Ann Surg Treat Res.
2020 Jul;99(1):1-7. 10.4174/astr.2020.99.1.1.
Operation start time and long-term outcome of hepatocellular carcinoma after curative hepatic resection
- Affiliations
-
- 1Department of Hepatobiliary Surgery, Institute of Advanced Surgical Technology and Engineering, The First Affiliated Hospital of Xi’an Jiaotong University, Shaanxi Province, China
- 2Shaanxi Provincial Regenerative Medicine and Surgical Engineering Research Center, Xi’an, Shaanxi Province, China
- KMID: 2503454
- DOI: http://doi.org/10.4174/astr.2020.99.1.1
Abstract
- Purpose
The objective of the current study was to examine the potential effects of surgery start times (morning vs. afternoon) on the long-term prognosis of patients after hepatic resection (HR) for hepatocellular carcinoma (HCC).
Methods
All eligible patients were divided into 2 groups according to the start time of surgery: group M (morning surgery, 8 AM–1 PM) and group A (afternoon surgery, 1 PM–6 PM). Clinicopathologic and surgical parameters, as well as oncologic outcomes were compared between the 2 groups.
Results
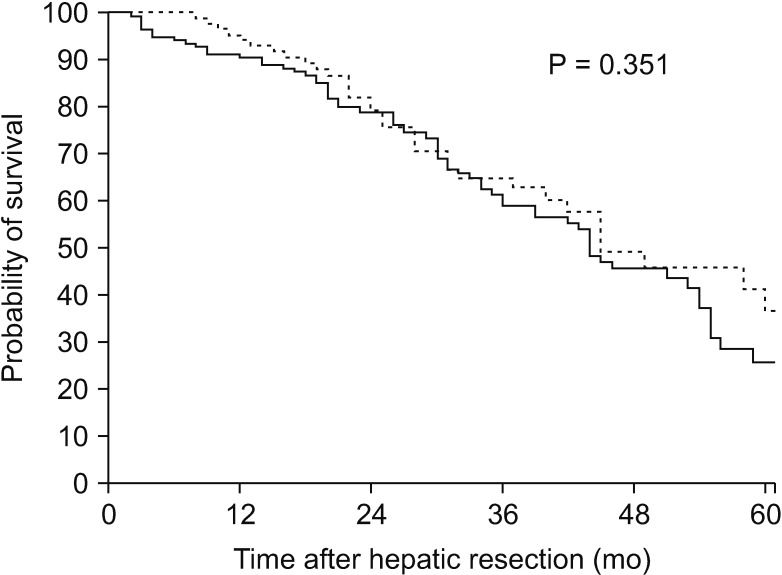
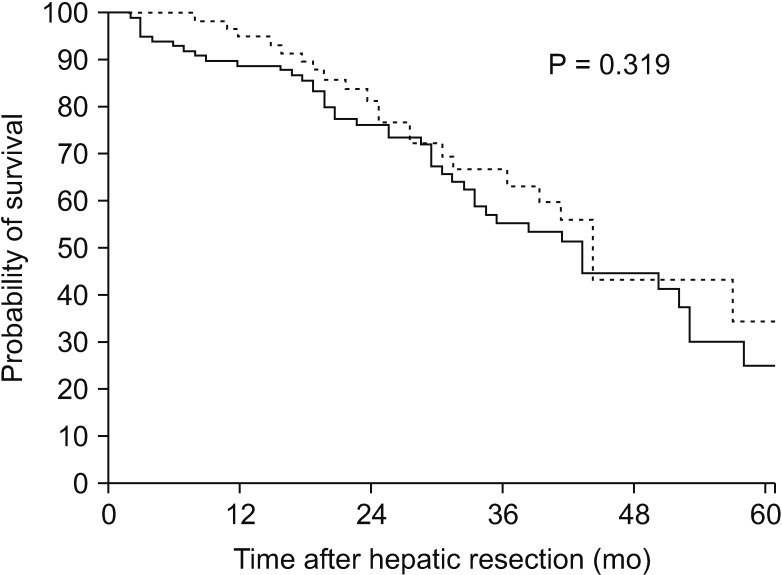
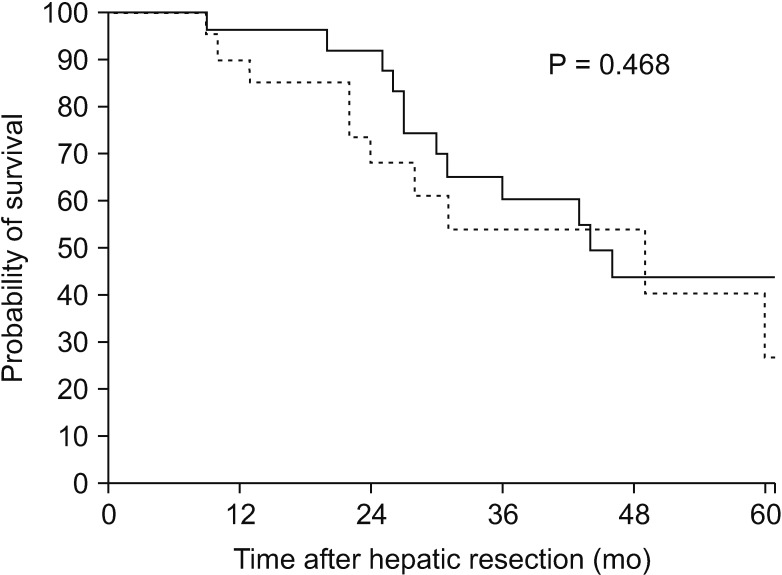
In total, 231 patients were included in the study. There was no difference in age, body mass index, comorbidities, tumor size, tumor location, tumor stages, surgical procedures, or surgical margin between morning and afternoon surgery (all P > 0.05). In contrast, patients in group M experienced longer operation duration than those in group A (median, 240 minutes vs. 195 minutes, P = 0.004). However, no differences of overall survival were observed between morning and afternoon surgery groups in the whole cohort or stratified by surgical margin (all P > 0.05).
Conclusion
Surgery start times during the work day have no measurable influence on patient outcome following curative HR for HCC, indicating good self-regulation and professional judgment of surgeons for progressive fatigue during surgery.
Keyword
Figure
Reference
-
1. Bigourdan Jean-Marc, Jaeck Daniel, Meyer Nicolas, Meyer Carole, Oussoultzoglou Elie, Bachellier Philippe, et al. Small hepatocellular carcinoma in child A cirrhotic patients: hepatic resection versus transplantation. Liver Transpl. 2003; 9:513–520. PMID: 12740796.2. Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996; 334:693–699. PMID: 8594428.3. Zhou Li, Rui Jing-An, Wang Shao-Bin, Chen Shu-Guang, Qu Qiang. Early recu rrence in large hepatocellular carcinoma after curative hepatic resection: prog nostic significance and risk factors. Hepatogastroenterology. 2014; 61:2035–2041. PMID: 25713907.4. Benzoni Enrico, Lorenzin Dario, Favero Alessandro, Adani Gianluigi, Baccarani Umberto, Molaro Roberta, et al. Liver resection for hepatocellular carcinoma: a multivariate analysis of factors associated with improved prognosis. The role of clinical, pathological and surgical related factors. Tumori. 2007; 93:264–268. PMID: 17679461.5. Sturm Lana, Dawson Drew, Vaughan Richard, Hewett Peter, Hill Andrew G, Graham John C, et al. Effects of fatigue on surgeon performance and surgical outcomes: a systematic review. ANZ J Surg. 2011; 81:502–509. PMID: 22295360.6. Strunk CL, Bailey BJ, Scott BA, Cummings CW, Lucente FE, Beatty CW, et al. Resident work hours and working environment in otolaryngology. Analysis of daily activity and resident perception. JAMA. 1991; 266:1371–1374. PMID: 1880867.7. Whang EE, Perez A, Ito H, Mello MM, Ashley SW, Zinner MJ. Work hours reform: perceptions and desires of contemporary surgical residents. J Am Coll Surg. 2003; 197:624–630. PMID: 14522334.8. Goel N, Basner M, Rao H, Dinges DF. Circadian rhythms, sleep deprivation, and human performance. Prog Mol Biol Transl Sci. 2013; 119:155–190. PMID: 23899598.9. Landrigan CP, Rothschild JM, Cronin JW, Rainu Kaushal, Elisabeth Burdick, Joel T Katz, et al. Effect of reducing interns' work hours on serious medical errors in intensive care units. N Engl J Med. 2004; 351:1838–1848. PMID: 15509817.10. Lockley SW, Cronin JW, Evans EE, Cade BE, Lee CJ, Landrigan CP, et al. Effect of reducing interns' weekly work hours on sleep and attentional failures. N Engl J Med. 2004; 351:1829–1837. PMID: 15509816.11. Fisman DN, Harris AD, Rubin M, Sorock GS, Mittleman MA. Fatigue increases the risk of injury from sharp devices in medical trainees: results from a casecrossover study. Infect Control Hosp Epidemiol. 2007; 28:10–17. PMID: 17230382.12. Barger LK, Ayas NT, Cade BE, Cronin JW, Rosner B, Speizer FE, et al. Impact of extended-duration shifts on medical errors, adverse events, and attentional failures. PLoS Med. 2006; 3:e487. PMID: 17194188.13. Ayas NT, Barger LK, Cade BE, Hashimoto DM, Rosner B, Cronin JW, et al. Extended work duration and the risk of selfreported percutaneous injuries in interns. JAMA. 2006; 296:1055–1062. PMID: 16954484.14. Sanaka MR, Shah N, Mullen KD, Ferguson DR, Thomas C, McCullough AJ. Afternoon colonoscopies have higher failure rates than morning colonoscopies. Am J Gastroenterol. 2006; 101:2726–2730. PMID: 17227519.15. Gurudu SR, Ratuapli SK, Leighton JA, Heigh RI, Crowell MD. Adenoma detection rate is not influenced by the timing of colonoscopy when performed in half-day blocks. Am J Gastroenterol. 2011; 106:1466–1471. PMID: 21502998.16. Teng TY, Khor SN, Kailasam M, Cheah WK, Lau CC. Morning colonoscopies are associated with improved adenoma detection rates. Surg Endosc. 2016; 30:1796–1803. PMID: 26198158.17. Wright MC, Phillips-Bute B, Mark JB, Stafford-Smith M, Grichnik KP, Andregg BC, et al. Time of day effects on the incidence of anesthetic adverse events. Qual Saf Health Care. 2006; 15:258–263. PMID: 16885250.18. Lu Q, Shen Y, Zhang J, Ren YF, Dong J, Du ZQ, et al. Operation start times and postoperative morbidity from liver resection: a propensity score matching analysis. World J Surg. 2017; 41:1100–1109. PMID: 27878349.19. Ellman PI, Kron IL, Alvis JS, Tache-Leon C, Maxey TS, Reece TB, et al. Acute sleep deprivation in the thoracic surgical resident does not affect operative outcomes. Ann Thorac Surg. 2005; 80:60–64. PMID: 15975341.20. Ellman PI, Law MG, Tache-Leon C, Reece TB, Maxey TS, Peeler BB, et al. Sleep eprivation does not affect operative results in cardiac surgery. Ann Thorac Surg. 2004; 78:906–911. PMID: 15337018.21. Govindarajan A, Urbach DR, Kumar M, Li Q, Murray BJ, Juurlink D, et al. Outcomes of daytime procedures performed by attending surgeons after night work. N Engl J Med. 2015; 373:845–853. PMID: 26308685.22. You DD, Kim DG, Seo CH, Choi HJ, Yoo YK, Park YG. Prognostic factors after curative resection hepatocellular carcinoma and the surgeon's role. Ann Surg Treat Res. 2017; 93:252–259. PMID: 29184878.23. Amin MB, Edge SB. AJCC cancer staging manual. New York: Springer;2017.24. Llovet JM, Brú C, Bruix J. Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis. 1999; 19:329–338. PMID: 10518312.25. Pang YY. The Brisbane 2000 terminology of liver anatomy and resections. HPB 2000; 2:333–39. HPB (Oxford). 2002; 4:99. author reply 99–100. PMID: 18332933.26. Kim JM, Yi NJ, Kwon CHD, Lee KW, Suh KS, Joh JW. Early disseminated recurrence after liver resection in solitary hepatocellular carcinoma. Ann Surg Treat Res. 2018; 94:129–134. PMID: 29520346.27. Slaughter KN, Frumovitz M, Schmeler KM, Nick AM, Fleming ND, dos Reis R, et al. Minimally invasive surgery for endometrial cancer: does operative start time impact surgical and oncologic outcomes. Gynecol Oncol. 2014; 134:248–252. PMID: 24945591.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Long Term Survival in Patient with Early Intrahepatic Recurrence and Extrahepatic Metastasis after Curative Resection of Hepatocellular Carcinoma
- Outcome of Hepatic Resection for Hepatocellular Carcinoma within the Milan Criteria in Child-Pugh Class A Patients
- Saftey and Long-term Outcome following Major Hepatectomy for Hepatocellular Carcinoma Combined with Compensated Liver Cirrhosis
- Repeat Resection for Intrahepatic and Omental Recurrence of Ruptured Hepatocelluar Carcinoma after the Initial Surgery
- Complete Remission with Transarterial Chemoembolization in a Patient with Hepatocellular Carcinoma Who Showed Early Recurrence following Surgical Resection