Korean J Sports Med.
2020 Mar;38(1):12-19. 10.5763/kjsm.2020.38.1.12.
The Time of Return to Play after Surgery for Chronic Lateral Ankle Instability in Athletes: A Systematic Review
- Affiliations
-
- 1Sejong Sports Medicine and Performance Center, Seoul, Korea
- 2CM Hospital of National Training Center of Korean Sport & Olympic Committee, Jincheon, Korea
- 3Seoul CM Hospital, Seoul, Korea
- KMID: 2502512
- DOI: http://doi.org/10.5763/kjsm.2020.38.1.12
Abstract
- Purpose
The study aimed to assess the average time to return to play following surgery for chronic lateral ankle instability in athletes.
Methods
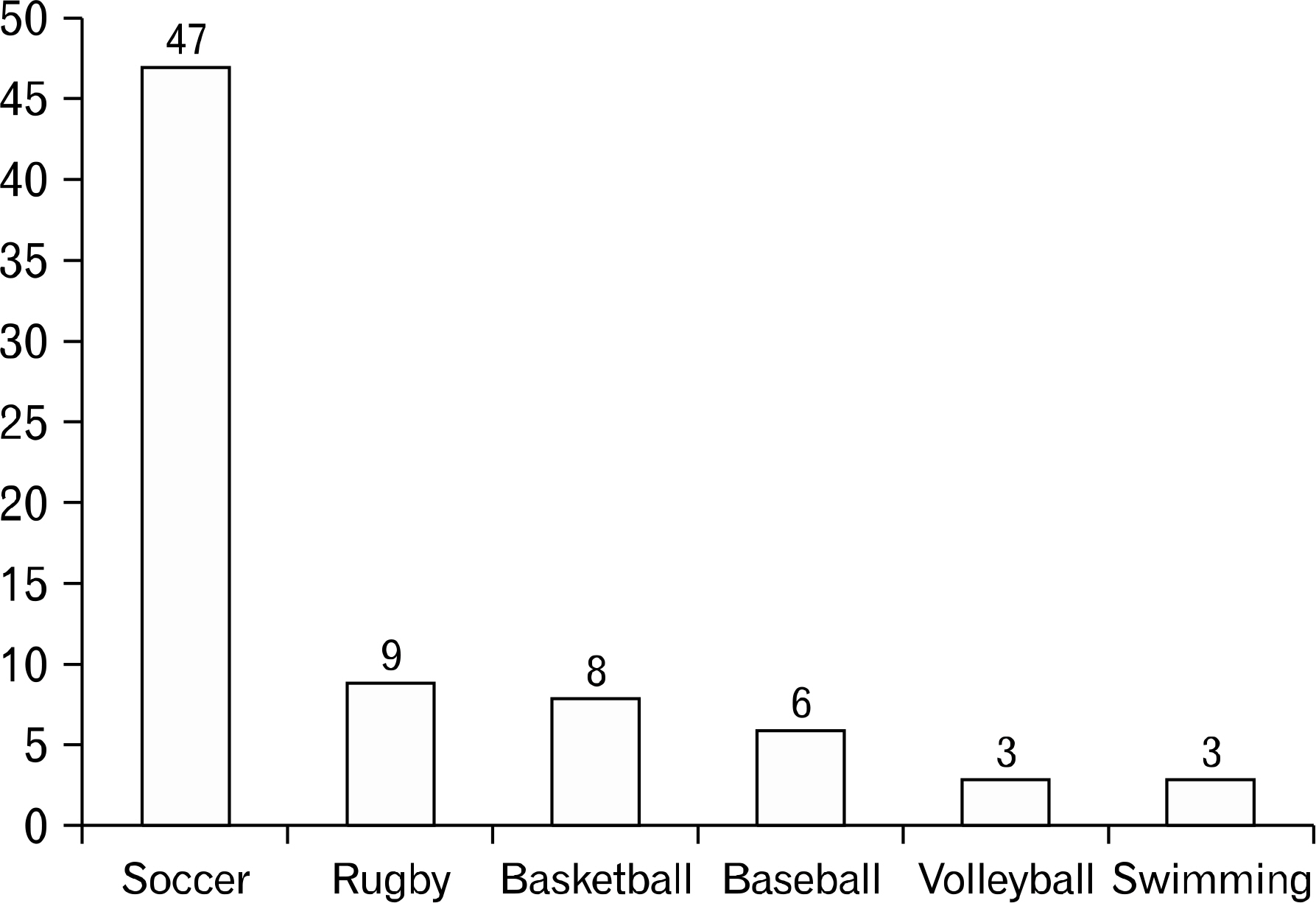
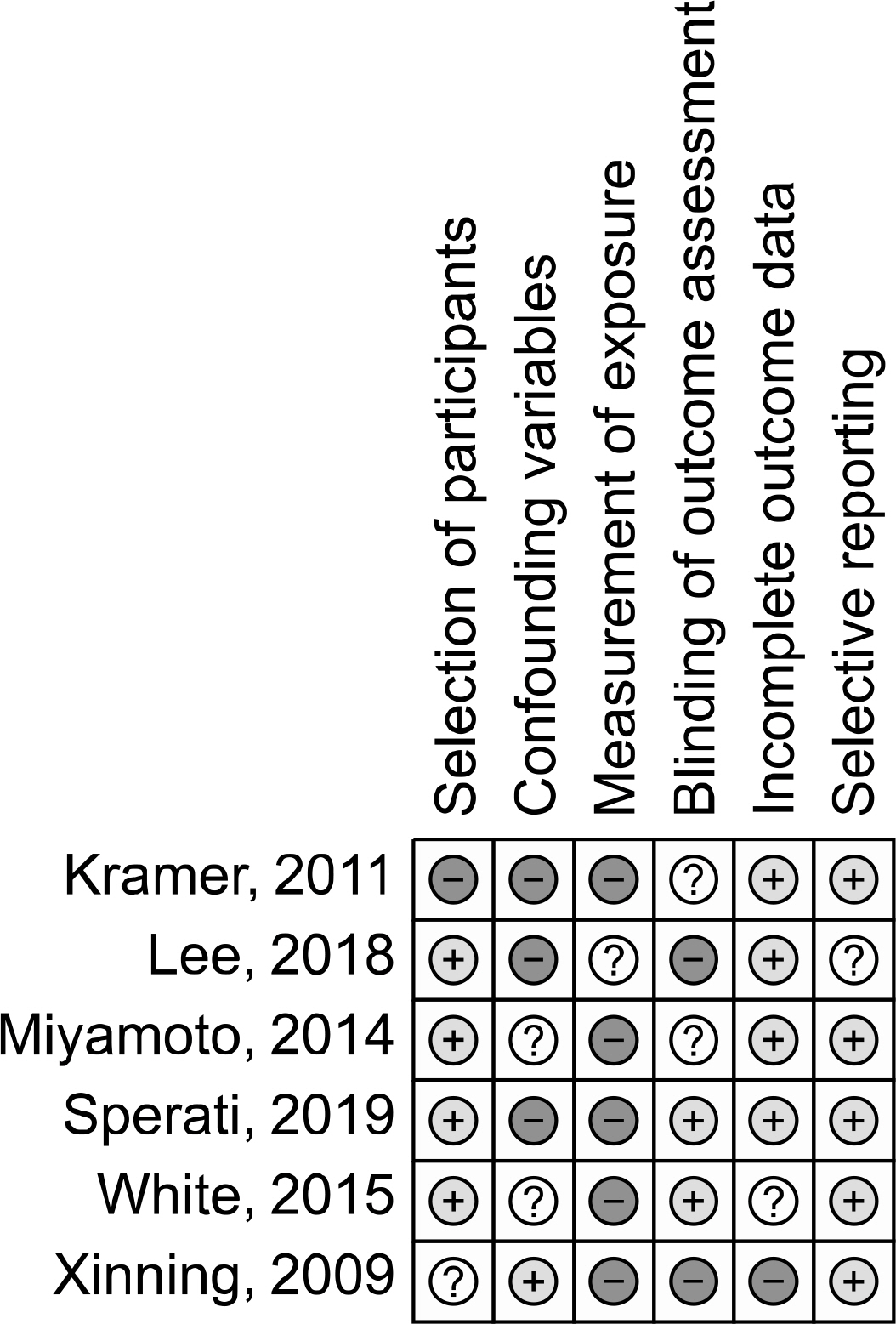
A literature search was conducted (1976 to 2019) by two independent reviewers using the Medline, Embase, and Cochrane library databases. Articles were retrieved by an electronic search using individual keywords (“lateral ankle instability,” “surgery,” “operation,” “return to sport,” “return to play”) and their combinations. Studies that met the inclusion criteria were assessed for pertinent data.
Results
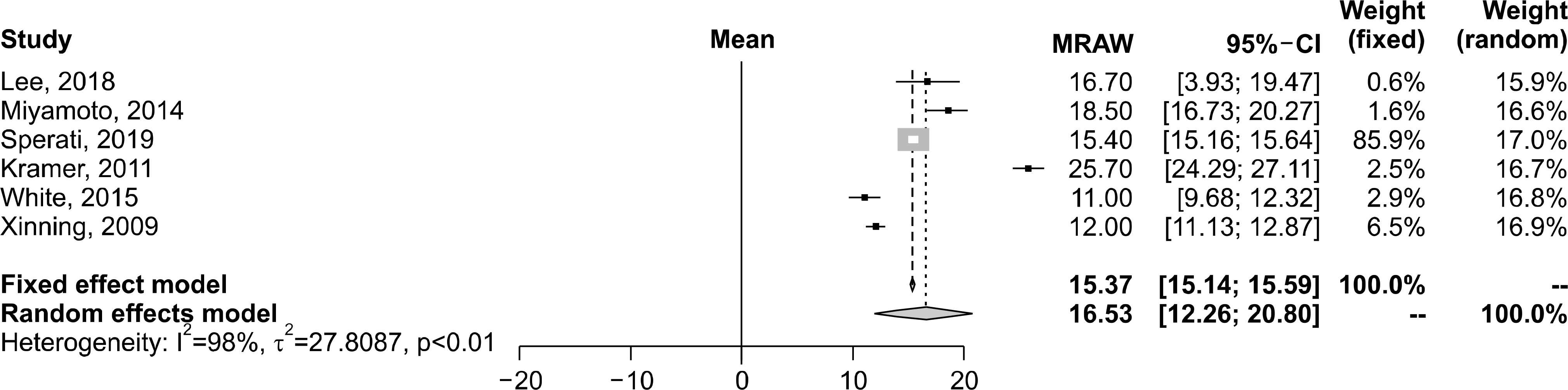
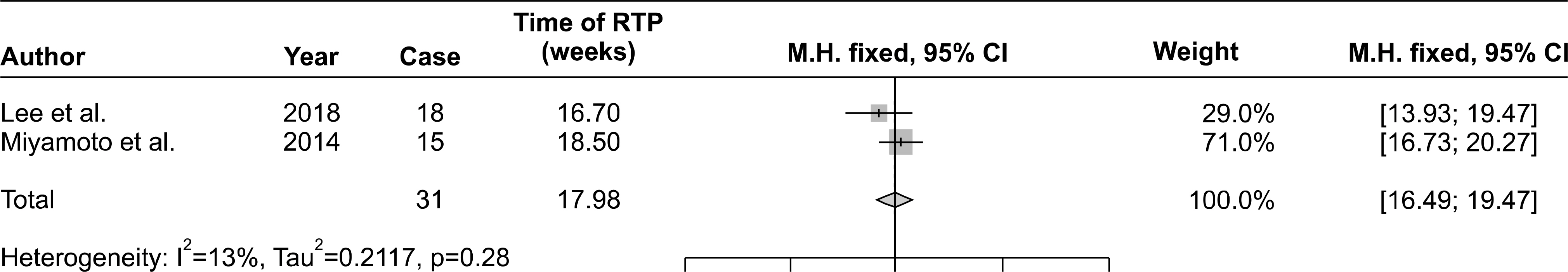
Six randomized controlled trials were included in this analysis. The mean follow-up period was 44.8 months (range, 31.8–58.1 months) in 219 patients (male, 126; female, 113). The mean age was 23.2 years (range, 18.2– 28.2 years). Different criteria for returning to sports were used in each paper. In the papers included in this study, different methods and definitions were used for the postoperative recovery method for lateral ankle instability injury. The average time until return to play was 16.53 weeks.
Conclusion
There are limitations to the application of different surgical techniques and data from different athletes for chronic lateral ankle instability. However, these results suggest that sports physicians evaluate the surgical outcome and may be utilized as reference data for informing the athletes about their time until return.
Keyword
Figure
Cited by 1 articles
-
Treatment of Chronic Lateral Ankle Instability: A Modified Broström Technique Using All-Suture Anchor
Sungjoon Lim, Nam Jun Baek, Geon Jung Kim
Korean J Sports Med. 2024;42(2):119-125. doi: 10.5763/kjsm.2024.42.2.119.
Reference
-
References
1. Fong DT, Hong Y, Chan LK, Yung PS, Chan KM. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007; 37:73–94.
Article2. Kerkhoffs GM, Handoll HH, de Bie R, Rowe BH, Struijs PA. Surgical versus conservative treatment for acute injuries of the lateral ligament complex of the ankle in adults. Cochrane Database Syst Rev. 2007; 2:CD000380.
Article3. Ahlgren O, Larsson S. Reconstruction for lateral ligament injuries of the ankle. J Bone Joint Surg Br. 1989; 71:300–3.
Article4. Bell SJ, Mologne TS, Sitler DF, Cox JS. Twenty-six-year results after Brostrom procedure for chronic lateral ankle instability. Am J Sports Med. 2006; 34:975–8.5. Lee KT, Park YU, Kim JS, Kim JB, Kim KC, Kang SK. Long-term results after modified Brostrom procedure without calcaneofibular ligament reconstruction. Foot Ankle Int. 2011; 32:153–7.
Article6. Mabit C, Tourne Y, Besse JL, et al. Chronic lateral ankle instability surgical repairs: the long term prospective. Orthop Traumatol Surg Res. 2010; 96:417–23.
Article7. Gribble PA, Bleakley CM, Caulfield BM, et al. 2016 Consensus statement of the International Ankle Consortium: prevalence, impact and longterm consequences of lateral ankle sprains. Br J Sports Med. 2016; 50:1493–5.
Article8. Swenson DM, Collins CL, Fields SK, Comstock RD. Epidemiology of U.S. high school sports-related ligamentous ankle injuries, 2005/06–2010/11. Clin J Sport Med. 2013; 23:190–6.
Article9. Swenson DM, Yard EE, Fields SK, Comstock RD. Patterns of recurrent injuries among US high school athletes, 2005–2008. Am J Sports Med. 2009; 37:1586–93.
Article10. Malliaropoulos N, Ntessalen M, Papacostas E, Longo UG, Maffulli N. Reinjury after acute lateral ankle sprains in elite track and field athletes. Am J Sports Med. 2009; 37:1755–61.
Article11. Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007; 42:311–9.12. Gribble PA, Bleakley CM, Caulfield BM, et al. Evidence review for the 2016 International Ankle Consortium consensus statement on the prevalence, impact and longterm consequences of lateral ankle sprains. Br J Sports Med. 2016; 50:1496–505.
Article13. Birrer RB, Fani-Salek MH, Totten VY, Herman LM, Politi V. Managing ankle injuries in the emergency department. J Emerg Med. 1999; 17:651–60.
Article14. Higgins J, Green S. Cochrane handbook for systematic reviews of interventions. London: John Wiley & Sons;2008.15. Park J, Lee Y, Seo H, et al. Risk of bias assessment tool for non-randomized studies (RoBANS): development and validation of a new instrument. In: Proceedings of the 19th Cochrane Colloquium;. 2011. Oct 19–22; Madrid, Spain.16. Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and metaanalyses: the PRISMA statement. Int J Surg. 2010; 8:336–41.
Article17. Lee K, Jegal H, Chung H, Park Y. Return to play after modified Brostrom operation for chronic ankle instability in elite athletes. Clin Orthop Surg. 2019; 11:126–30.18. Miyamoto W, Takao M, Yamada K, Matsushita T. Accelerated versus traditional rehabilitation after anterior talofibular ligament reconstruction for chronic lateral instability of the ankle in athletes. Am J Sports Med. 2014; 42:1441–7.
Article19. Sperati G, Ceri L. Hemi-castaing ligamentoplasty for the surgical treatment of chronic lateral ankle instability in young athletes: our 7 years experience. Acta Biomed. 2018; 90:141–5.20. Kramer D, Solomon R, Curtis C, Zurakowski D, Micheli LJ. Clinical results and functional evaluation of the Chrisman-Snook procedure for lateral ankle instability in athletes. Foot Ankle Spec. 2011; 4:18–28.
Article21. White WJ, McCollum GA, Calder JD. Return to sport following acute lateral ligament repair of the ankle in professional athletes. Knee Surg Sports Traumatol Arthrosc. 2016; 24:1124–9.
Article22. Li X, Killie H, Guerrero P, Busconi BD. Anatomical reconstruction for chronic lateral ankle instability in the high-demand athlete: functional outcomes after the modified Brostrom repair using suture anchors. Am J Sports Med. 2009; 37:488–94.23. Kerkhoffs GM, van den Bekerom M, Elders LA, et al. Diagnosis, treatment and prevention of ankle sprains: an evidencebased clinical guideline. Br J Sports Med. 2012; 46:854–60.
Article24. Tassignon B, Verschueren J, Delahunt E, et al. Criteria-based return to sport decision-making following lateral ankle sprain injury: a systematic review and narrative synthesis. Sports Med. 2019; 49:601–19.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Return to Play after Modified Broström Operation for Chronic Ankle Instability in Elite Athletes
- Ligament Repair in Chronic Lateral Ankle Instability: Efficacy and Technique of Broström Procedures
- Diagnosis of Lateral Ankle Ligament Injury in the Evaluation of Chronic Lateral Ankle Instability
- Chronic Lateral Ankle Instability
- Arthroscopic Procedure in the Treatment of Chronic Lateral Ankle Instability