Clin Exp Otorhinolaryngol.
2020 Aug;13(3):299-307. 10.21053/ceo.2019.01669.
Management of Laryngopharyngeal Reflux in Asia
- Affiliations
-
- 1Laryngopharyngeal Reflux Study Group of Young Otolaryngologists of the International Federation of Oto-rhino-laryngological Societies, Paris, France
- 2Department of Otolaryngology-Head and Neck Surgery, Kyung Hee University School of Medicine, Seoul, Korea
- 3Department of Anatomy and Experimental Oncology, Mons School of Medicine, UMONS Research Institute for Health Sciences and Technology, University of Mons, Mons, Belgium
- 4Department of Otorhinolaryngology and Head and Neck Surgery, CHU Saint-Pierre, Faculty of Medicine, Université Libre de Bruxelles, Brussels, Belgium
- 5Division of Otolaryngology-Head and Neck Surgery, Centre Hospitalier de l’Université de Montréal, Montreal, Québec, Canada
- 6Department of Otorhinolaryngology and Head and Neck Surgery, Shanghai Ninth People’s Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, China
- 7Larynx Function Laboratory, Department of Speech Therapy, School of Rehabilitation, Tehran University of Medical Sciences, Tehran, Iran
- 8Department of Otolaryngology, Marmara University Pendik Training and Research Hospital, Istanbul, Turkey
- 9Department of Otology, Neurotology and Skullbase Surgery, Madras ENT Research Foundation, Chennai, India
- 10Department of Otorhinolaryngology-Head and Neck Surgery, American University of Beirut Medical Center, Beirut, Lebanon
- KMID: 2504926
- DOI: http://doi.org/10.21053/ceo.2019.01669
Abstract
Objectives
. This study was conducted to investigate the current practices of Asian otolaryngologists for laryngopharyngeal reflux (LPR).
Methods
. An online survey about LPR was sent to 2,000 members of Asian otolaryngological societies, and a subgroup analysis was performed between Western and Eastern Asian otolaryngologists. The survey was conducted by the Laryngopharyngeal Reflux Study Group of Young Otolaryngologists of the International Federation of Oto-rhino-laryngological Societies.
Results
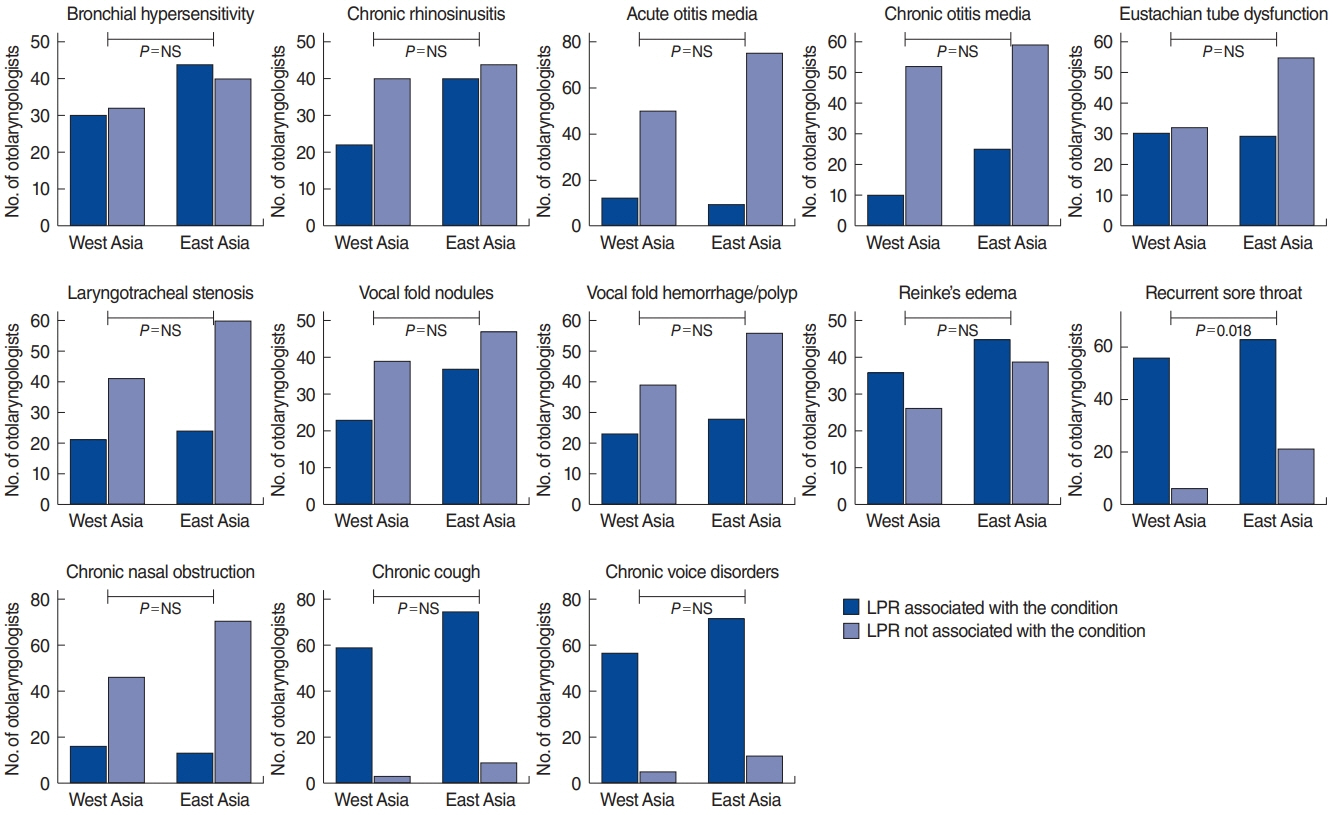
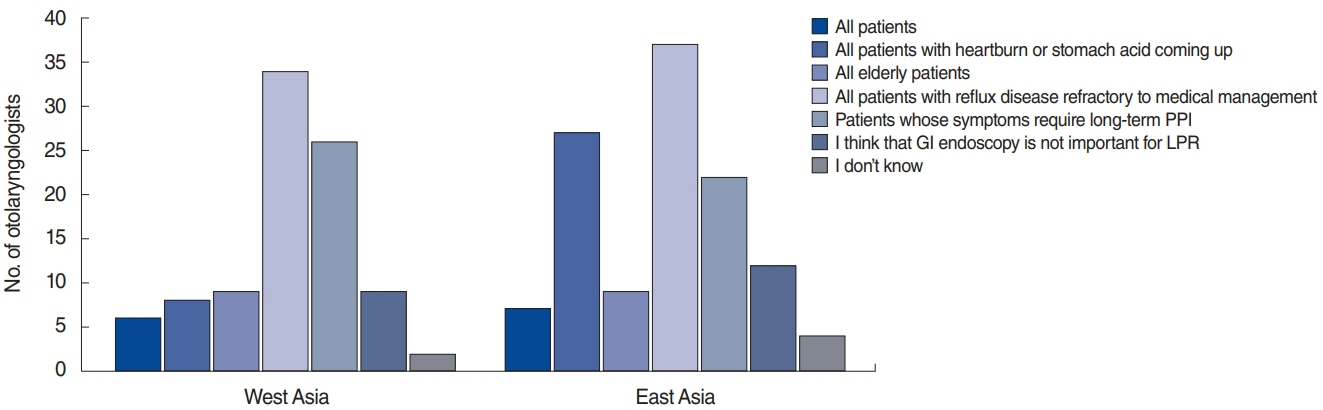
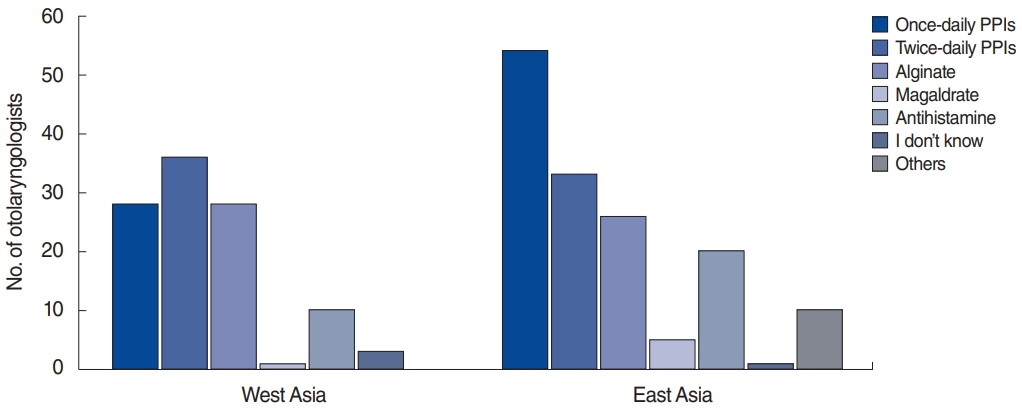
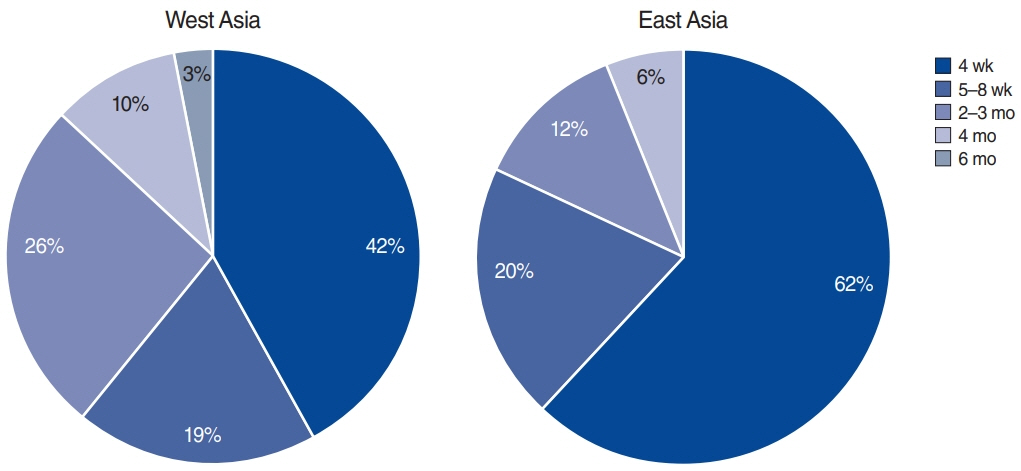
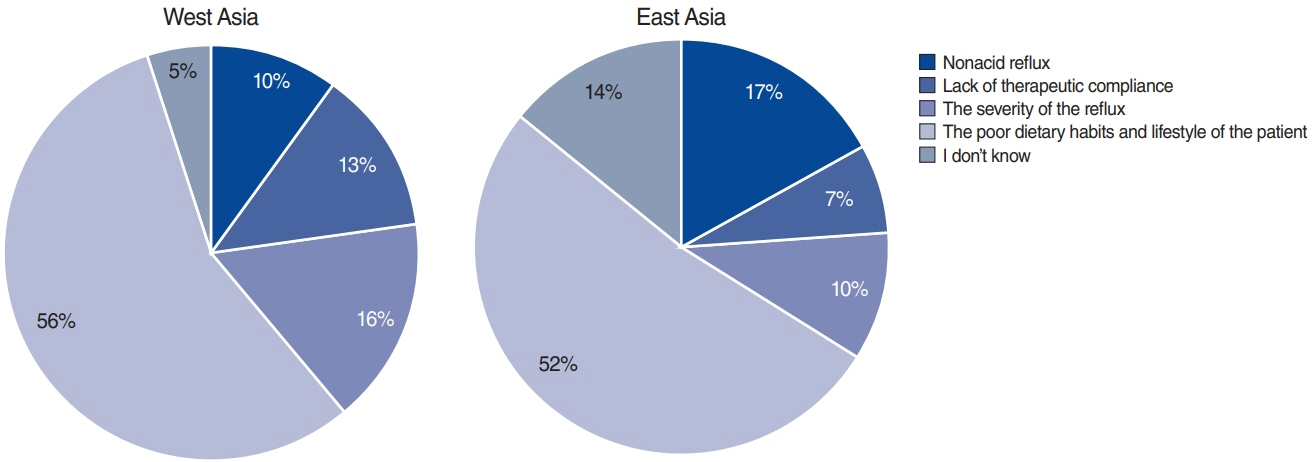
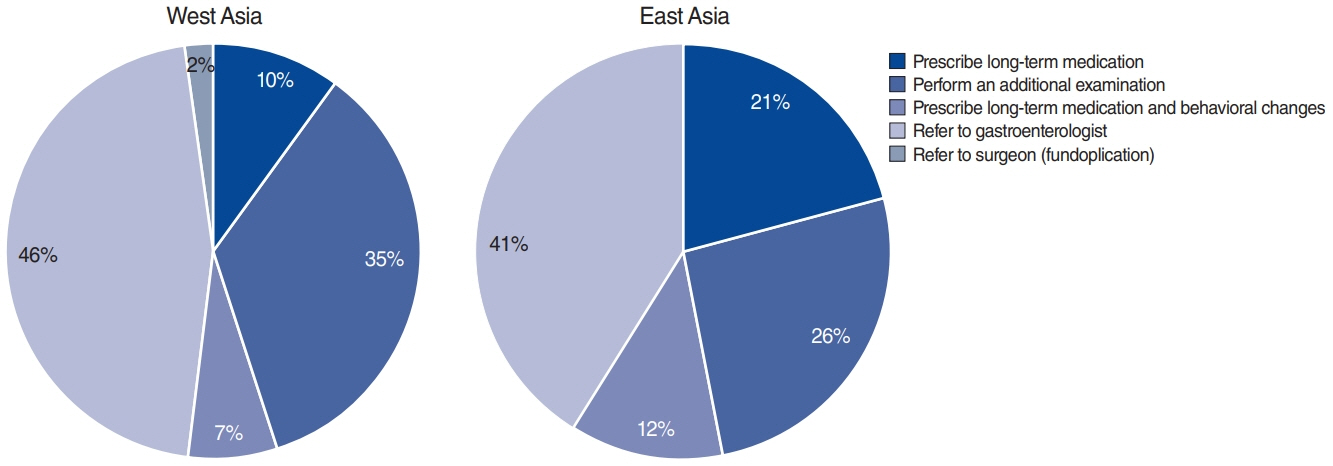
. Among approximately 1,600 Asian otolaryngologists, 146 completed the survey (62 from Western Asian countries, 84 from Eastern Asian countries). A substantial majority (73.3%) of the otolaryngologists considered LPR and gastroesophageal reflux disease to be different diseases. The symptoms thought to be closely related to LPR were coughing after lying down, throat clearing, and globus sensation. The findings thought to be closely related to LPR were posterior commissure granulations and hypertrophy, arytenoids, and laryngeal erythema. The respondents indicated that they mostly diagnosed LPR (70%) after an empirical therapeutic trial of proton pump inhibitors (PPIs). Although multichannel intraluminal impedance-pH (MII-pH) monitoring is a useful tool for diagnosing nonacid or mixed LPR, 78% of Asian otolaryngologists never or very rarely used MII-pH. Eastern Asian otolaryngologists more frequently used once-daily PPIs (64.3% vs. 45.2%, P=0.021), whereas Western Asian otolaryngologists preferred to use twice-daily PPIs (58.1% vs. 39.3%, P=0.025). The poor dietary habits of patients were considered to be the main reason for therapeutic failure by Asian otolaryngologists (53.8%). Only 48.6% of Asian otolaryngologists considered themselves to be adequately knowledgeable and skilled regarding LPR.
Conclusion
. Significant differences exist between Western and Eastern Asian otolaryngologists in the diagnosis and treatment of LPR. Future consensus statements are needed to establish diagnostic criteria and therapeutic regimens.
Keyword
Figure
Reference
-
1. Lechien JR, Saussez S, Schindler A, Karkos PD, Hamdan AL, Harmegnies B, et al. Clinical outcomes of laryngopharyngeal reflux treatment: a systematic review and meta-analysis. Laryngoscope. 2019; May. 129(5):1174–87.
Article2. Mosli M, Alkhathlan B, Abumohssin A, Merdad M, Alherabi A, Marglani O, et al. Prevalence and clinical predictors of LPR among patients diagnosed with GERD according to the reflux symptom index questionnaire. Saudi J Gastroenterol. 2018; Jul-Aug. 24(4):236–41.
Article3. Koufman JA, Aviv JE, Casiano RR, Shaw GY. Laryngopharyngeal reflux: position statement of the committee on speech, voice, and swallowing disorders of the American Academy of Otolaryngology-Head and Neck Surgery. Otolaryngol Head Neck Surg. 2002; Jul. 127(1):32–5.
Article4. Eusebi LH, Ratnakumaran R, Yuan Y, Solaymani-Dodaran M, Bazzoli F, Ford AC. Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: a meta-analysis. Gut. 2018; Mar. 67(3):430–40.
Article5. Kamani T, Penney S, Mitra I, Pothula V. The prevalence of laryngopharyngeal reflux in the English population. Eur Arch Otorhinolaryngol. 2012; Oct. 269(10):2219–25.
Article6. Spantideas N, Drosou E, Bougea A, Assimakopoulos D. Laryngopharyngeal reflux disease in the Greek general population, prevalence and risk factors. BMC Ear Nose Throat Disord. 2015; Dec. 15:7.
Article7. Chen XM, Li Y, Guo WL, Wang WT, Lu M. Prevalence of laryngopharyngeal reflux disease in Fuzhou region of China. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2016; Dec. 51(12):909–13.8. Kim SI, Kwon OE, Na SY, Lee YC, Park JM, Eun YG. Association between 24-hour combined multichannel intraluminal impedance-pH monitoring and symptoms or quality of life in patients with laryngopharyngeal reflux. Clin Otolaryngol. 2017; Jun. 42(3):584–91.
Article9. Lechien JR, Akst LM, Hamdan AL, Schindler A, Karkos PD, Barillari MR, et al. Evaluation and management of laryngopharyngeal reflux disease: state of the art review. Otolaryngol Head Neck Surg. 2019; May. 160(5):762–82.
Article10. Gupta N, Green RW, Megwalu UC. Evaluation of a laryngopharyngeal reflux management protocol. Am J Otolaryngol. 2016; May-Jun. 37(3):245–50.
Article11. Altman KW, Stephens RM, Lyttle CS, Weiss KB. Changing impact of gastroesophageal reflux in medical and otolaryngology practice. Laryngoscope. 2005; Jul. 115(7):1145–53.
Article12. Johnston N, Ondrey F, Rosen R, Hurley BP, Gould J, Allen J, et al. Airway reflux. Ann N Y Acad Sci. 2016; Oct. 1381(1):5–13.
Article13. Lechien JR, Bobin F, Muls V, Thill MP, Horoi M, Ostermann K, et al. Validity and reliability of the reflux symptom score. Laryngoscope. 2020; Mar. 130(3):E98–107.
Article14. Koufman JA. The otolaryngologic manifestations of gastroesophageal reflux disease (GERD): a clinical investigation of 225 patients using ambulatory 24-hour pH monitoring and an experimental investigation of the role of acid and pepsin in the development of laryngeal injury. Laryngoscope. 1991; Apr. 101(4 Pt 2 Suppl 53):1–78.15. Lechien JR, Mouawad F, Mortuaire G, Remacle M, Bobin F, Huet K, et al. Awareness of European otolaryngologists and general practitioners toward laryngopharyngeal reflux. Ann Otol Rhinol Laryngol. 2019; Nov. 128(11):1030–40.
Article16. Michaudet C, Malaty J. Chronic cough: evaluation and management. Am Fam Physician. 2017; Nov. 96(9):575–80.17. Wang JS, Li JR. The role of laryngopharyngeal reflux in the pathogenesis of Reinke’s edema. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2016; Dec. 30(24):1931–4.18. Alanazi R, Alrahim A, Bayounos S, Al-Ghuwainem A, Al-Bar MH. Association between voice handicap index and reflux symptom index: a cross-sectional study of undiagnosed general and teacher cohorts in Saudi Arabia. Sultan Qaboos Univ Med J. 2018; Aug. 18(3):e350–4.
Article19. Lechien JR, Finck C, Khalife M, Huet K, Delvaux V, Picalugga M, et al. Change of signs, symptoms and voice quality evaluations throughout a 3- to 6-month empirical treatment for laryngopharyngeal reflux disease. Clin Otolaryngol. 2018; Oct. 43(5):1273–82.
Article20. Jiang SP, Liang RY, Zeng ZY, Liu QL, Liang YK, Li JG. Effects of antireflux treatment on bronchial hyper-responsiveness and lung function in asthmatic patients with gastroesophageal reflux disease. World J Gastroenterol. 2003; May. 9(5):1123–5.
Article21. Miura MS, Mascaro M, Rosenfeld RM. Association between otitis media and gastroesophageal reflux: a systematic review. Otolaryngol Head Neck Surg. 2012; Mar. 146(3):345–52.22. Al-Saab F, Manoukian JJ, Al-Sabah B, Almot S, Nguyen LH, Tewfik TL, et al. Linking laryngopharyngeal reflux to otitis media with effusion: pepsinogen study of adenoid tissue and middle ear fluid. J Otolaryngol Head Neck Surg. 2008; Aug. 37(4):565–71.23. Lechien JR, Saussez S, Nacci A, Barillari MR, Rodriguez A, Le Bon SD, et al. Association between laryngopharyngeal reflux and benign vocal folds lesions: a systematic review. Laryngoscope. 2019; 129(9):E329–41.
Article24. Toohill RJ, Ulualp SO, Shaker R. Evaluation of gastroesophageal reflux in patients with laryngotracheal stenosis. Ann Otol Rhinol Laryngol. 1998; Dec. 107(12):1010–4.
Article25. Loehrl TA, Samuels TL, Poetker DM, Toohill RJ, Blumin JH, Johnston N. The role of extraesophageal reflux in medically and surgically refractory rhinosinusitis. Laryngoscope. 2012; Jul. 122(7):1425–30.
Article26. Lee YC, Kwon OE, Park JM, Eun YG. Do laryngoscopic findings reflect the characteristics of reflux in patients with laryngopharyngeal reflux. Clin Otolaryngol. 2018; Feb. 43(1):137–43.
Article27. Chang BA, MacNeil SD, Morrison MD, Lee PK. The reliability of the reflux finding score among general otolaryngologists. J Voice. 2015; Sep. 29(5):572–7.
Article28. Koufman JA. Laryngopharyngeal reflux is different from classic gastroesophageal reflux disease. Ear Nose Throat J. 2002; Sep. 81(9 Suppl 2):7–9.29. Jaspersen D, Kulig M, Labenz J, Leodolter A, Lind T, Meyer-Sabellek W, et al. Prevalence of extra-oesophageal manifestations in gastro-oesophageal reflux disease: an analysis based on the ProGERD Study. Aliment Pharmacol Ther. 2003; Jun. 17(12):1515–20.
Article30. Patel D, Vaezi MF. Normal esophageal physiology and laryngopharyngeal reflux. Otolaryngol Clin North Am. 2013; Dec. 46(6):1023–41.
Article31. Guo H, Ma H, Wang J. Proton pump inhibitor therapy for the treatment of laryngopharyngeal reflux: a meta-analysis of randomized controlled trials. J Clin Gastroenterol. 2016; Apr. 50(4):295–300.32. Park W, Hicks DM, Khandwala F, Richter JE, Abelson TI, Milstein C, et al. Laryngopharyngeal reflux: prospective cohort study evaluating optimal dose of proton-pump inhibitor therapy and pretherapy predictors of response. Laryngoscope. 2005; Jul. 115(7):1230–8.
Article33. Yoon YH, Park KW, Lee SH, Park HS, Chang JW, Koo BS. Efficacy of three proton-pump inhibitor therapeutic strategies on laryngopharyngeal reflux disease; a prospective randomized double-blind study. Clin Otolaryngol. 2019; Jul. 44(4):612–8.
Article34. Postma GN, Johnson LF, Koufman JA. Treatment of laryngopharyngeal reflux. Ear Nose Throat J. 2002; Sep. 81(9 Suppl 2):24–6.35. Koufman JA. Low-acid diet for recalcitrant laryngopharyngeal reflux: therapeutic benefits and their implications. Ann Otol Rhinol Laryngol. 2011; May. 120(5):281–7.
Article36. Zalvan CH, Hu S, Greenberg B, Geliebter J. A comparison of alkaline water and Mediterranean diet vs proton pump inhibition for treatment of laryngopharyngeal reflux. JAMA Otolaryngol Head Neck Surg. 2017; Oct. 143(10):1023–9.
Article37. Lechien JR, Huet K, Khalife M, De Marrez LG, Finck C, Harmegnies B, et al. Alkaline, protein, low-fat and low-acid diet in laryngopharyngeal reflux disease: our experience on 65 patients. Clin Otolaryngol. 2019; May. 44(3):379–84.
Article38. Pisegna JM, Yang S, Purcell A, Rubio A. A mixed-methods study of patient views on reflux symptoms and medication routines. J Voice. 2017; May. 31(3):381.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Usefulness of Esophagography as a Screening Test for Laryngopharyngeal Reflux
- The Management of Laryngopharyngeal Reflux Disease
- Mapping Regional Laryngopharyngeal Mechanoreceptor Response
- Ultra-Structural and Molecular Aspects of Laryngopharyngeal Reflux
- Clinical Manifestations of Laryngopharyngeal Reflux