Ann Rehabil Med.
2020 Jun;44(3):203-209. 10.5535/arm.19140.
Changes in Pharyngeal Width Over Time as an Indicator of Dysphagia in Stroke Patients
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea
- KMID: 2504440
- DOI: http://doi.org/10.5535/arm.19140
Abstract
Objective
To verify the pharyngeal width at rest as a measurement that could be used to assess changes in the degree of dysphagia over time in stroke patients.
Methods
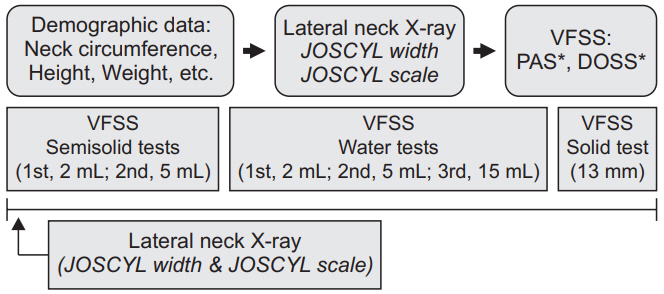
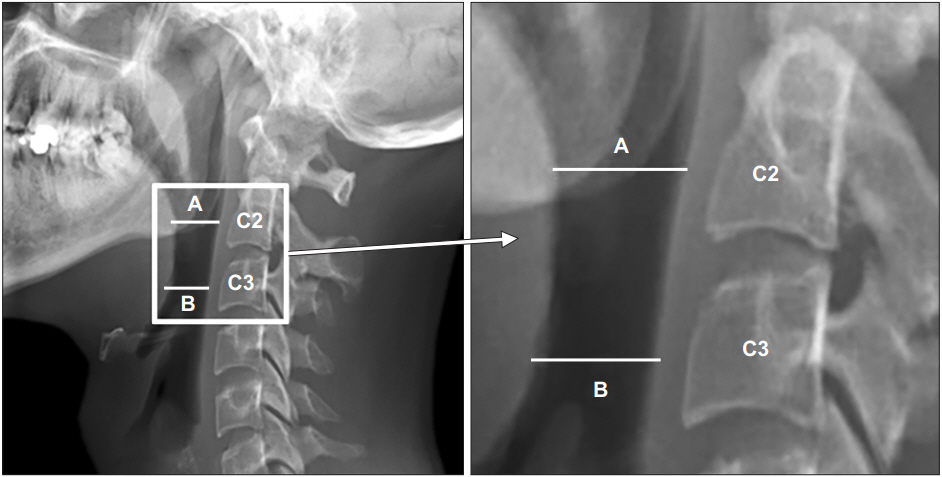
In a cohort of stroke patients, we performed serial measurements of the pharyngeal width at the midpoints of the second (C2) and third (C3) cervical vertebral bodies using lateral neck X-rays while the patients were at rest. The JOSCYL width, a parameter named after the first initial of each developers’ surname and defined as the average value of the upper and lower pharyngeal widths, was used to formulate the JOSCYL scale, which was calculated as the JOSCYL width × 100/neck circumference. All patients also underwent serial videofluoroscopic swallowing studies (VFSSs). The Spearman correlation analysis was used to detect correlations between the serial VFSS results, JOSCYL widths, and JOSCYL scale values.
Results
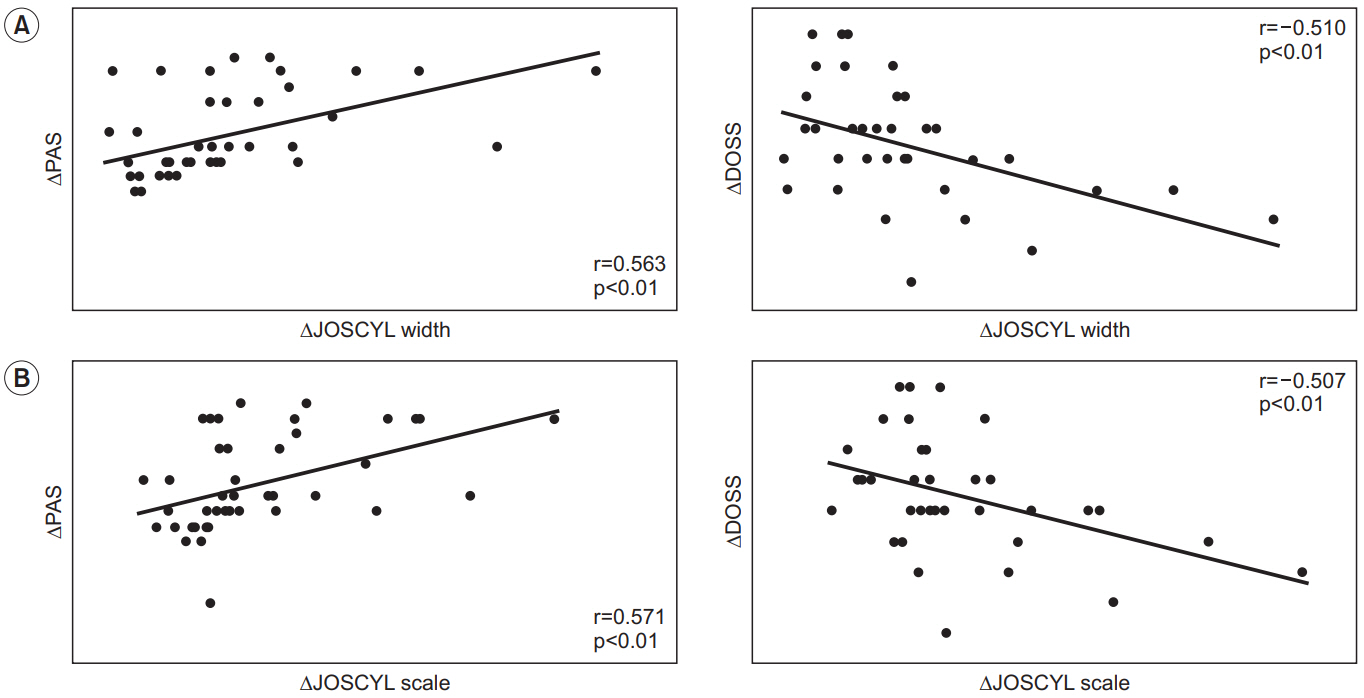
Over time, we observed significant positive and negative correlations of change in the JOSCYL width and scale with changes in the Penetration-Aspiration Scale and the Dysphagia Outcome and Severity Scale scores, respectively.
Conclusion
The JOSCYL width and JOSCYL scale clearly reflected changes in dysphagia in stroke patients over time. These parameters may provide an easier method for evaluating whether post-stroke dysphagia has been alleviated.
Keyword
Figure
Reference
-
1. Kim AS, Cahill E, Cheng NT. Global stroke belt: geographic variation in stroke burden worldwide. Stroke. 2015; 46:3564–70.2. Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005; 36:2756–63.3. Papadopoulou SL, Ploumis A, Exarchakos G, Theodorou SJ, Beris A, Fotopoulos AD. Versatility of repetitive transcranial magnetic stimulation in the treatment of poststroke dysphagia. J Neurosci Rural Pract. 2018; 9:391–6.
Article4. Smithard DG, O’Neill PA, Parks C, Morris J. Complications and outcome after acute stroke. Does dysphagia matter? Stroke. 1996; 27:1200–4.5. Lan Y, Xu G, Dou Z, Lin T, Yu F, Jiang L. The correlation between manometric and videofluoroscopic measurements of the swallowing function in brainstem stroke patients with dysphagia. J Clin Gastroenterol. 2015; 49:24–30.
Article6. Gomes GF, Campos AC, Pisani JC, Macedo ED, Vieira MC. Diagnostic methods for the detection of anterograde aspiration in enterally fed patients. Curr Opin Clin Nutr Metab Care. 2004; 7:285–92.
Article7. Dodds WJ. Physiology of swallowing. Dysphagia. 1989; 3:171–8.8. Mu L, Sanders I. Neuromuscular specializations within human pharyngeal constrictor muscles. Ann Otol Rhinol Laryngol. 2007; 116:604–17.
Article9. Jung IH, Lee HY, Cha E, Song J, Baek S, Jung KI, et al. Pharyngeal width and aspiration after stroke. Int J Rehabil Res. 2019; 42:152–9.
Article10. Lee HY, Jung IH, Cha E, Song J, Jung KI, Yoo WK, et al. Predictive value of pharyngeal width at rest (JOSCYL Width) for aspiration in elderly people. Ann Rehabil Med. 2019; 43:187–94.
Article11. Curtis JA, Molfenter SM, Troche MS. Pharyngeal area changes in Parkinson’s disease and its effect on swallowing safety, efficiency, and kinematics. Dysphagia. 2020; 35:389–98.
Article12. Nicosia MA, Robbins J. The usefulness of the line spread test as a measure of liquid consistency. Dysphagia. 2007; 22:306–11.
Article13. Edmiaston J, Connor LT, Loehr L, Nassief A. Validation of a dysphagia screening tool in acute stroke patients. Am J Crit Care. 2010; 19:357–64.
Article14. Han TR, Paik NJ, Park JW. Quantifying swallowing function after stroke: a functional dysphagia scale based on videofluoroscopic studies. Arch Phys Med Rehabil. 2001; 82:677–82.
Article15. Eisenhuber E, Schima W, Schober E, Pokieser P, Stadler A, Scharitzer M, et al. Videofluoroscopic assessment of patients with dysphagia: pharyngeal retention is a predictive factor for aspiration. AJR Am J Roentgenol. 2002; 178:393–8.16. Jaffer NM, Ng E, Au FW, Steele CM. Fluoroscopic evaluation of oropharyngeal dysphagia: anatomic, technical, and common etiologic factors. AJR Am J Roentgenol. 2015; 204:49–58.
Article17. Jones B. Radiologic evaluation of the dysphagic patient. Nutr Clin Pract. 1999; 14:S10–S12.
Article18. Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996; 11:93–8.
Article19. O’Neil KH, Purdy M, Falk J, Gallo L. The dysphagia outcome and severity scale. Dysphagia. 1999; 14:139–45.
Article20. Horiguchi S, Suzuki Y. Screening tests in evaluating swallowing function. Japan Med Assoc J. 2011; 54:31–4.21. Leigh JH, Lim JY, Han MK, Bae HJ, Kim WS, Paik NJ. A prospective comparison between bedside swallowing screening test and videofluoroscopic swallowing study in post-stroke dysphagia. Brain Neurorehabil. 2016; Sep. 9(2):e7.
Article22. Kendall KA, Leonard RJ. Pharyngeal constriction in elderly dysphagic patients compared with young and elderly nondysphagic controls. Dysphagia. 2001; 16:272–8.
Article23. Stokely SL, Peladeau-Pigeon M, Leigh C, Molfenter SM, Steele CM. The relationship between pharyngeal constriction and post-swallow residue. Dysphagia. 2015; 30:349–56.
Article24. Molfenter SM, Lenell C, Lazarus CL. Volumetric changes to the pharynx in healthy aging: consequence for pharyngeal swallow mechanics and function. Dysphagia. 2019; 34:129–37.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Dysphagia Between Infratentorial and Supratentorial Stroke Patients
- Relationship between Generalized Sarcopenia and the Severity of Dysphagia after a Stroke
- The Usefulness of the Dynamic Image of the Pharynx with Digital Radiography in Dysphagia Following Stroke
- Epidemiology, Natural Recovery, Long-term Outcome of Post Stroke Dysphagia
- Lesion Characteristics of Chronic Dysphagia in Patients With Supratentorial Stroke