J Rhinol.
2020 May;27(1):54-57. 10.18787/jr.2020.00310.
A Child who has Nasal Polyposis Combined with Bronchiectasis
- Affiliations
-
- 1Department of Otolaryngology-Head and Neck Surgery, College of Medicine, Dong-A University, Busan, Korea
- 2Department of Pediatrics, College of Medicine, Dong-A University, Busan, Korea
- KMID: 2502796
- DOI: http://doi.org/10.18787/jr.2020.00310
Abstract
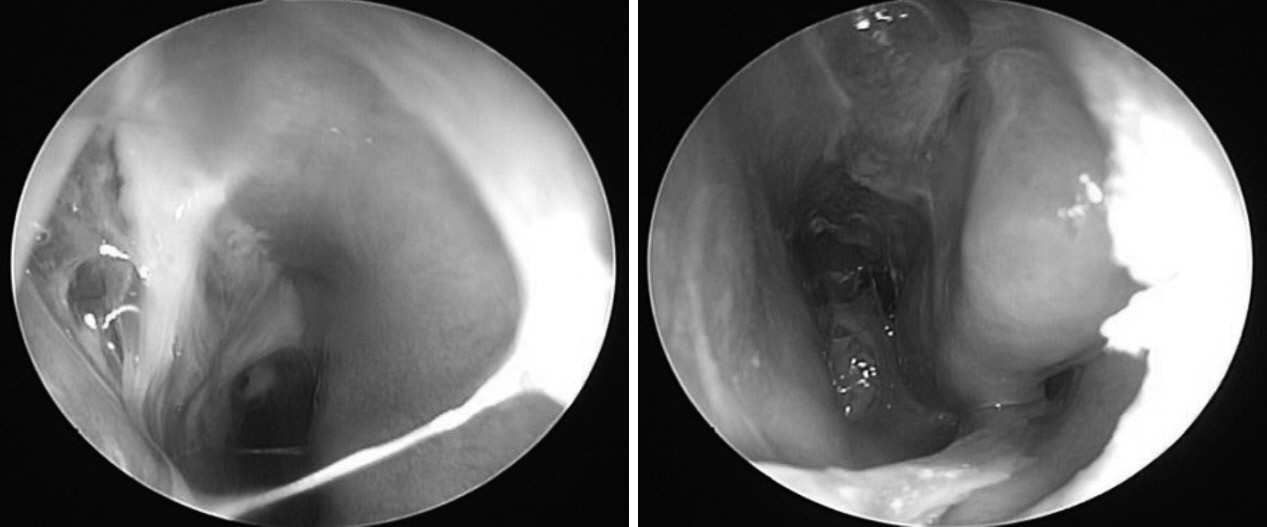
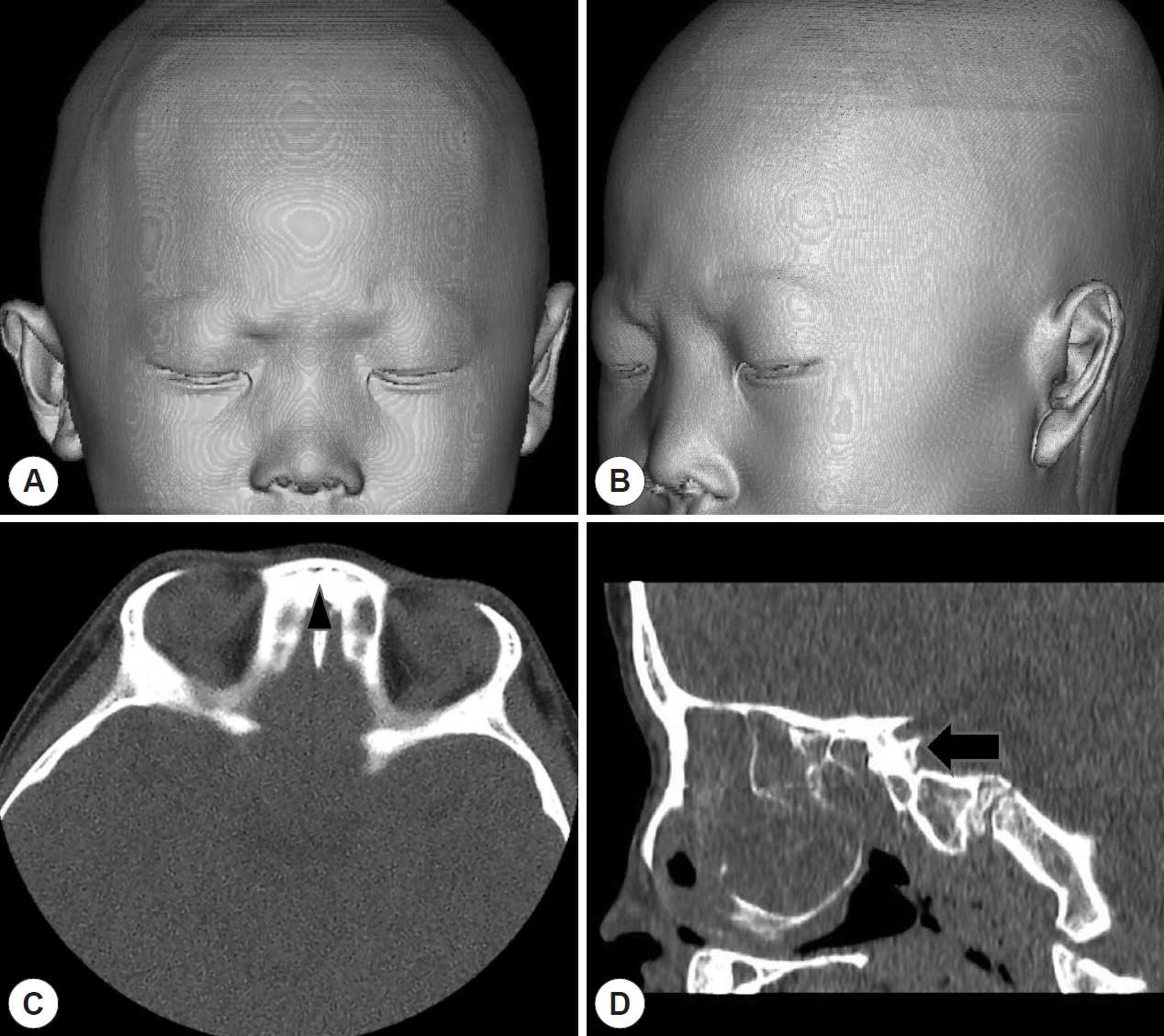
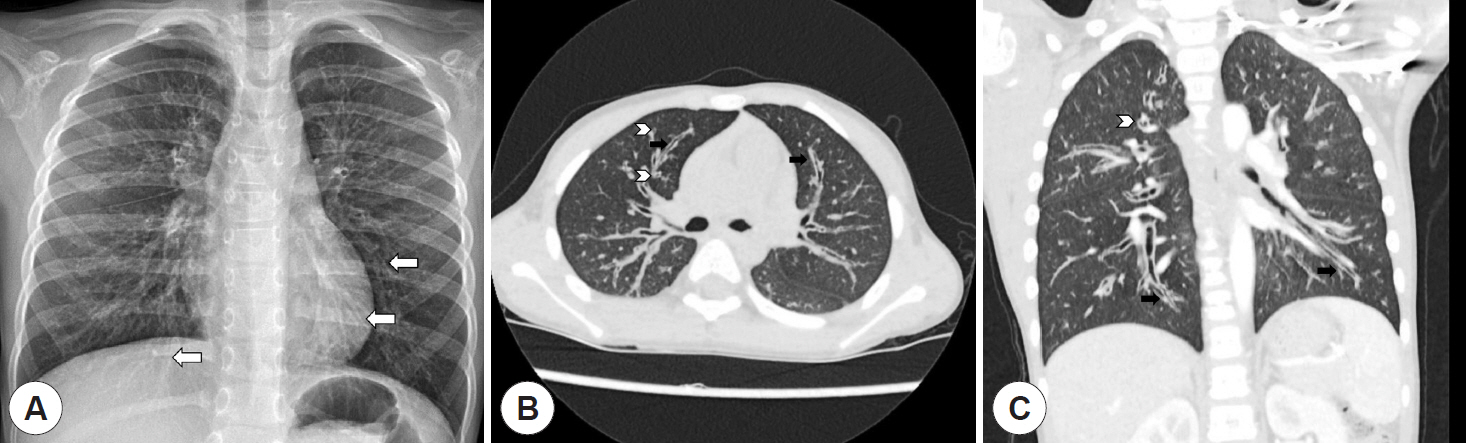
- Nasal polyps are inflammatory lesions of sinonasal tissue that are associated with chronic rhinosinusitis, allergic reaction, and other diseases. Although it is the most common cause of nasal polyps, chronic inflammation of the nasal cavity is not common in children. When nasal polyps are found in childhood, it is important to investigate the cause, such as immunodeficiency disease, cystic fibrosis, primary ciliary dyskinesia, and other syndromes such as Woakes’ syndrome. We report a child who presented with nasal polyps combined with bronchiectasis with a review of related literature.
Keyword
Figure
Reference
-
1. Fokkens WJ, Lund VJ, Mullol J, Bachert C, Alobid I, Baroody F, et al. EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology. 2012; 50(1):1–12.2. Heath J, Hartzell L, Putt C, Kennedy JL. Chronic Rhinosinusitis in Children: Pathophysiology, Evaluation, and Medical Management. Curr Allergy Asthma Rep. 2018; 18(7):37.3. Stevens WW, Schleimer RP, Kern RC. Chronic Rhinosinusitis with Nasal Polyps. J Allergy Clin Immunol Pract. 2016; 4(4):565–72.4. Virgin FW, Rowe SM, Wade MB, Gaggar A, Leon KJ, Young KR, et al. Extensive surgical and comprehensive postoperative medical management of chronic rhinosinusitis. Am J Rhinol Allergy. 2012; 26:70–5.5. Goyal V, Grimwood K, Marchant J, Masters IB, Chang AB. Pediatric bronchiectasis: No longer an orphan disease. Pediatr Pulmonol. 2016; 51(5):450–69.6. Lee E, Shim JY, Kim HY, Suh DI, Choi YJ, Han MY, et al. Clinical characteristics and etiologies of bronchiectasis in Korean children: A multicenter retrospective study. Respir Med. 2019; 150:8–14.7. Chiarella SE, Grammer LC. Immune deficiency in chronic rhinosinusitis: screening and treatment. Expert Rev Clin Immunol. 2017; 13(2):117–23.8. Elborn JS. Cystic fibrosis. Lancet. 2016; 388(10059):2519–31.9. Zariwala MA, Knowles MR, Leigh MW. Primary Ciliary Dyskinesia. Clin Chest Med. 2016; 37(3):449–61.10. Kellerhals B, de Uthemann B. Woakes’ syndrome: the problems of infantile nasal polyps. Int J Pediatr Otorhinolaryngol. 1979; 1(1):79–85.11. Lee CB, Jung NY, Loh YJ, Bae WY. Two Cases of Recurrent Nasal Polyps in Siblings-Woakes’ syndrome. Korean J Otolaryngol. 2019; 62(4):250–4.12. Groman JD, Bolger W, Brass-Ernst L, Macek M Jr, Zeitlin P, Cutting G. Recurrent and destructive nasal polyposis in 2 siblings: a possible case of Woakes’ syndrome. Otolaryngol Head Neck Surg. 2004; 131(6):1009–11.