J Cerebrovasc Endovasc Neurosurg.
2020 Jun;22(2):97-105. 10.7461/jcen.2020.22.2.97.
A safer endovascular technique for pre-operative embolization of juvenile nasopharyngeal angiofibroma: avoiding the pitfalls of external carotid artery – internal carotid artery anastomoses
- Affiliations
-
- 1Department of Neurology, University of Texas Medical School at Houston, Houston, TX, USA
- 2Department of Neurosurgery, Mayo Clinic, Pheonix, AZ, USA
- 3Deptartment of Clinical Research, University of Chicago, Chicago, IL, USA
- 4Department of Neurosurgery, University of Texas Medical School at Houston, Houston, TX, USA
- 5Department of Otorhinolaryngology, University of Texas Medical School at Houston, Houston, TX, USA
- KMID: 2503823
- DOI: http://doi.org/10.7461/jcen.2020.22.2.97
Abstract
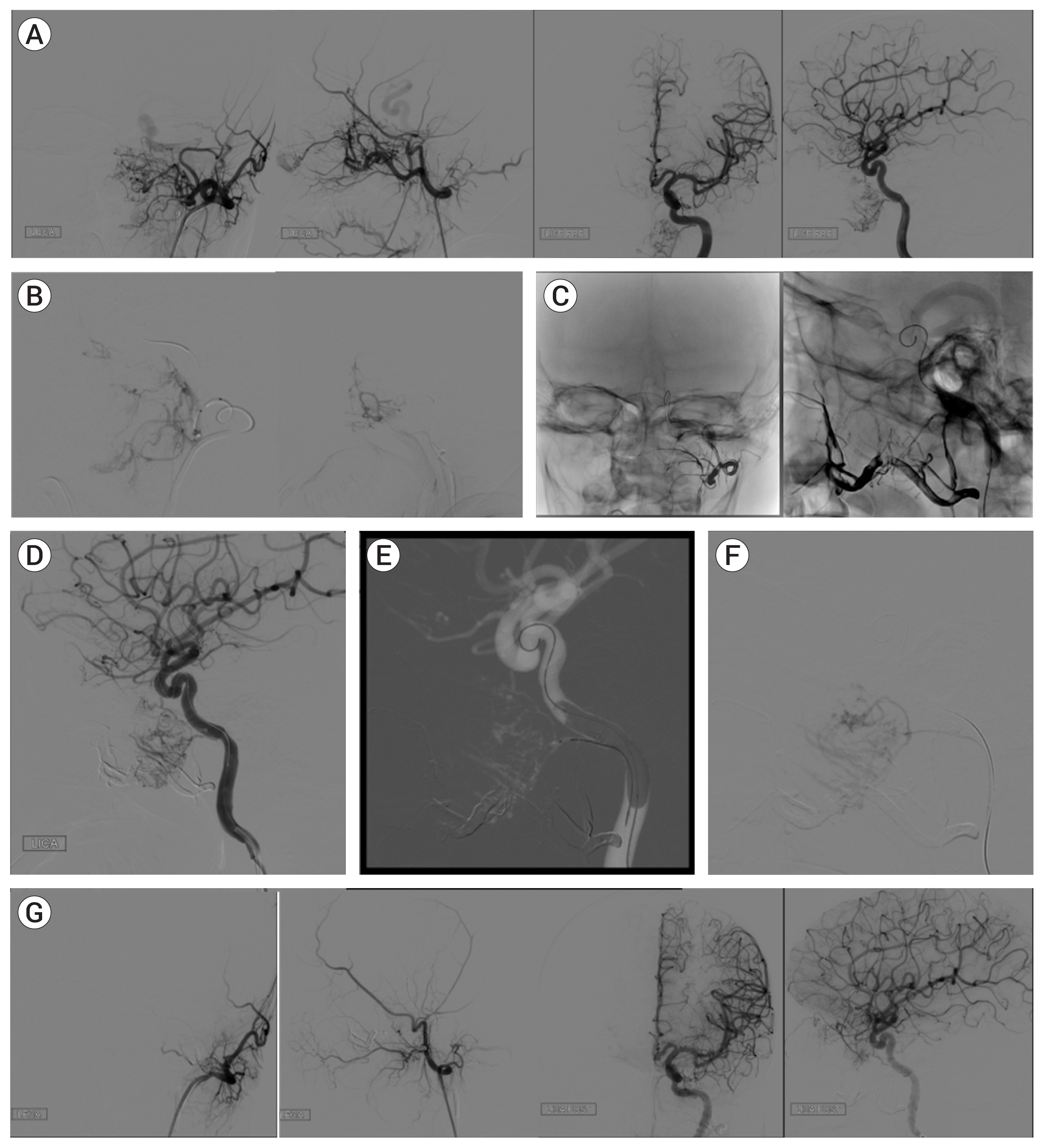
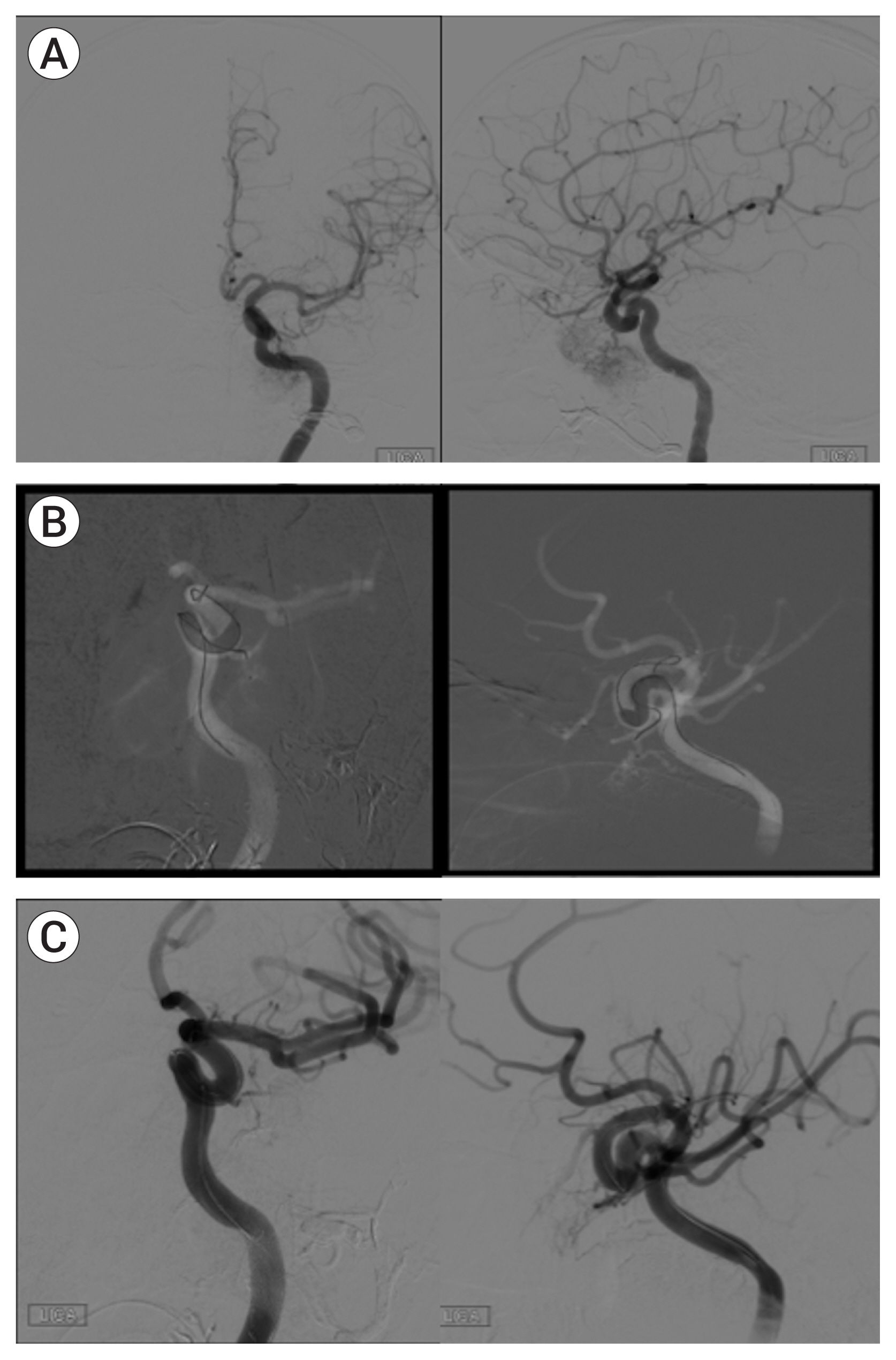
- Intra-arterial embolization of juvenile nasopharyngeal angiofibroma (JNA) prior to surgical resection is the preferred approach to minimize blood loss during surgical resection of the tumor. However, the presence of external carotid artery–internal carotid artery (ECA-ICA) anastomoses may hinder complete tumor embolization due to the associated risk for embolic complications. Here, we evaluate the use of a balloon-assisted embolization (BAE) technique in the treatment of JNA. We conducted a retrospective review of JNA patients who underwent tumor embolization with injection of Onyx in a single session between 2013-2018. All cases displayed tumor arterial supply from ECA and ICA circulations on 2-D catheter angiograms. Procedural and surgical outcome data were analyzed. Results are given as mean±- standard deviation (range). Among 9 patients with JNA, all were males and mean age was 14.1±6.3 years (range, 9-29 years). The mean tumor volume embolization was 84.4±12.4% (range, 60-100%) and in 89% patients ≥80% of tumor volume embolization was achieved. There were no embolization-related complications reported. During surgical resection of the tumor there was a low average surgical blood loss of 722±651.5 mL (range, 50-2,000 mL) and the mean procedure time was 282.6±85.4 mins (range, 151-403 mins). In this series, the BAE technique showed to be a safe and effective approach to achieve successful tumor embolization while avoiding embolic complications and effectively reducing the risk for blood loss during surgical resection.
Keyword
Figure
Reference
-
1. Beham A, BehamSchmid C, Regauer S, Auböck L, Stammberger H. Nasopharyngeal Angiofibroma: True Neoplasm or Vascular Malformation? Adv Anat Pathol. 2000; Jan. 7(1):36–46.
Article2. Berenstein A, Lasjaunias P, Kricheff II. Functional anatomy of the facial vasculature in pathologic conditions and its therapeutic application. AJNR Am J Neuroradiol. 1983; Mar–Apr. 4(2):149–53.3. Borota L, Mahmoud E, Nyberg C, Ekberg T. Combined percutaneous and transarterial devascularisation of juvenile nasopharyngeal angiofibroma with protection of internal carotid artery: A modification of the technique. Interv Neuroradiol. 2015; Jun. 21(3):390–6.
Article4. Casasco A, Herbreteau D, Houdart E, George B, Tran Ba, Huy P, Deffresne D, et al. Devascularization of craniofacial tumors by percutaneous tumor puncture. AJNR Am J Neuroradiol. 1994; Aug. 15(7):1233–9.5. Casasco A, Houdart E, Biondi A, Jhaveri HS, Herbreteau D, Aymard A, et al. Major complications of percutaneous embolization of skull-base tumors. AJNR Am J Neuroradiol. 1999; Jan. 20(1):179–81.6. Chen P, Ortiz R, Page JH, Siddiqui AH, Veznedaroglu E, Rosenwasser RH. Spontaneous systolic blood pressure elevation during temporary balloon occlusion increases the risk of ischemic events after carotid artery occlusion. Neurosurgery. 2008; Aug. 63(2):256–64.
Article7. Countee RW, Vijayanathan T. External carotid artery in internal carotid artery occlusion. Angiographic, therapeutic, and prognostic considerations. Stroke. 1979; Jul. 10(4):450–60.
Article8. Coyas A, Tzagarakis M, Giorgis G, Katsiotis P. Transcatheter arterial embolization as a preoperative procedure in the management of juvenile angiofibroma. Rhinology. 1979; Dec. 17(4):265–70.9. Elhammady MS, Johnson JN, Peterson EC, Aziz-Sultan MA. Preoperative embolization of juvenile nasopharyngeal angiofibromas: transarterial versus direct tumoral puncture. World Neurosurg. 2011; Sep–Oct. 76(3–4):328–34.
Article10. Gao M, Gemmete JJ, Chaudhary N, Pandey AS, Sullivan SE, McKean EL, et al. A comparison of particulate and onyx embolization in preoperative devascularization of juvenile nasopharyngeal angiofibromas. Neuroradiology. 2013; Sep. 55(9):1089–96.
Article11. Gay I, Elidan J, Gordon R. Oronasal fistula–a possible complication of pre-operation embolization in the management of juvenile nasopharyngeal angiofibroma. J Laryngol Otol. 1983; Jul. 97(7):651–6.
Article12. Geibprasert S, Pongpech S, Armstrong D, Krings T. Dangerous extracranial-intracranial anastomoses and supply to the cranial nerves: vessels the neurointerventionalist needs to know. AJNR Am J Neuroradiol. 2009; Sep. 30(8):1459–68.
Article13. Krishnamoorthy T, Gupta AK, Rajan JE, Thomas B. Stroke from delayed embolization of polymerized glue following percutaneous direct injection of a carotid body tumor. Korean J Radiol. 2007; May–Jun. 8(3):249–53.
Article14. Monga SP, Wadleigh R, Sharma A, Adib H, Strader D, Singh G, et al. Intratumoral therapy of cisplatin/epinephrine injectable gel for palliation in patients with obstructive esophageal cancer. Am J Clin Oncol. 2000; Aug. 23(4):386–92.
Article15. Naithani P, Khanduja S, Sinha S, Khanduja N, Naithani P. n-Butyl cyanoacrylate-induced multiple retinal arteriolar occlusions. Int Ophthalmol. 2013; Oct. 33(5):599–600.
Article16. Perrini P, Cardia A, Fraser K, Lanzino G. A microsurgical study of the anatomy and course of the ophthalmic artery and its possibly dangerous anastomoses. J Neurosurg. 2007; Jan. 106(1):142–50.
Article17. Radkowski D, McGill T, Healy GB, Ohlms L, Jones DT. Angiofibroma. Changes in staging and treatment. Arch Otolaryngol Head Neck Surg. 1996; Feb. 122(2):122–9.
Article18. Ramezani A, Haghighatkhah H, Moghadasi H, Taheri M, Parsafar H. A case of central retinal artery occlusion following embolization procedure for juvenile nasopharyngeal angiofibroma. Indian J Ophthalmol. 2010; Sep–Oct. 58(5):419–21.
Article19. Siddiqui AH, Chen PR. Intracranial collateral anastomoses: relevance to endovascular procedures. Neurosurg Clin N Am. 2009; Jul. 20(3):279–96.
Article20. Trivedi M, Desai RJ, Potdar NA, Shinde CA, Ukirde V, Bhuta M, et al. Vision loss due to central retinal artery occlusion following embolization in a case of a giant juvenile nasopharyngeal angiofibroma. J Craniofac Surg. 2015; Jul. 26(5):e451–3.
Article21. Valavanis A. Preoperative embolization of the head and neck: indications, patient selection, goals, and precautions. AJNR Am J Neuroradiol. 1986; Sep–Oct. 7(5):943–52.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anglographic Findings of Collateral Vessels in Cervicofacial Vascular Lesions with Previously Ligated Carotid Artery
- Congenital External Carotid-Internal Carotid Artery Anastomosis
- Preoperative Embolization of Hypervascular Brain Tumor Fed by Branches of the Internal Carotid Artery
- Traumatic Pseudoaneurysm of the External and Internal Carotid Artery Presenting as Epistaxis: Case Report
- Embolization of a Bleeding Maxillary Arteriovenous Malformation via the Superficial Temporal Artery after External Carotid Artery Ligation