Korean J Orthod.
2020 May;50(3):188-196. 10.4041/kjod.2020.50.3.188.
Periodontal ligament proliferation and expressions of bone biomolecules upon orthodontic preloading: Clinical implications for tooth autotransplantation
- Affiliations
-
- 1Department of Orthodontics, Faculty of Dentistry, Bangkokthonburi University, Bangkok, Thailand
- 2Department of Oral Biology and Diagnostic Sciences, Center of Excellence in Oral and Maxillofacial Biology, Faculty of Dentistry, Chiang Mai University, Chiang Mai, Thailand
- 3Center of Excellence in Oral and Maxillofacial Biology, Faculty of Dentistry, Chiang Mai University, Chiang Mai, Thailand
- KMID: 2502628
- DOI: http://doi.org/10.4041/kjod.2020.50.3.188
Abstract
Objective
Preservation of the periodontal ligament (PDL) is vital to the success of tooth autotransplantation (TAT). Increased PDL volumes and facilitated tooth extraction have been observed upon orthodontic preloading. However, it is unclear whether any changes occur in the expressions of bone biomolecules in the increased PDL volumes. This study aimed to determine the expressions of runt-related transcription factor 2 (RUNX2), alkaline phosphatase (ALP), receptor activator of nuclear factor kappa-B ligand (RANKL), and osteoprotegerin (OPG) in PDL upon preloading.
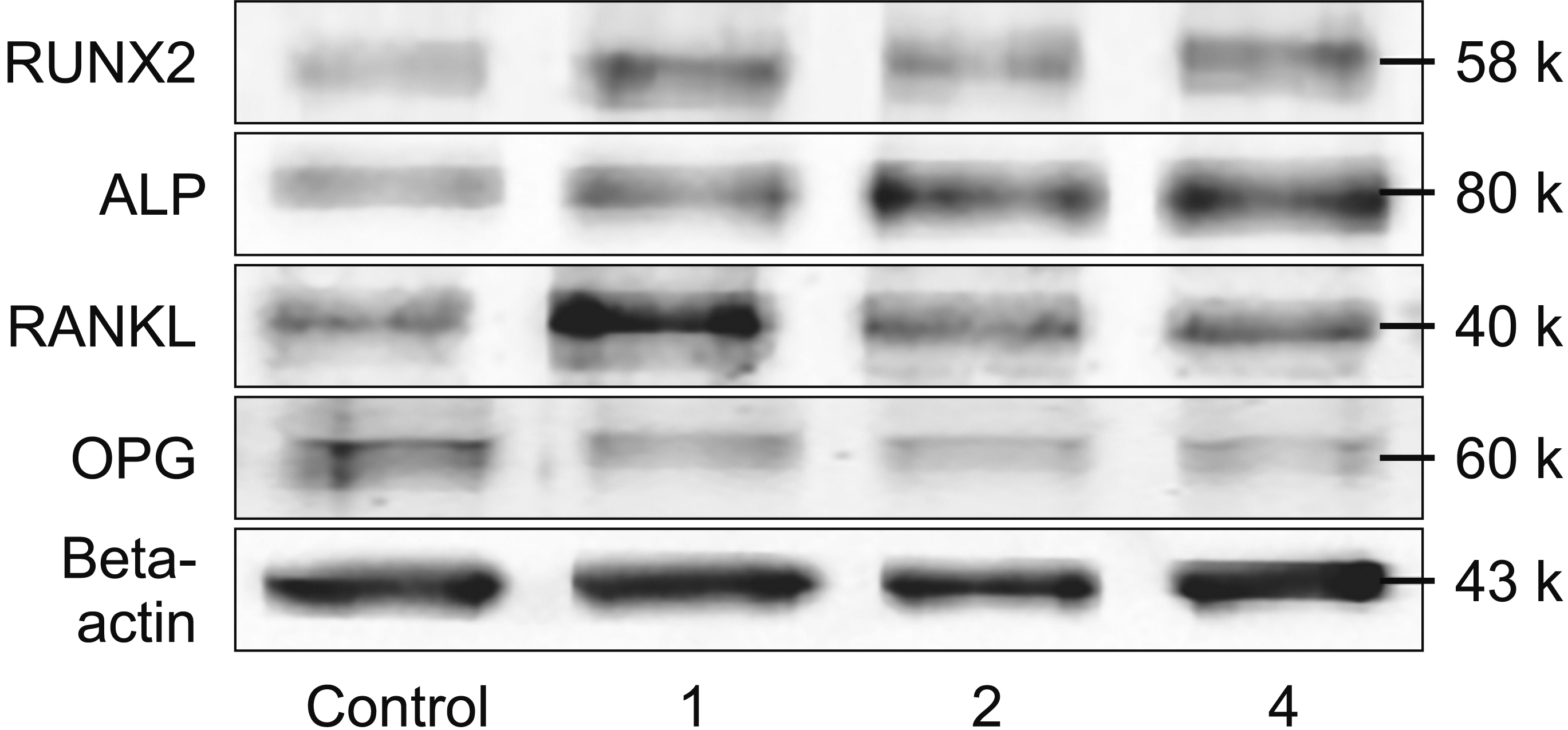
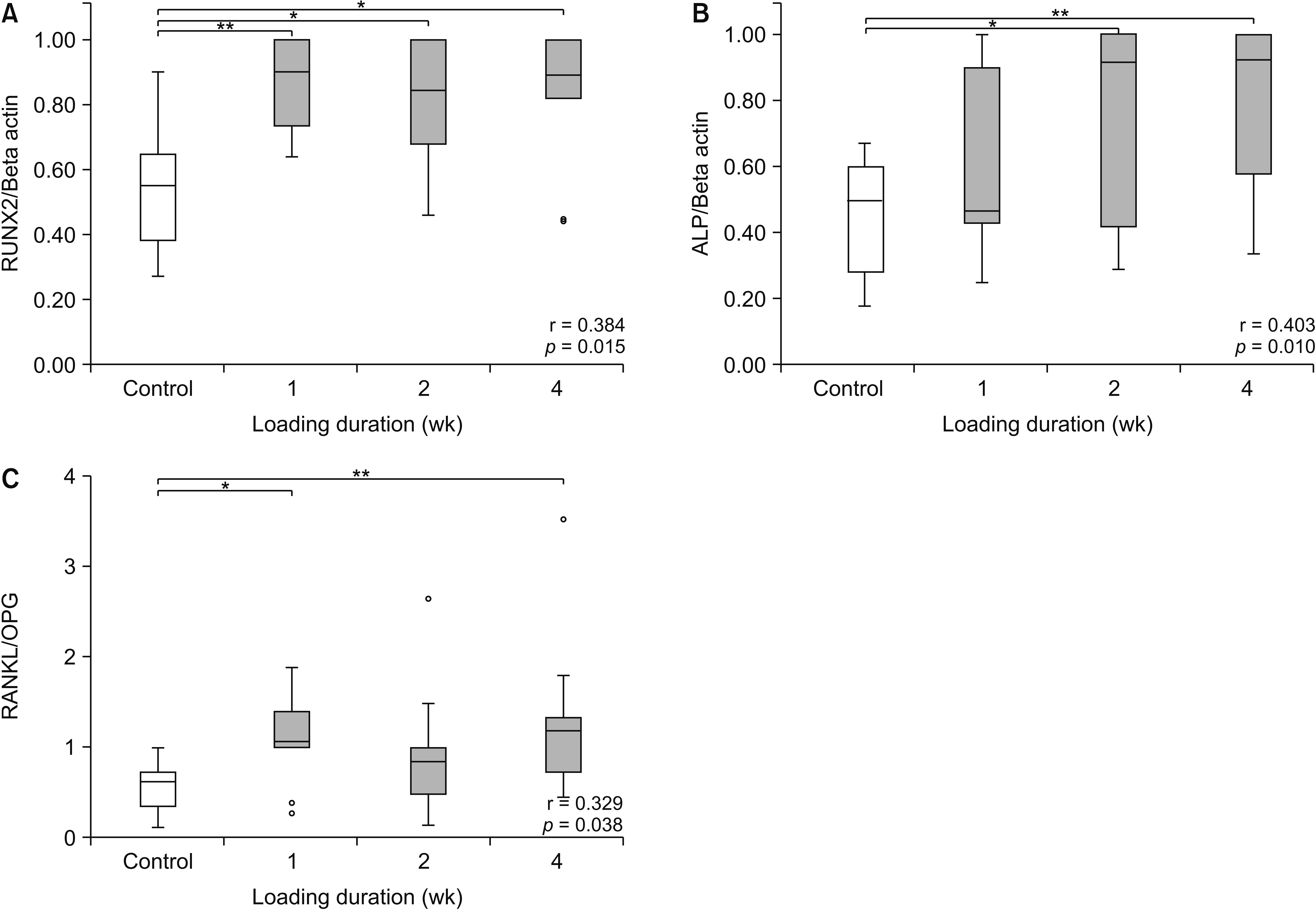
Methods
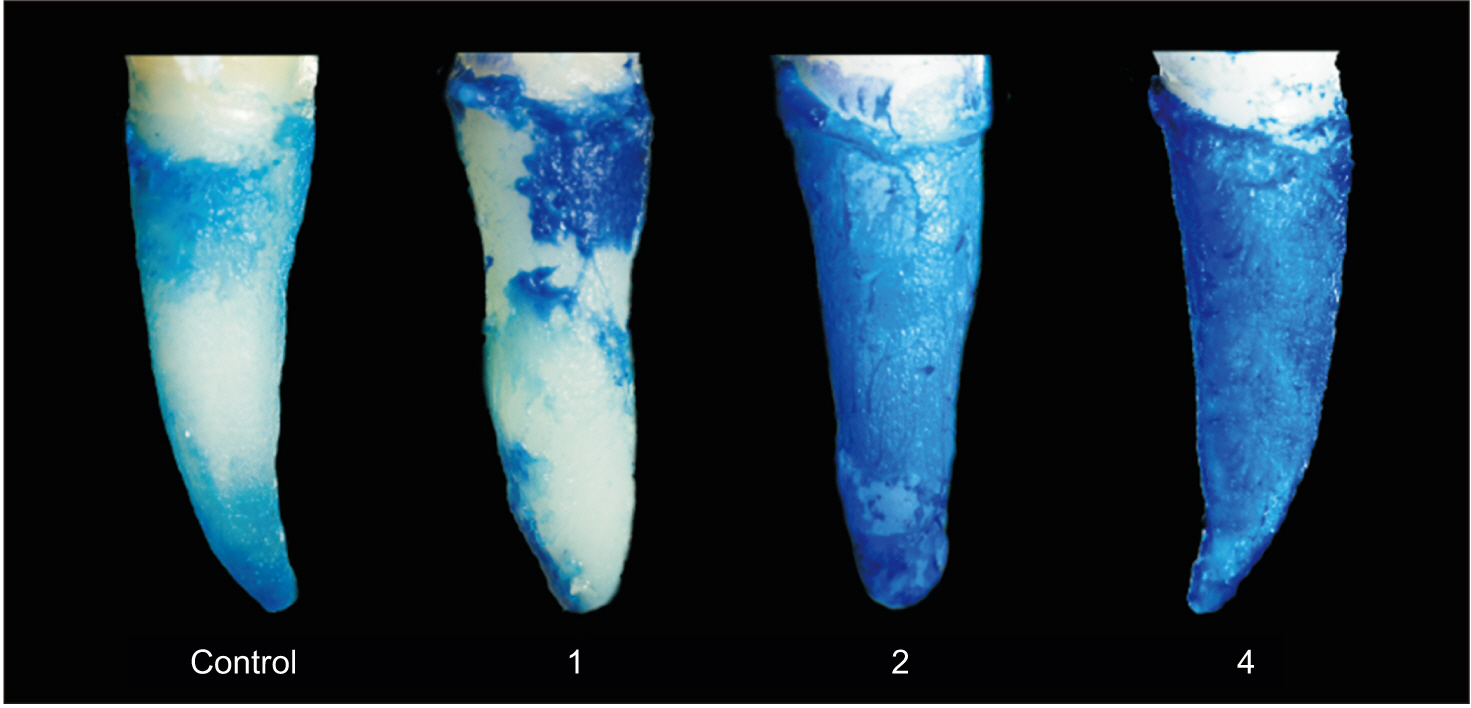
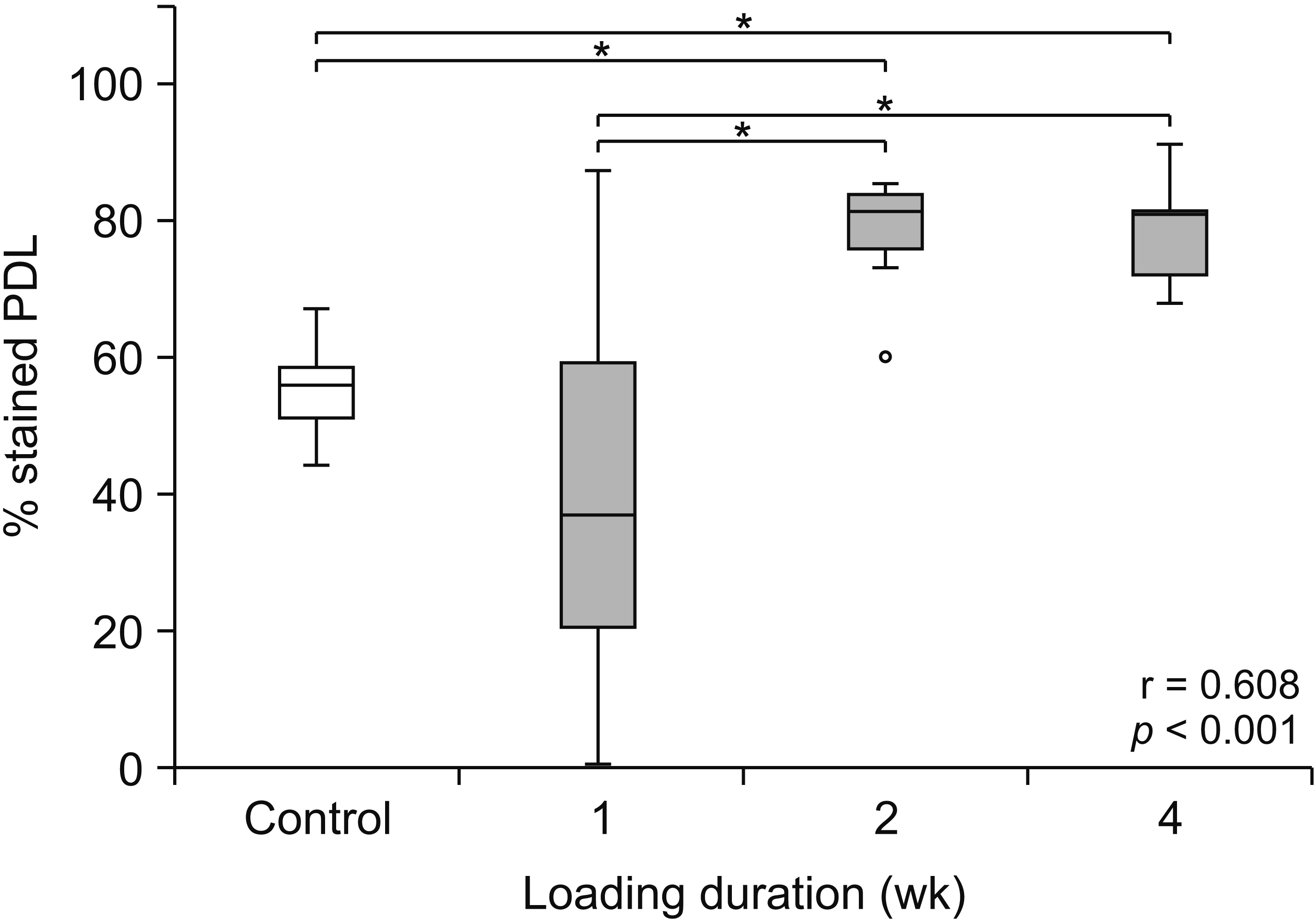
Seventy-two premolars from 18 patients were randomly assigned to experimental groups that received a leveling force for 1, 2, or 4 weeks or to a control unloaded group. Following extraction, PDL volumes from 32 premolars of eight patients (21.0 ± 3.8 years) were evaluated using toluidine blue staining. The expressions of the biomolecules in the PDL from 40 premolars of ten patients (21.4 ± 4.0 years) were analyzed via immunoblotting.
Results
The median percentage of stained PDL was significantly higher at 2 and 4 weeks after preloading than in the unloaded condition (p < 0.05). The median RUNX2 and ALP expression levels were significantly higher at 2 and 4 weeks after preloading than in the unloaded condition (p < 0.05), whereas the median RANKL/OPG ratios were significantly higher at 1 and 4 weeks after preloading (p < 0.05).
Conclusions
Orthodontic preloading for 4 weeks enhances PDL volumes as well as the expressions of RUNX2, ALP and the RANKL/OPG ratio in the PDL, suggesting this loading period is suitable for successful TAT.
Figure
Reference
-
1. Andreasen JO. 1981; Periodontal healing after replantation and autotransplantation of incisors in monkeys. Int J Oral Surg. 10:54–61. DOI: 10.1016/S0300-9785(81)80008-7. PMID: 6792095.
Article2. Tsukiboshi M, Andreasen JO. 2001. Autotransplantation of teeth. Quintessence Pub Co;Chicago:3. Sugai T, Yoshizawa M, Kobayashi T, Ono K, Takagi R, Kitamura N, et al. 2010; Clinical study on prognostic factors for autotransplantation of teeth with complete root formation. Int J Oral Maxillofac Surg. 39:1193–203. DOI: 10.1016/j.ijom.2010.06.018. PMID: 20630706.
Article4. Li M, Zhang C, Yang Y. 2019; Effects of mechanical forces on osteogenesis and osteoclastogenesis in human periodontal ligament fibroblasts: a systematic review of in vitro studies. Bone Joint Res. 8:19–31. DOI: 10.1302/2046-3758.81.BJR-2018-0060.R1. PMID: 30800296. PMCID: PMC6359886.5. Brooks PJ, Nilforoushan D, Manolson MF, Simmons CA, Gong SG. 2009; Molecular markers of early orthodontic tooth movement. Angle Orthod. 79:1108–13. DOI: 10.2319/121508-638R.1. PMID: 19852601.
Article6. Li B, Zhang YH, Wang LX, Li X, Zhang XD. 2015; Expression of OPG, RANKL, and RUNX2 in rabbit periodontium under orthodontic force. Genet Mol Res. 14:19382–8. DOI: 10.4238/2015.December.29.48. PMID: 26782591.
Article7. Garlet TP, Coelho U, Silva JS, Garlet GP. 2007; Cytokine expression pattern in compression and tension sides of the periodontal ligament during orthodontic tooth movement in humans. Eur J Oral Sci. 115:355–62. DOI: 10.1111/j.1600-0722.2007.00469.x. PMID: 17850423.
Article8. Nishijima Y, Yamaguchi M, Kojima T, Aihara N, Nakajima R, Kasai K. 2006; Levels of RANKL and OPG in gingival crevicular fluid during orthodontic tooth movement and effect of compression force on releases from periodontal ligament cells in vitro. Orthod Craniofac Res. 9:63–70. DOI: 10.1111/j.1601-6343.2006.00340.x. PMID: 16764680.
Article9. Zhang L, Liu W, Zhao J, Ma X, Shen L, Zhang Y, et al. 2016; Mechanical stress regulates osteogenic differentiation and RANKL/OPG ratio in periodontal ligament stem cells by the Wnt/β-catenin pathway. Biochim Biophys Acta. 1860:2211–9. DOI: 10.1016/j.bbagen.2016.05.003. PMID: 27154288.
Article10. Tripuwabhrut P, Mustafa M, Gjerde CG, Brudvik P, Mustafa K. 2013; Effect of compressive force on human osteoblast-like cells and bone remodelling: an in vitro study. Arch Oral Biol. 58:826–36. DOI: 10.1016/j.archoralbio.2013.01.004. PMID: 23583016.
Article11. Pavlin D, Dove SB, Zadro R, Gluhak-Heinrich J. 2000; Mechanical loading stimulates differentiation of periodontal osteoblasts in a mouse osteoinduction model: effect on type I collagen and alkaline phosphatase genes. Calcif Tissue Int. 67:163–72. DOI: 10.1007/s00223001105. PMID: 10920222.
Article12. Banerjee C, McCabe LR, Choi JY, Hiebert SW, Stein JL, Stein GS, et al. 1997; Runt homology domain proteins in osteoblast differentiation: AML3/CBFA1 is a major component of a bone-specific complex. J Cell Biochem. 66:1–8. DOI: 10.1002/(SICI)1097-4644(19970701)66:1<1::AID-JCB1>3.0.CO;2-V. PMID: 9215522.
Article13. Yamaguchi M. 2009; RANK/RANKL/OPG during orthodontic tooth movement. Orthod Craniofac Res. 12:113–9. DOI: 10.1111/j.1601-6343.2009.01444.x. PMID: 19419454.
Article14. Kapasa ER, Giannoudis PV, Jia X, Hatton PV, Yang XB. 2017; The effect of RANKL/OPG balance on reducing implant complications. J Funct Biomater. 8:E42. DOI: 10.3390/jfb8040042. PMID: 28937598. PMCID: PMC5748549.
Article15. Suzaki Y, Matsumoto Y, Kanno Z, Soma K. 2008; Preapplication of orthodontic forces to the donor teeth affects periodontal healing of transplanted teeth. Angle Orthod. 78:495–501. DOI: 10.2319/020207-51.1. PMID: 18416609.
Article16. Choi YH, Bae JH, Kim YK, Kim HY, Kim SK, Cho BH. 2014; Clinical outcome of intentional replantation with preoperative orthodontic extrusion: a retrospective study. Int Endod J. 47:1168–76. DOI: 10.1111/iej.12268. PMID: 24527674.
Article17. Suzuki EY, Suzuki B. 2019; Guiding template for direct bracket placement: a hybrid technique. Austin J Dent. 6:1127.18. Miura F, Mogi M, Ohura Y, Hamanaka H. 1986; The super-elastic property of the Japanese NiTi alloy wire for use in orthodontics. Am J Orthod Dentofacial Orthop. 90:1–10. DOI: 10.1016/0889-5406(86)90021-1. PMID: 3460342.
Article19. Nakdilok K, Langsa-ard S, Krisanaprakornkit S, Suzuki EY, Suzuki B. 2020; Enhancement of human periodontal ligament by preapplication of orthodontic loading. Am J Orthod Dentofacial Orthop. 157:186–93. DOI: 10.1016/j.ajodo.2019.03.019. PMID: 32005470.
Article20. Thilander B. Graber LW, Vanarsdall RL, Vig KWL, editors. 2011. Tissue reactions in orthodontics. Orthodontics: current principles and techniques. 5th ed. Elsevier/Mosby;Philadelphia: p. 247–86.21. VigTen Cate AR, Deporter DA, Freeman E. 1976; The role of fibroblasts in the remodeling of periodontal ligament during physiologic tooth movement. Am J Orthod. 69:155–68. DOI: 10.1016/0002-9416(76)90194-9. PMID: 1061506.22. Shen T, Qiu L, Chang H, Yang Y, Jian C, Xiong J, et al. 2014; Cyclic tension promotes osteogenic differentiation in human periodontal ligament stem cells. Int J Clin Exp Pathol. 7:7872–80. PMID: 25550827. PMCID: PMC4270604.23. Kanzaki H, Chiba M, Shimizu Y, Mitani H. 2002; Periodontal ligament cells under mechanical stress induce osteoclastogenesis by receptor activator of nuclear factor kappaB ligand up-regulation via prostaglandin E2 synthesis. J Bone Miner Res. 17:210–20. DOI: 10.1359/jbmr.2002.17.2.210. PMID: 11811551.24. Dunn MD, Park CH, Kostenuik PJ, Kapila S, Giannobile WV. 2007; Local delivery of osteoprotegerin inhibits mechanically mediated bone modeling in orthodontic tooth movement. Bone. 41:446–55. DOI: 10.1016/j.bone.2007.04.194. PMID: 17588510. PMCID: PMC2581749.
Article25. Krishnan V, Davidovitch Z. 2006; Cellular, molecular, and tissue-level reactions to orthodontic force. Am J Orthod Dentofacial Orthop. 129:469.e1–32. DOI: 10.1016/j.ajodo.2005.10.007. PMID: 16627171.
Article26. Bumann A, Carvalho RS, Schwarzer CL, Yen EH. 1997; Collagen synthesis from human PDL cells following orthodontic tooth movement. Eur J Orthod. 19:29–37. DOI: 10.1093/ejo/19.1.29. PMID: 9071043.
Article27. Pilon JJ, Kuijpers-Jagtman AM, Maltha JC. 1996; Magnitude of orthodontic forces and rate of bodily tooth movement. An experimental study. Am J Orthod Dentofacial Orthop. 110:16–23. DOI: 10.1016/S0889-5406(96)70082-3. PMID: 8686673.
Article28. Han J, Xu X, Zhang B, Chen B, Hang W. 2015; Expression of ATF4 and RUNX2 in periodontal tissue of pressure side during orthodontic tooth movement in rat. Int J Clin Exp Med. 8:934–8. PMID: 25785078. PMCID: PMC4358533.29. Insoft M, King GJ, Keeling SD. 1996; The measurement of acid and alkaline phosphatase in gingival crevicular fluid during orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 109:287–96. DOI: 10.1016/S0889-5406(96)70152-X. PMID: 8607474.
Article30. Flórez-Moreno GA, Isaza-Guzmán DM, Tobón-Arroyave SI. 2013; Time-related changes in salivary levels of the osteotropic factors sRANKL and OPG through orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 143:92–100. DOI: 10.1016/j.ajodo.2012.08.026. PMID: 23273364.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Autotransplantation of the missing tooth: the report of cases
- The study on the periodontal vascular changes of rat incisors following experimental tooth movement
- Effects of nitric oxide on the proliferation and differentiation of human periodontal ligament cells
- Cases report of autotransplantation of immature teeth
- The autotransplantation of an anklyosed maxillary canine