Clin Endosc.
2020 May;53(3):266-275. 10.5946/ce.2020.095.
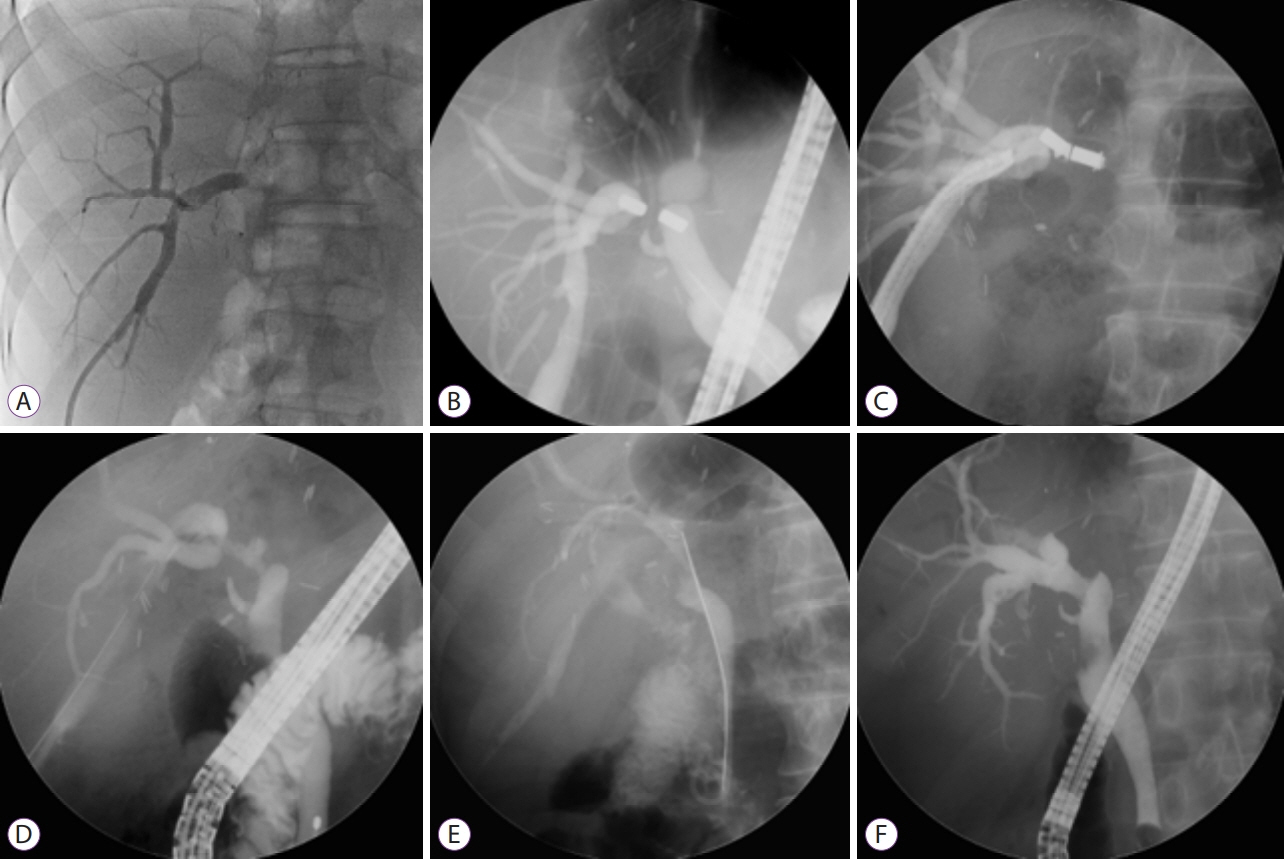
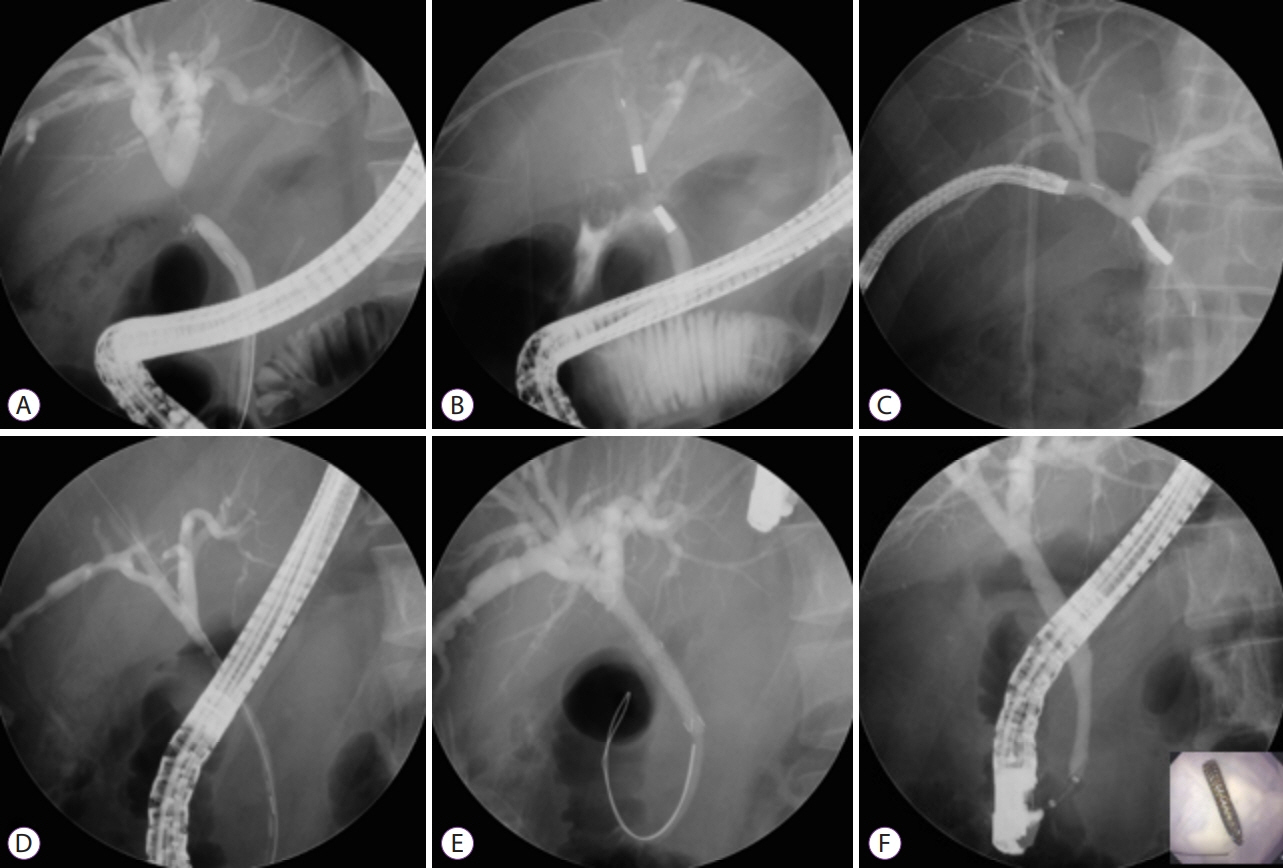
Magnetic Compression Anastomosis for the Treatment of Post-Transplant Biliary Stricture
- Affiliations
-
- 1Department of Internal Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2502761
- DOI: http://doi.org/10.5946/ce.2020.095
Abstract
- A number of different conditions can lead to a bile duct stricture. These strictures are particularly common after biliary operations, including living-donor liver transplantation. Endoscopic and percutaneous methods have high success rates in treating benign biliary strictures. However, these conventional methods are difficult to manage when a guidewire cannot be passed through areas of severe stenosis or complete obstruction. Magnetic compression anastomosis has emerged as an alternative nonsurgical treatment method to avoid the mortality and morbidity risks of reoperation. The feasibility and safety of magnetic compression anastomosis have been reported in several experimental and clinical studies in patients with biliobiliary and bilioenteric strictures. Magnetic compression anastomosis is a minimally traumatic and highly effective procedure, and represents a new paradigm for benign biliary strictures that are difficult to treat with conventional methods.
Figure
Cited by 1 articles
-
Post-cholecystectomy total bile duct strictures: Cases for magnetic compression anastomosis
Freddy Pereira Graterol, Francisco Salazar Marcano, Yajaira Venales Barrios, Yeisson Rivero-Moreno, Dong Ki Lee
Ann Hepatobiliary Pancreat Surg. 2025;29(2):199-204. doi: 10.14701/ahbps.24-186.
Reference
-
1. Martins FP, De Paulo GA, Contini MLC, Ferrari AP. Metal versus plastic stents for anastomotic biliary strictures after liver transplantation: a randomized controlled trial. Gastrointest Endosc. 2018; 87:131. e1-e131.e13.
Article2. Brunet M, Blouin Y, Mosimann F. Biliary strictures after cholecystectomy: long term results of a novative endoscopic treatment. Hepatogastroenterology. 2014; 61:2203–2208.3. Marcos A, Fisher RA, Ham JM, et al. Liver regeneration and function in donor and recipient after right lobe adult to adult living donor liver transplantation. Transplantation. 2000; 69:1375–1379.4. Sanchez-Urdazpal L, Gores GJ, Ward EM, et al. Diagnostic features and clinical outcome of ischemic-type biliary complications after liver transplantation. Hepatology. 1993; 17:605–609.
Article5. Schwartz DA, Petersen BT, Poterucha JJ, Gostout CJ. Endoscopic therapy of anastomotic bile duct strictures occurring after liver transplantation. Gastrointest Endosc. 2000; 51:169–174.
Article6. Yoshimoto T, Yazumi S, Hisatsune H, Egawa H, Maetani Y, Chiba T. Crane-neck deformity after right lobe living donor liver transplantation. Gastrointest Endosc. 2006; 64:271.
Article7. Kim HJ, Park DI, Park JH, et al. Multidetector computed tomography cholangiography with multiplanar reformation for the assessment of patients with biliary obstruction. J Gastroenterol Hepatol. 2007; 22:400–405.
Article8. Pasha SF, Harrison ME, Das A, et al. Endoscopic treatment of anastomotic biliary strictures after deceased donor liver transplantation: outcomes after maximal stent therapy. Gastrointest Endosc. 2007; 66:44–51.
Article9. Shah SA, Grant DR, McGilvray ID, et al. Biliary strictures in 130 consecutive right lobe living donor liver transplant recipients: results of a Western center. Am J Transplant. 2007; 7:161–167.
Article10. Venu M, Brown RD, Lepe R, et al. Laboratory diagnosis and nonoperative management of biliary complications in living donor liver transplant patients. J Clin Gastroenterol. 2007; 41:501–506.
Article11. Avaliani M, Chigogidze N, Nechipai A, Dolgushin B. Magnetic compression biliary-enteric anastomosis for palliation of obstructive jaundice: initial clinical results. J Vasc Interv Radiol. 2009; 20:614–623.
Article12. Graziadei IW, Schwaighofer H, Koch R, et al. Long-term outcome of endoscopic treatment of biliary strictures after liver transplantation. Liver Transpl. 2006; 12:718–725.
Article13. Wang SP, Yan XP, Xue F, et al. Fast magnetic reconstruction of the portal vein with allogeneic blood vessels in canines. Hepatobiliary Pancreat Dis Int. 2015; 14:293–299.
Article14. Matsuno N, Uchiyama M, Nakamura Y, et al. A nonsuture anastomosis using magnetic compression for biliary stricture after living donor liver transplantation. Hepatogastroenterology. 2009; 56:47–49.15. Yamanouchi E. A new interventional method: magnetic compression anastomosis with rare-earth magnets. Cardiovasc Intervent Radiol. 1998; 21(Suppl 1):S155.16. Yamanouchi E, Kumano R, Kobayashi K, et al. [Treatment for bowel or biliary obstruction by magnetic compression anastomosis development of Yamanouchi’s method and its clinical evaluation]. J Nippon Med Sch. 2002; 69:471–475.
Article17. Mimuro A, Tsuchida A, Yamanouchi E, et al. A novel technique of magnetic compression anastomosis for severe biliary stenosis. Gastrointest Endosc. 2003; 58:283–287.
Article18. Itoi T, Yamanouchi E, Ikeda T, et al. Magnetic compression anastomosis: a novel technique for canalization of severe hilar bile duct strictures. Endoscopy. 2005; 37:1248–1251.
Article19. Muraoka N, Uematsu H, Yamanouchi E, et al. Yamanouchi magnetic compression anastomosis for bilioenteric anastomotic stricture after living-donor liver transplantation. J Vasc Interv Radiol. 2005; 16:1263–1267.
Article20. Yukawa N, Rino Y, Yamanouchi E, et al. [A case of magnetic compression anastomosis between the common bile duct and the duodenum after distal gastrectomy with Roux-Y reconstruction and cholecystectomy]. Nihon Shokakibyo Gakkai Zasshi. 2008; 105:1523–1528.21. Takao S, Matsuo Y, Shinchi H, et al. Magnetic compression anastomosis for benign obstruction of the common bile duct. Endoscopy. 2001; 33:988–990.
Article22. Jang SI, Kim JH, Won JY, et al. Magnetic compression anastomosis is useful in biliary anastomotic strictures after living donor liver transplantation. Gastrointest Endosc. 2011; 74:1040–1048.
Article23. Jang SI, Rhee K, Kim H, et al. Recanalization of refractory benign biliary stricture using magnetic compression anastomosis. Endoscopy. 2014; 46:70–74.
Article24. Jang SI, Lee KH, Yoon HJ, Lee DK. Treatment of completely obstructed benign biliary strictures with magnetic compression anastomosis: follow-up results after recanalization. Gastrointest Endosc. 2017; 85:1057–1066.
Article25. Dumonceau JM, Devière J, Delhaye M, Baize M, Cremer M. Plastic and metal stents for postoperative benign bile duct strictures: the best and the worst. Gastrointest Endosc. 1998; 47:8–17.
Article26. Bonnel DH, Liguory CL, Lefebvre JF, Cornud FE. Placement of metallic stents for treatment of postoperative biliary strictures: long-term outcome in 25 patients. AJR Am J Roentgenol. 1997; 169:1517–1522.
Article27. Ernst O, Sergent G, Mizrahi D, Delemazure O, L’Herminé C. Biliary leaks: treatment by means of percutaneous transhepatic biliary drainage. Radiology. 1999; 211:345–348.
Article28. Vogel SB, Howard RJ, Caridi J, Hawkins IF Jr. Evaluation of percutaneous transhepatic balloon dilatation of benign biliary strictures in highrisk patients. Am J Surg. 1985; 149:73–79.
Article29. Mita A, Hashikura Y, Masuda Y, et al. Nonsurgical policy for treatment of bilioenteric anastomotic stricture after living donor liver transplantation. Transpl Int. 2008; 21:320–327.
Article30. Okajima H, Kotera A, Takeichi T, et al. Magnet compression anastomosis for bile duct stenosis after duct-to-duct biliary reconstruction in living donor liver transplantation. Liver Transpl. 2005; 11:473–475.
Article31. Oya H, Sato Y, Yamanouchi E, et al. Magnetic compression anastomosis for bile duct stenosis after donor left hepatectomy: a case report. Transplant Proc. 2012; 44:806–809.
Article32. Suyama K, Takamori H, Yamanouchi E, et al. Recanalization of obstructed choledochojejunostomy using the magnet compression anastomosis technique. Am J Gastroenterol. 2010; 105:230–231.
Article33. Itoi T, Yamanouchi E, Ikeuchi N, Kasuya K, Iwamoto H, Tsuchida A. Magnetic compression duct-to-duct anastomosis for biliary obstruction in a patient with living donor liver transplantation. Gut Liver. 2010; 4(Suppl 1):S96–S98.
Article34. Jang SI, Choi J, Lee DK. Magnetic compression anastomosis for treatment of benign biliary stricture. Dig Endosc. 2015; 27:239–249.
Article35. Jang SI, Lee KH, Joo SM, Park H, Choi JH, Lee DK. Maintenance of the fistulous tract after recanalization via magnetic compression anastomosis in completely obstructed benign biliary stricture. Scand J Gastroenterol. 2018; 53:1393–1398.
Article36. Kao D, Zepeda-Gomez S, Tandon P, Bain VG. Managing the post-liver transplantation anastomotic biliary stricture: multiple plastic versus metal stents: a systematic review. Gastrointest Endosc. 2013; 77:679–691.
Article37. Thuluvath PJ, Pfau PR, Kimmey MB, Ginsberg GG. Biliary complications after liver transplantation: the role of endoscopy. Endoscopy. 2005; 37:857–863.
Article38. Zoepf T, Maldonado-Lopez EJ, Hilgard P, et al. Balloon dilatation vs. balloon dilatation plus bile duct endoprostheses for treatment of anastomotic biliary strictures after liver transplantation. Liver Transpl. 2006; 12:88–94.
Article39. Sharma S, Gurakar A, Jabbour N. Biliary strictures following liver transplantation: past, present and preventive strategies. Liver Transpl. 2008; 14:759–769.
Article40. Tal AO, Finkelmeier F, Filmann N, et al. Multiple plastic stents versus covered metal stent for treatment of anastomotic biliary strictures after liver transplantation: a prospective, randomized, multicenter trial. Gastrointest Endosc. 2017; 86:1038–1045.41. Akita H, Hikita H, Yamanouchi E, et al. Use of a metallic-wall stent in the magnet compression anastomosis technique for bile duct obstruction after liver transplantation. Liver Transpl. 2008; 14:118–120.
Article42. Ersoz G, Tekin F, Bozkaya H, et al. Magnetic compression anastomosis for patients with a disconnected bile duct after living-donor related liver transplantation: a pilot study. Endoscopy. 2016; 48:652–656.
Article43. Parlak E, Koksal AS, Kucukay F, Eminler AT, Toka B, Uslan MI. A novel technique for the endoscopic treatment of complete biliary anastomosis obstructions after liver transplantation: through-the-scope magnetic compression anastomosis. Gastrointest Endosc. 2017; 85:841–847.
Article44. Jiang XM, Yamamoto K, Tsuchiya T, et al. Magnetic compression anastomosis for biliary obstruction after partial hepatectomy. Endoscopy. 2018; 50:E144–E145.
Article45. Li Y, Sun H, Yan X, et al. Magnetic compression anastomosis for the treatment of benign biliary strictures: a clinical study from China. Surg Endosc. 2020; 34:2541–2550.
Article46. Weber A, Zellner S, Wagenpfeil S, et al. Long-term follow-up after endoscopic stent therapy for benign biliary strictures. J Clin Gastroenterol. 2014; 48:88–93.
Article47. Dumonceau JM, Tringali A, Blero D, et al. Biliary stenting: indications, choice of stents and results: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy. 2012; 44:277–298.
Article48. Schumacher B, Othman T, Jansen M, Preiss C, Neuhaus H. Long-term follow-up of percutaneous transhepatic therapy (PTT) in patients with definite benign anastomotic strictures after hepaticojejunostomy. Endoscopy. 2001; 33:409–415.
Article49. Weber A, Rosca B, Neu B, et al. Long-term follow-up of percutaneous transhepatic biliary drainage (PTBD) in patients with benign bilioenterostomy stricture. Endoscopy. 2009; 41:323–328.
Article50. Bonnel DH, Fingerhut AL. Percutaneous transhepatic balloon dilatation of benign bilioenteric strictures: long-term results in 110 patients. Am J Surg. 2012; 203:675–683.
Article51. Costamagna G, Boškoski I. Current treatment of benign biliary strictures. Ann Gastroenterol. 2013; 26:37–40.52. Kato H, Kawamoto H, Tsutsumi K, et al. Long-term outcomes of endoscopic management for biliary strictures after living donor liver transplantation with duct-to-duct reconstruction. Transpl Int. 2009; 22:914–921.
Article53. Chang JH, Lee IS, Choi JY, et al. Biliary stricture after adult right-lobe living-donor liver transplantation with duct-to-duct anastomosis: longterm outcome and its related factors after endoscopic treatment. Gut Liver. 2010; 4:226–233.
Article54. Elwir S, Thompson J, Amateau SK, et al. Endoscopic management of biliary leaks and strictures after living donor liver transplantation: optimizing techniques for successful management. Dig Dis Sci. 2017; 62:244–252.
Article55. Melcher ML, Pomposelli JJ, Verbesey JE, et al. Comparison of biliary complications in adult living-donor liver transplants performed at two busy transplant centers. Clin Transplant. 2010; 24:E137–E144.
Article56. Rao J, Sun Y, Zhou H, et al. Remain recipient partial liver during liver transplant after Hassab. J Surg Res. 2014; 189:321–325.
Article57. Gondolesi GE, Varotti G, Florman SS, et al. Biliary complications in 96 consecutive right lobe living donor transplant recipients. Transplantation. 2004; 77:1842–1848.
Article58. Kasahara M, Egawa H, Takada Y, et al. Biliary reconstruction in right lobe living-donor liver transplantation: comparison of different techniques in 321 recipients. Ann Surg. 2006; 243:559–566.59. Tsujino T, Isayama H, Sugawara Y, et al. Endoscopic management of biliary complications after adult living donor liver transplantation. Am J Gastroenterol. 2006; 101:2230–2236.
Article60. Yazumi S, Yoshimoto T, Hisatsune H, et al. Endoscopic treatment of biliary complications after right-lobe living-donor liver transplantation with duct-to-duct biliary anastomosis. J Hepatobiliary Pancreat Surg. 2006; 13:502–510.
Article61. Tashiro H, Itamoto T, Sasaki T, et al. Biliary complications after duct-toduct biliary reconstruction in living-donor liver transplantation: causes and treatment. World J Surg. 2007; 31:2222–2229.
Article62. Londoño MC, Balderramo D, Cárdenas A. Management of biliary complications after orthotopic liver transplantation: the role of endoscopy. World J Gastroenterol. 2008; 14:493–497.
Article63. Ohkubo M, Nagino M, Kamiya J, et al. Surgical anatomy of the bile ducts at the hepatic hilum as applied to living donor liver transplantation. Ann Surg. 2004; 239:82–86.
Article64. Archer SB, Brown DW, Smith CD, Branum GD, Hunter JG. Bile duct injury during laparoscopic cholecystectomy: results of a national survey. Ann Surg. 2001; 234:549–558. discussion 558-559.65. Bismuth H, Majno PE. Biliary strictures: classification based on the principles of surgical treatment. World J Surg. 2001; 25:1241–1244.
Article66. Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995; 180:101–125.67. Way LW, Stewart L, Gantert W, et al. Causes and prevention of laparoscopic bile duct injuries: analysis of 252 cases from a human factors and cognitive psychology perspective. Ann Surg. 2003; 237:460–469.68. Fiocca F, Salvatori FM, Fanelli F, et al. Complete transection of the main bile duct: minimally invasive treatment with an endoscopic-radiologic rendezvous. Gastrointest Endosc. 2011; 74:1393–1398.
Article69. Devière J. Benign biliary strictures and leaks. Gastrointest Endosc Clin N Am. 2015; 25:713–723.
Article70. Liu XM, Li Y, Xiang JX, et al. Magnetic compression anastomosis for biliojejunostomy and pancreaticojejunostomy in Whipple’s procedure: an initial clinical study. J Gastroenterol Hepatol. 2019; 34:589–594.
Article71. Itoi T, Kasuya K, Sofuni A, et al. Magnetic compression anastomosis for biliary obstruction: review and experience at Tokyo Medical University Hospital. J Hepatobiliary Pancreat Sci. 2011; 18:357–365.
Article72. Lim HC, Lee DK, Choi HK, et al. [Magnet compression anastomosis for bilioenteric anastomotic stricture after removal of a choledochal cyst: a case report]. Korean J Gastrointest Endosc. 2010; 41:180–184.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Magnetic compression anastomosis for treatment of post-transplant biliary stricture: A case report with dual-graft living donor liver transplantation
- Post-cholecystectomy total bile duct strictures: Cases for magnetic compression anastomosis
- A case with combined postoperative bile leakage and anastomotic stricture after liver transplantation treated with magnet compression anastomosis
- Magnetic Compression Duct-to-duct Anastomosis for Biliary Obstruction in a Patient with Living Donor Liver Transplantation
- Unilateral Versus Bilateral Biliary Drainage for Post-Transplant Anastomotic Stricture