. PMID: 26027629.
Article45. Park DW, Kwon O, Jang JS, et al. Clinically significant bleeding with ticagrelor versus clopidogrel in Korean patients with acute coronary syndromes intended for invasive management: a randomized clinical trial. Circulation. 2019; 140:1865–1877. PMID: 31553203.46. Yokoi H, Kimura T, Isshiki T, Ogawa H, Ikeda Y. Pharmacodynamic assessment of a novel P2Y12 receptor antagonist in Japanese patients with coronary artery disease undergoing elective percutaneous coronary intervention. Thromb Res. 2012; 129:623–628. PMID: 22178576.
Article47. Saito S, Isshiki T, Kimura T, et al. Efficacy and safety of adjusted-dose prasugrel compared with clopidogrel in Japanese patients with acute coronary syndrome: the PRASFIT-ACS study. Circ J. 2014; 78:1684–1692. PMID: 24759796.48. Roe MT, Armstrong PW, Fox KA, et al. Prasugrel versus clopidogrel for acute coronary syndromes without revascularization. N Engl J Med. 2012; 367:1297–1309. PMID: 22920930.49. The Korean Society of Cardiology. Guidelines of Antiplatelet Therapy for Patients with Acute Coronary Syndrome [Internet]. Seoul: The Korean Society of Cardiology;2012. cited 2020 Apr 7. Available from https://kaim.or.kr/files/guide/%EC%8B%AC%EC%9E%A5_04.pdf.50. Risk factors for stroke and efficacy of antithrombotic therapy in atrial fibrillation. Analysis of pooled data from five randomized controlled trials. Arch Intern Med. 1994; 154:1449–1457. PMID: 8018000.51. Connolly SJ, Pogue J, Eikelboom J, et al. Benefit of oral anticoagulant over antiplatelet therapy in atrial fibrillation depends on the quality of international normalized ratio control achieved by centers and countries as measured by time in therapeutic range. Circulation. 2008; 118:2029–2037. PMID: 18955670.
Article52. Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007; 146:857–867. PMID: 17577005.
Article53. January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the heart rhythm society in collaboration with the society of thoracic surgeons. Circulation. 2019; 140:e125–51. PMID: 30686041.
Article54. Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016; 37:2893–2962. PMID: 27567408.
Article55. El Rouby S, Mestres CA, LaDuca FM, Zucker ML. Racial and ethnic differences in warfarin response. J Heart Valve Dis. 2004; 13:15–21. PMID: 14765833.56. Oh S, Goto S, Accetta G, et al. Vitamin K antagonist control in patients with atrial fibrillation in Asia compared with other regions of the world: real-world data from the GARFIELD-AF registry. Int J Cardiol. 2016; 223:543–547. PMID: 27552578.
Article57. Oldgren J, Healey JS, Ezekowitz M, et al. Variations in cause and management of atrial fibrillation in a prospective registry of 15,400 emergency department patients in 46 countries: the RE-LY atrial fibrillation registry. Circulation. 2014; 129:1568–1576. PMID: 24463370.58. JCS Joint Working Group. Guidelines for pharmacotherapy of atrial fibrillation (JCS 2008): digest version. Circ J. 2010; 74:2479–2500. PMID: 20962419.59. Yamaguchi T. Optimal intensity of warfarin therapy for secondary prevention of stroke in patients with nonvalvular atrial fibrillation : a multicenter, prospective, randomized trial. Japanese Nonvalvular Atrial Fibrillation-Embolism Secondary Prevention Cooperative Study Group. Stroke. 2000; 31:817–821. PMID: 10753981.60. Inoue H, Okumura K, Atarashi H, et al. Target international normalized ratio values for preventing thromboembolic and hemorrhagic events in Japanese patients with non-valvular atrial fibrillation: results of the J-RHYTHM registry. Circ J. 2013; 77:2264–2270. PMID: 23708863.61. Chiang CE, Wang KL, Lip GY. Stroke prevention in atrial fibrillation: an Asian perspective. Thromb Haemost. 2014; 111:789–797. PMID: 24500243.
Article62. Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009; 361:1139–1151. PMID: 19717844.
Article63. Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011; 365:883–891. PMID: 21830957.
Article64. Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011; 365:981–992. PMID: 21870978.65. Giugliano RP, Ruff CT, Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013; 369:2093–2104. PMID: 24251359.
Article66. Wang KL, Lip GY, Lin SJ, Chiang CE, Non-Vitamin K. Non-vitamin K antagonist oral anticoagulants for stroke prevention in Asian patients with nonvalvular atrial fibrillation: meta-analysis. Stroke. 2015; 46:2555–2561. PMID: 26304863.67. Chiang CE, Okumura K, Zhang S, et al. 2017 consensus of the Asia Pacific Heart Rhythm Society on stroke prevention in atrial fibrillation. J Arrhythm. 2017; 33:345–367. PMID: 28765771.
Article68. Lee SR, Choi EK, Park CS, et al. Direct oral anticoagulants in patients with nonvalvular atrial fibrillation and low body weight. J Am Coll Cardiol. 2019; 73:919–931. PMID: 30819360.69. Ohman EM, Roe MT, Steg PG, et al. Clinically significant bleeding with low-dose rivaroxaban versus aspirin, in addition to P2Y12 inhibition, in acute coronary syndromes (GEMINI-ACS-1): a double-blind, multicentre, randomised trial. Lancet. 2017; 389:1799–1808. PMID: 28325638.
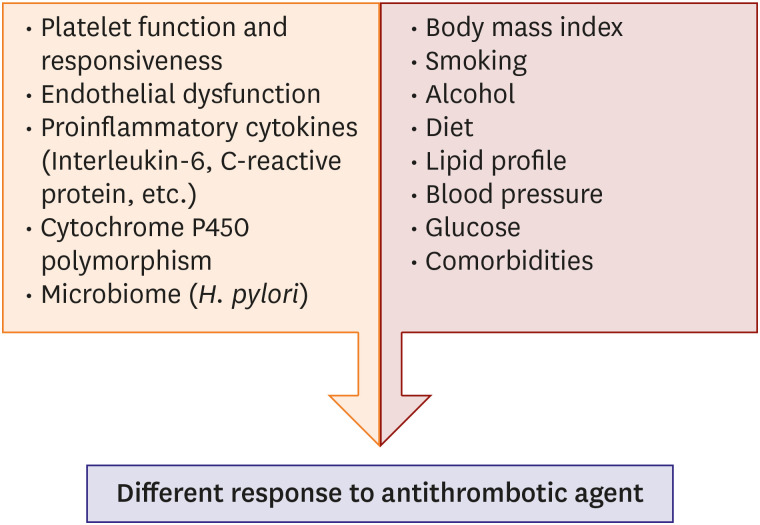
Article70. Iantorno M, Weintraub WS, Garcia-Garcia HM, et al. Genetic and nongenetic implications of racial variation in response to antiplatelet therapy. Am J Cardiol. 2019; 123:1878–1883. PMID: 30967284.
Article71. Bray PF, Mathias RA, Faraday N, et al. Heritability of platelet function in families with premature coronary artery disease. J Thromb Haemost. 2007; 5:1617–1623. PMID: 17663734.
Article72. Folsom AR, Aleksic N, Sanhueza A, Boerwinkle E. Risk factor correlates of platelet and leukocyte markers assessed by flow cytometry in a population-based sample. Atherosclerosis. 2009; 205:272–278. PMID: 19124123.
Article73. Gurbel PA, Bliden KP, Cohen E, et al. Race and sex differences in thrombogenicity: risk of ischemic events following coronary stenting. Blood Coagul Fibrinolysis. 2008; 19:268–275. PMID: 18469547.
Article74. Scott SA, Sangkuhl K, Stein CM, et al. Clinical pharmacogenetics implementation consortium guidelines for CYP2C19 genotype and clopidogrel therapy: 2013 update. Clin Pharmacol Ther. 2013; 94:317–323. PMID: 23698643.
Article75. Jeong YH, Abadilla KA, Tantry US, et al. Influence of CYP2C19*2 and *3 loss-of-function alleles on the pharmacodynamic effects of standard- and high-dose clopidogrel in East Asians undergoing percutaneous coronary intervention: the results of the ACCEL-DOUBLE-2N3 study. J Thromb Haemost. 2013; 11:1194–1197. PMID: 23517020.
Article76. Schick UM, Jain D, Hodonsky CJ, et al. Genome-wide association study of platelet count identifies ancestry-specific loci in Hispanic/Latino Americans. Am J Hum Genet. 2016; 98:229–242. PMID: 26805783.
Article77. Lutsey PL, Cushman M, Steffen LM, et al. Plasma hemostatic factors and endothelial markers in four racial/ethnic groups: the MESA study. J Thromb Haemost. 2006; 4:2629–2635. PMID: 17002663.
Article78. Albert MA. Inflammatory biomarkers, race/ethnicity and cardiovascular disease. Nutr Rev. 2007; 65:S234–8. PMID: 18240555.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antithrombotic Therapy for Patients with Nonvalvular Atrial Fibrillation
- Review of Updated Guidelines and Evidence for Antithrombotic Therapy in Acute Ischemic Stroke
- Periprocedural antithrombotic management
- Antithrombotic therapy has no beneficial effect in conservative treatment of spontaneous isolated superior mesenteric arterial dissection
- Outcomes of Endoscopic Ultrasound-Guided Biliary Drainage in Patients Undergoing Antithrombotic Therapy