Diabetes Metab J.
2020 Apr;44(2):277-285. 10.4093/dmj.2019.0008.
Intra-Abdominal Fat and High Density Lipoprotein Cholesterol Are Associated in a Non-Linear Pattern in Japanese-Americans
- Affiliations
-
- 1Epidemiologic Research and Information Center, VA Puget Sound Health Care System, Seattle, WA, USA
- 2Department of Medicine, University of Washington School of Medicine, Seattle, WA, USA,
- 3Division of Endocrinology and Metabolism, Department of Internal Medicine, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 4Division of Endocrinology and Metabolism, Department of Medicine, Kyung Hee University Hospital at Gangdong, Kyung Hee University School of Medicine, Seoul, Korea
- 5Division of Metabolism, Endocrinology and Nutrition, Department of Medicine, University of Washington School of Medicine, Seattle, WA, USA
- 6Hospital and Specialty Medicine Service, VA Puget Sound Health Care System, Seattle, WA, USA
- 7Department of Anthropology, University of Washington, Seattle, WA, USA
- KMID: 2502409
- DOI: http://doi.org/10.4093/dmj.2019.0008
Abstract
- Background
We describe the association between high density lipoprotein cholesterol (HDL-C) concentration and computed tomography (CT)-measured fat depots.
Methods
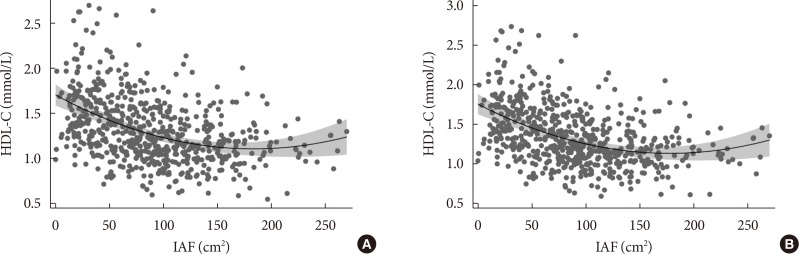
We examined the cross-sectional associations between HDL-C concentration and intra-abdominal (IAF), abdominal subcutaneous (SCF), and thigh fat (TF) areas in 641 Japanese-American men and women. IAF, SCF, and TF were measured by CT at the level of the umbilicus and mid-thigh. The associations between fat area measurements and HDL-C were examined using multivariate linear regression analysis adjusting for age, sex, diabetes family history, homeostasis model assessment of insulin resistance (HOMA-IR), and body mass index (BMI). Non-linearity was assessed using fractional polynomials.
Results
Mean±standard deviation of HDL-C concentration and IAF in men and women were 1.30±0.34 mg/dL, 105±55.3 cm2, and 1.67±0.43 mg/dL, 74.4±46.6 cm2 and differed significantly by gender for both comparisons (P<0.001). In univariate analysis, HDL-C concentration was significantly associated with CT-measured fat depots. In multivariate analysis, IAF was significantly and non-linearly associated with HDL-C concentration adjusted for age, sex, BMI, HOMA-IR, SCF, and TF (IAF: β=–0.1012, P <0.001; IAF2: β=0.0008, P<0.001). SCF was also negatively and linearly associated with HDL-C (β=–0.4919, P=0.001).
Conclusion
HDL-C does not linearly decline with increasing IAF in Japanese-Americans. A more complex pattern better fits this association.
Figure
Cited by 1 articles
-
Lower High-Density Lipoprotein Cholesterol Concentration Is Independently Associated with Greater Future Accumulation of Intra-Abdominal Fat
Sun Ok Song, You-Cheol Hwang, Han Uk Ryu, Steven E. Kahn, Donna L. Leonetti, Wilfred Y. Fujimoto, Edward J. Boyko
Endocrinol Metab. 2021;36(4):835-844. doi: 10.3803/EnM.2021.1130.
Reference
-
1. Heitmann BL, Erikson H, Ellsinger BM, Mikkelsen KL, Larsson B. Mortality associated with body fat, fat-free mass and body mass index among 60-year-old Swedish men-a 22-year follow-up: the study of men born in 1913. Int J Obes Relat Metab Disord. 2000; 24:33–37. PMID: 10702748.
Article2. Kannel WB. Lipids, diabetes, and coronary heart disease: insights from the Framingham Study. Am Heart J. 1985; 110:1100–1107. PMID: 4061265.
Article3. Larsson B. Obesity, fat distribution and cardiovascular disease. Int J Obes. 1991; 15 Suppl 2:53–57. PMID: 1794939.4. Thaete FL, Colberg SR, Burke T, Kelley DE. Reproducibility of computed tomography measurement of visceral adipose tissue area. Int J Obes Relat Metab Disord. 1995; 19:464–467. PMID: 8520635.5. Hayashi T, Boyko EJ, McNeely MJ, Leonetti DL, Kahn SE, Fujimoto WY. Visceral adiposity, not abdominal subcutaneous fat area, is associated with an increase in future insulin resistance in Japanese Americans. Diabetes. 2008; 57:1269–1275. PMID: 18299316.
Article6. Knopp RH, Retzlaff B, Fish B, Walden C, Wallick S, Anderson M, Aikawa K, Kahn SE. Effects of insulin resistance and obesity on lipoproteins and sensitivity to egg feeding. Arterioscler Thromb Vasc Biol. 2003; 23:1437–1443. PMID: 12816878.
Article7. Fujimoto WY, Bergstrom RW, Boyko EJ, Leonetti DL, Newell-Morris LL, Wahl PW. Susceptibility to development of central adiposity among populations. Obes Res. 1995; 3 Suppl 2:179S–186S. PMID: 8581774.
Article8. Gallagher D, Heshka S, Kelley DE, Thornton J, Boxt L, Pi-Sunyer FX, Patricio J, Mancino J, Clark JM. MRI Ancillary Study Group of Look AHEAD Research Group. Changes in adipose tissue depots and metabolic markers following a 1-year diet and exercise intervention in overweight and obese patients with type 2 diabetes. Diabetes Care. 2014; 37:3325–3332. PMID: 25336745.
Article9. Gordon DJ, Rifkind BM. High-density lipoprotein: the clinical implications of recent studies. N Engl J Med. 1989; 321:1311–1316. PMID: 2677733.10. Miller GJ, Miller NE. Plasma-high-density-lipoprotein concentration and development of ischaemic heart-disease. Lancet. 1975; 1:16–19. PMID: 46338.11. Rader DJ. Regulation of reverse cholesterol transport and clinical implications. Am J Cardiol. 2003; 92(4A):42J–49J.
Article12. DeFronzo RA. Dysfunctional fat cells, lipotoxicity and type 2 diabetes. Int J Clin Pract Suppl. 2004; (143):9–21.
Article13. Laszlo A, Simon M. Serum lipid and lipoprotein levels in premature ageing syndromes: total lipodystrophy and Cockayne syndrome. Arch Gerontol Geriatr. 1986; 5:189–196. PMID: 3800489.14. Simha V, Garg A. Body fat distribution and metabolic derangements in patients with familial partial lipodystrophy associated with mandibuloacral dysplasia. J Clin Endocrinol Metab. 2002; 87:776–785. PMID: 11836320.
Article15. Fujimoto WY, Leonetti DL, Kinyoun JL, Shuman WP, Stolov WC, Wahl PW. Prevalence of complications among second-generation Japanese-American men with diabetes, impaired glucose tolerance, or normal glucose tolerance. Diabetes. 1987; 36:730–739. PMID: 3569672.
Article16. Fujimoto WY, Bergstrom RW, Leonetti DL, Newell-Morris LL, Shuman WP, Wahl PW. Metabolic and adipose risk factors for NIDDM and coronary disease in third-generation Japanese-American men and women with impaired glucose tolerance. Diabetologia. 1994; 37:524–532. PMID: 8056192.17. Boyko EJ, Fujimoto WY, Leonetti DL, Newell-Morris L. Visceral adiposity and risk of type 2 diabetes: a prospective study among Japanese Americans. Diabetes Care. 2000; 23:465–471. PMID: 10857936.
Article18. Fujimoto WY, Bergstrom RW, Boyko EJ, Chen KW, Leonetti DL, Newell-Morris L, Shofer JB, Wahl PW. Visceral adiposity and incident coronary heart disease in Japanese-American men: the 10-year follow-up results of the Seattle Japanese-American Community Diabetes Study. Diabetes Care. 1999; 22:1808–1812. PMID: 10546012.
Article19. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985; 28:412–419. PMID: 3899825.20. Shuman WP, Morris LL, Leonetti DL, Wahl PW, Moceri VM, Moss AA, Fujimoto WY. Abnormal body fat distribution detected by computed tomography in diabetic men. Invest Radiol. 1986; 21:483–487. PMID: 3721806.
Article21. Royston P, Altman DG. Regression using fractional polynomials of continuous covariates: parsimonious parametric modelling. J R Stat Soc Ser C Appl Stat. 1994; 43:429–467.
Article22. Taskinen MR. Diabetic dyslipidaemia: from basic research to clinical practice. Diabetologia. 2003; 46:733–749. PMID: 12774165.
Article23. Ibrahim MM. Subcutaneous and visceral adipose tissue: structural and functional differences. Obes Rev. 2010; 11:11–18. PMID: 19656312.
Article24. Lee MJ, Wu Y, Fried SK. Adipose tissue heterogeneity: implication of depot differences in adipose tissue for obesity complications. Mol Aspects Med. 2013; 34:1–11. PMID: 23068073.
Article25. Leenen R, van der Kooy K, Seidell JC, Deurenberg P. Visceral fat accumulation measured by magnetic resonance imaging in relation to serum lipids in obese men and women. Atherosclerosis. 1992; 94:171–181. PMID: 1632871.
Article26. Serra MC, Ryan AS, Sorkin JD, Favor KH, Goldberg AP. High adipose LPL activity and adipocyte hypertrophy reduce visceral fat and metabolic risk in obese, older women. Obesity (Silver Spring). 2015; 23:602–607. PMID: 25612068.
Article27. Lupattelli G, Pirro M, Mannarino MR, Siepi D, Roscini AR, Schillaci G, Mannarino E. Visceral fat positively correlates with cholesterol synthesis in dyslipidaemic patients. Eur J Clin Invest. 2012; 42:164–170. PMID: 21793822.
Article28. Luo Y, Ma X, Shen Y, Hao Y, Hu Y, Xiao Y, Bao Y, Jia W. Positive between serum low-density lipoprotein cholesterol levels and visceral fat in a Chinese nondiabetic population. PLoS One. 2014; 9:e112715. PMID: 25398089.29. Hwang YC, Hayashi T, Fujimoto WY, Kahn SE, Leonetti DL, McNeely MJ, Boyko EJ. Visceral abdominal fat accumulation predicts the conversion of metabolically healthy obese subjects to an unhealthy phenotype. Int J Obes (Lond). 2015; 39:1365–1370. PMID: 25920773.
Article30. Hayashi T, Boyko EJ, Leonetti DL, McNeely MJ, Newell-Morris L, Kahn SE, Fujimoto WY. Visceral adiposity and the risk of impaired glucose tolerance: a prospective study among Japanese Americans. Diabetes Care. 2003; 26:650–655. PMID: 12610016.
Article31. Hwang YC, Fujimoto WY, Kahn SE, Leonetti DL, Boyko EJ. Greater visceral abdominal fat is associated with a lower probability of conversion of prehypertension to normotension. J Hypertens. 2017; 35:1213–1218. PMID: 28169882.
Article32. Wander PL, Boyko EJ, Leonetti DL, McNeely MJ, Kahn SE, Fujimoto WY. Change in visceral adiposity independently predicts a greater risk of developing type 2 diabetes over 10 years in Japanese Americans. Diabetes Care. 2013; 36:289–293. PMID: 22966093.
Article33. Hwang YC, Fujimoto WY, Hayashi T, Kahn SE, Leonetti DL, Boyko EJ. Increased visceral adipose tissue is an independent predictor for future development of atherogenic dyslipidemia. J Clin Endocrinol Metab. 2016; 101:678–685. PMID: 26636177.
Article34. Gotto AM Jr, Brinton EA. Assessing low levels of high-density lipoprotein cholesterol as a risk factor in coronary heart disease: a working group report and update. J Am Coll Cardiol. 2004; 43:717–724. PMID: 14998606.35. Paradis ME, Badellino KO, Rader DJ, Tchernof A, Richard C, Luu-The V, Deshaies Y, Bergeron J, Archer WR, Couture P, Bergeron N, Lamarche B. Visceral adiposity and endothelial lipase. J Clin Endocrinol Metab. 2006; 91:3538–3543. PMID: 16772345.
Article36. Rashid S, Barrett PH, Uffelman KD, Watanabe T, Adeli K, Lewis GF. Lipolytically modified triglyceride-enriched HDLs are rapidly cleared from the circulation. Arterioscler Thromb Vasc Biol. 2002; 22:483–487. PMID: 11884294.
Article37. Rashid S, Watanabe T, Sakaue T, Lewis GF. Mechanisms of HDL lowering in insulin resistant, hypertriglyceridemic states: the combined effect of HDL triglyceride enrichment and elevated hepatic lipase activity. Clin Biochem. 2003; 36:421–429. PMID: 12951168.
Article38. Vajo Z, Terry JG, Brinton EA. Increased intra-abdominal fat may lower HDL levels by increasing the fractional catabolic rate of Lp A-I in postmenopausal women. Atherosclerosis. 2002; 160:495–501. PMID: 11849676.
Article39. Horowitz BS, Goldberg IJ, Merab J, Vanni TM, Ramakrishnan R, Ginsberg HN. Increased plasma and renal clearance of an exchangeable pool of apolipoprotein A-I in subjects with low levels of high density lipoprotein cholesterol. J Clin Invest. 1993; 91:1743–1752. PMID: 8473514.
Article40. Lamarche B, Uffelman KD, Carpentier A, Cohn JS, Steiner G, Barrett PH, Lewis GF. Triglyceride enrichment of HDL enhances in vivo metabolic clearance of HDL apo A-I in healthy men. J Clin Invest. 1999; 103:1191–1199. PMID: 10207171.
Article41. Zanoni P, Khetarpal SA, Larach DB, Hancock-Cerutti WF, Millar JS, Cuchel M, DerOhannessian S, Kontush A, Surendran P, Saleheen D, Trompet S, Jukema JW, De Craen A, Deloukas P, Sattar N, Ford I, Packard C, Majumder Aa, Alam DS, Di Angelantonio E, Abecasis G, Chowdhury R, Erdmann J, Nordestgaard BG, Nielsen SF, Tybjaerg-Hansen A, Schmidt RF, Kuulasmaa K, Liu DJ, Perola M, Blankenberg S, Salomaa V, Mannisto S, Amouyel P, Arveiler D, Ferrieres J, Muller-Nurasyid M, Ferrario M, Kee F, Willer CJ, Samani N, Schunkert H, Butterworth AS, Howson JM, Peloso GM, Stitziel NO, Danesh J, Kathiresan S, Rader DJ. CHD Exome+ Consortium. CARDIoGRAM Exome Consortium. Global Lipids Genetics Consortium. Rare variant in scavenger receptor BI raises HDL cholesterol and increases risk of coronary heart disease. Science. 2016; 351:1166–1171. PMID: 26965621.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Correlation between the Triglyceride to High Density Lipoprotein Cholesterol Ratio and Computed Tomography-Measured Visceral Fat and Cardiovascular Disease Risk Factors in Local Adult Male Subjects
- Lower High-Density Lipoprotein Cholesterol Concentration Is Independently Associated with Greater Future Accumulation of Intra-Abdominal Fat
- Higher High Density Lipoprotein 2 (HDL2) to Total HDL Cholesterol Ratio Is Associated with a Lower Risk for Incident Hypertension
- Predictors of Serum Low-Density Lipoprotein Cholesterol Level in Postmenopausal Women
- Hypolipidemic Effects and Safety of Lovastatin in Patients with Primary Hypercholesterolemia