J Neurocrit Care.
2020 Jun;13(1):61-64. 10.18700/jnc.190105.
Nonconvulsive status epilepticus associated with leptomeningeal carcinomatosis and positive SOX1 antibodies
- Affiliations
-
- 1Department of Neurology, Dong-A University Hospital, Busan, Republic of Korea
- KMID: 2503387
- DOI: http://doi.org/10.18700/jnc.190105
Abstract
- Background
Nonconvulsive status epilepticus (NCSE) is a disorder with varying prognoses depending on the underlying etiology. It is increasingly recognized as a cause of altered mental status but is difficult to diagnose without continuous electroencephalogram (EEG) monitoring.
Case Report
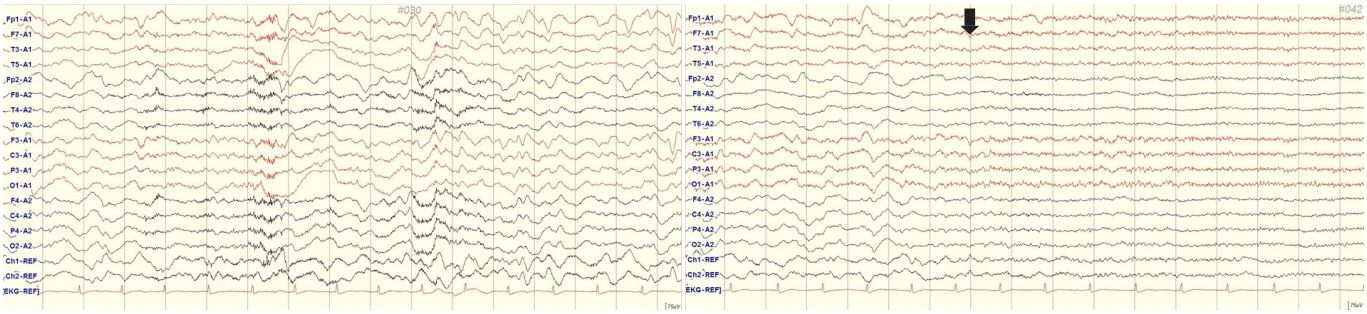
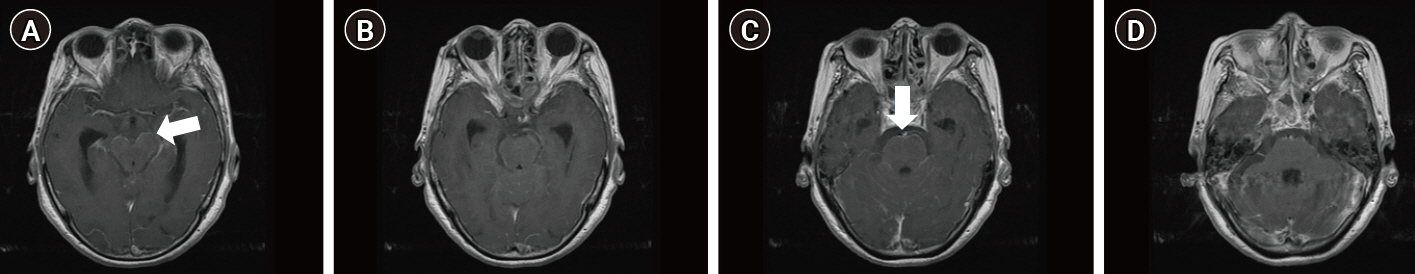
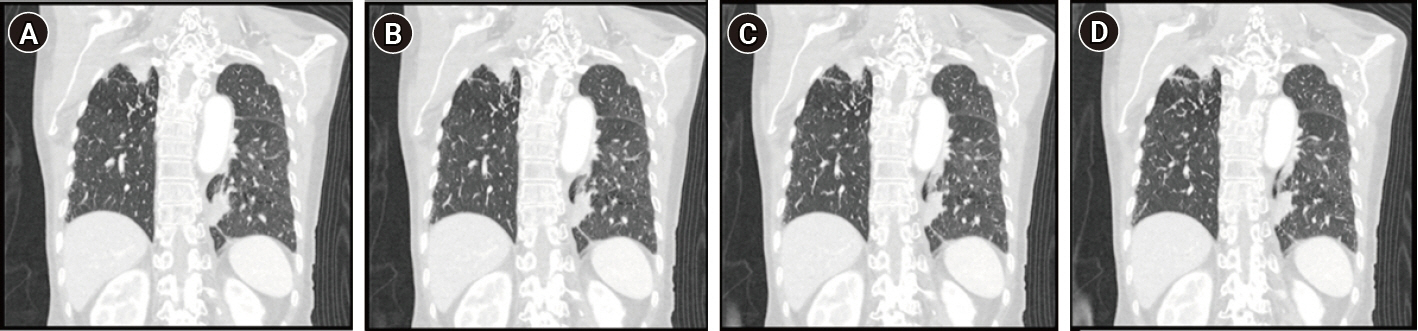
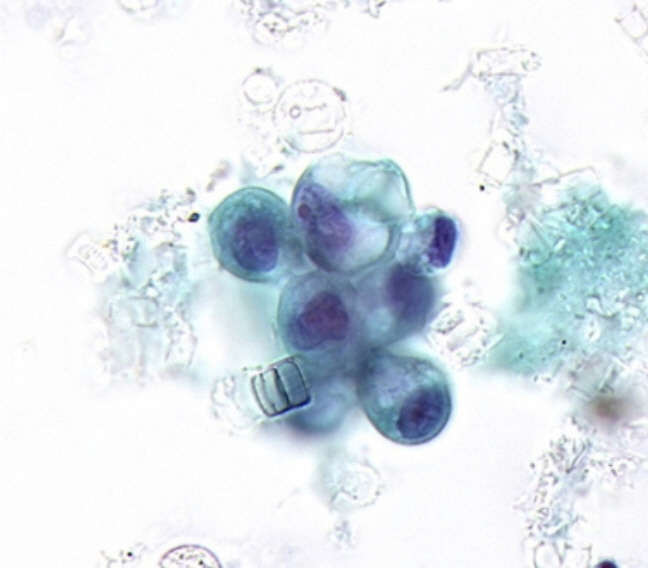
A 75-year-old woman visited our emergency department with acute altered mental status. A cerebrospinal fluid study showed meningeal carcinomatosis. The EEG showed NCSE. Brain magnetic resonance imaging showed diffuse meningeal enhancement around the brain stem. There were no other masses except suspected primary lung cancer on chest computed tomography. However, no malignant cells were detected in a bronchial washing. Levels of carbohydrate antigen 19-9 (CA19-9), CA125, and CA 15-3 were elevated. Autoimmune antibodies were all negative except for SOX1. The patient was unresponsive to first intrathecal chemotherapy and expired two days later.
Conclusion
This is a case report of NCSE caused by paraneoplastic autoimmune encephalitis associated with SOX1 antibodies.
Figure
Reference
-
1. Wasserstrom WR, Glass JP, Posner JB. Diagnosis and treatment of leptomeningeal metastases from solid tumors: experience with 90 patients. Cancer. 1982; 49:759–72.
Article2. Chamberlain MC. Neoplastic meningitis. Curr Neurol Neurosci Rep. 2008; 8:249–58.
Article3. Clarke JL, Perez HR, Jacks LM, Panageas KS, Deangelis LM. Leptomeningeal metastases in the MRI era. Neurology. 2010; 74:1449–54.
Article4. Bayreuther C, Bourg V, Dellamonica J, Borg M, Bernardin G, Thomas P. Complex partial status epilepticus revealing anti-NMDA receptor encephalitis. Epileptic Disord. 2009; 11:261–5.
Article5. Grativvol RS, Cavalcante WCP, Castro LHM, Nitrini R, Simabukuro MM. Updates in the diagnosis and treatment of paraneoplastic neurologic syndromes. Curr Oncol Rep. 2018; 20:92.
Article6. Mantere O, Saarela M, Kieseppä T, Raij T, Mäntylä T, Lindgren M, et al. Anti-neuronal anti-bodies in patients with early psychosis. Schizophr Res. 2018; 192:404–7.
Article7. Stich O, Klages E, Bischler P, Jarius S, Rasiah C, Voltz R, et al. SOX1 antibodies in sera from patients with paraneoplastic neurological syndromes. Acta Neurol Scand. 2012; 125:326–31.
Article8. Lancaster E, Martinez-Hernandez E, Dalmau J. Encephalitis and antibodies to synaptic and neuronal cell surface proteins. Neurology. 2011; 77:179–89.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nonconvulsive Status Epilepticus Associated with Hashimoto's Encephalopathy
- A Case of Complex Partial Status Epilepticus
- Ceftazidime-Induced Nonconvulsive Status Epilepticus
- Isoflurane Anesthesia Therapy for Nonconvulsive Status Epilepticus Continuing after the Control of Convulsive Status Epilepticus: A case report
- Generalized Nonconvulsive Status Epilepticus in Two Patients with End-Stage Renal Disease