Ann Surg Treat Res.
2020 Jun;98(6):324-331. 10.4174/astr.2020.98.6.324.
Incidence and outcome of isolated distal deep vein thrombosis in kidney transplant recipients
- Affiliations
-
- 1Division of Vascular and Transplant Surgery, Department of Surgery, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Division of Vascular and Transplant Surgery, Department of Surgery, Bucheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Bucheon, Korea
- 3Division of Vascular and Transplant Surgery, Department of Surgery, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4Division of Vascular and Transplant Surgery, Department of Surgery, Yeouido St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 5Division of Vascular and Transplant Surgery, Department of Surgery, Uijeongbu St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Uijeongbu, Korea
- KMID: 2502118
- DOI: http://doi.org/10.4174/astr.2020.98.6.324
Abstract
- Purpose
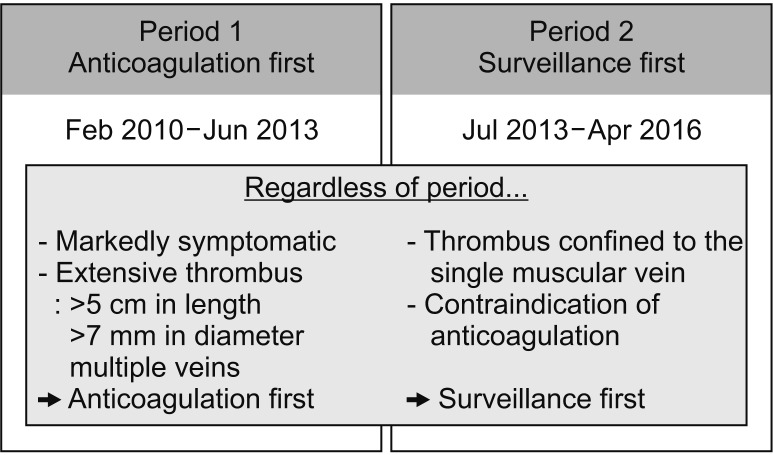
Isolated distal deep vein thrombosis (IDDVT) is a localized lesion; nonetheless, the risk of proximal vein propagation makes it difficult to decide on the treatment protocol—that is, whether immediate anticoagulation after diagnosis or surveillance via serial imaging should be employed. This study aimed to investigate the appropriate treatment protocol for IDDVT in kidney transplant recipient (KTR).
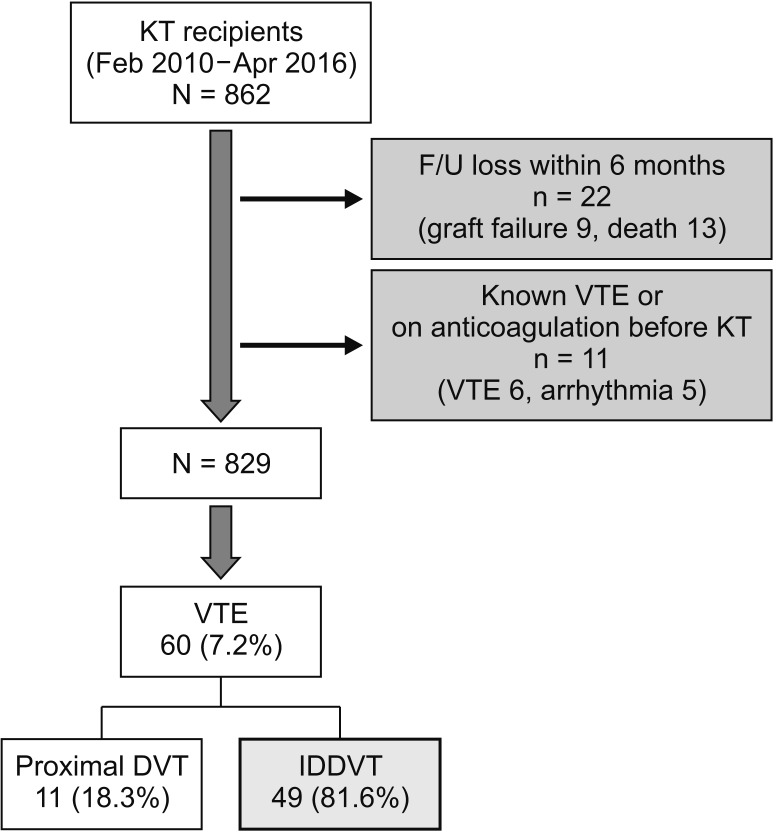
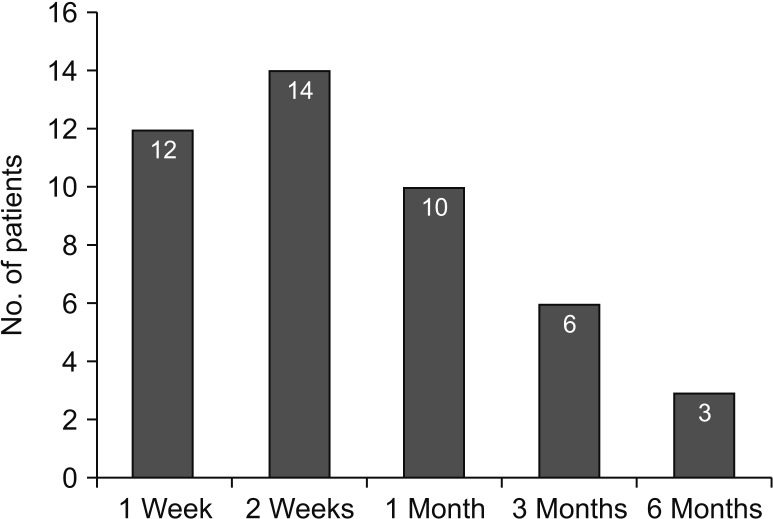
Methods
Surveillance for venous thromboembolism (VTE) was performed using duplex ultrasonography (DUS) before transplant surgery and at 1 week, 2 weeks, 1 month, 3 months, 6 months, and 1 year after transplant surgery. Dual mechanical prophylaxis was administered to prevent VTE.
Results
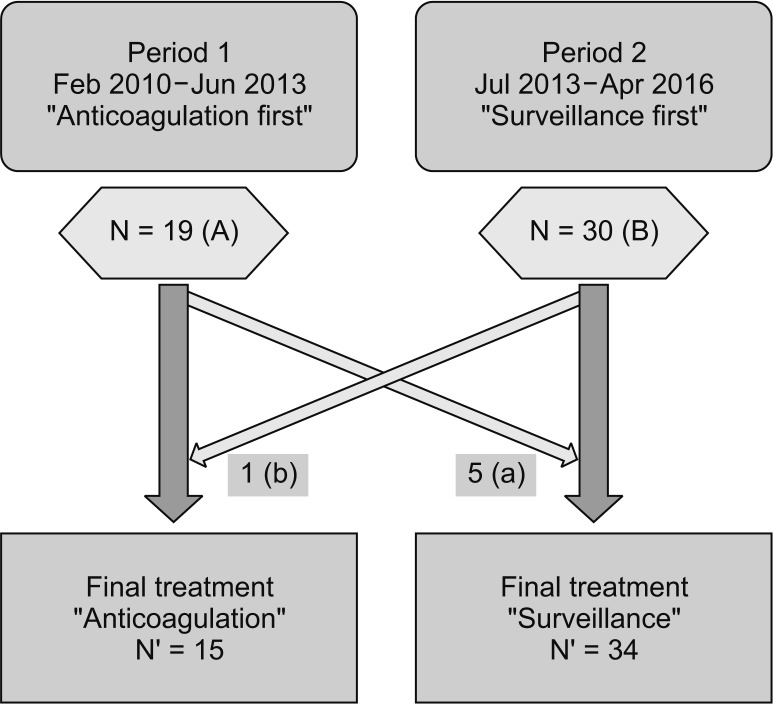
In total, 60 out of 829 patients (7.2%) developed VTE, with 49 cases (81.6%) of IDDVT. Among IDDVT patients, 15 patients were treated using anticoagulation-first strategy, whereas the remaining 34 patients were treated using surveillance-first strategy. No patient in either group exhibited thrombus extension into the proximal vein or recurrence within 1 year from transplant surgery.
Conclusion
In Korean KTR, extension of IDDVT into the proximal vein could be prevented safely and effectively by serial DUS surveillance along with the maintenance of mechanical prophylaxis. However, the patients who have high thrombus burden or are difficult to get repeated DUS require the use of anticoagulation in early stages.
Figure
Cited by 1 articles
-
Retroperitoneal
Viscum album extract instillation in patients with a large amount of drainage after kidney transplantation
Young Jun Park, Sang Kyun Mok, Jang Yong Kim, Sang Seob Yun, Sun Cheol Park
Ann Surg Treat Res. 2021;101(6):368-373. doi: 10.4174/astr.2021.101.6.368.
Reference
-
1. Solis MM, Ranval TJ, Nix ML, Eidt JF, Nelson CL, Ferris EJ, et al. Is anticoagulation indicated for asymptomatic postoperative calf vein thrombosis? J Vasc Surg. 1992; 16:414–418. PMID: 1522645.2. Macdonald PS, Kahn SR, Miller N, Obrand D. Short-term natural history of isolated gastrocnemius and soleal vein thrombosis. J Vasc Surg. 2003; 37:523–527. PMID: 12618686.3. Schwarz T, Buschmann L, Beyer J, Halbritter K, Rastan A, Schellong S. Therapy of isolated calf muscle vein thrombosis: a randomized, controlled study. J Vasc Surg. 2010; 52:1246–1250. PMID: 20630682.4. Deitcher SR, Caprini JA. Calf deep venous thrombosis should be treated with anticoagulation. Med Clin North Am. 2003; 87:1157–1164. PMID: 14680297.5. Masuda EM, Kistner RL. The case for managing calf vein thrombi with duplex surveillance and selective anticoagulation. Dis Mon. 2010; 56:601–613. PMID: 20971331.6. Kearon C, Akl EA, Ornelas J, Blaivas A, Jimenez D, Bounameaux H, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 2016; 149:315–352. PMID: 26867832.7. Ahn S, Kim MH, Jun KW, Hwang JK, Park SC, Moon IS, et al. The incidence and risk factors for deep vein thrombosis after kidney transplantation in Korea: single-center experience. Clin Transplant. 2015; 29:1181–1186. PMID: 26447458.8. Andrassy J, Zeier M, Andrassy K. Do we need screening for thrombophilia prior to kidney transplantation? Nephrol Dial Transplant. 2004; 19 Suppl 4:iv64–iv68. PMID: 15240853.9. Kazory A, Ducloux D. Acquired hypercoagulable state in renal transplant recipients. Thromb Haemost. 2004; 91:646–654. PMID: 15045124.10. Todeschini P, La Manna G, Dalmastri V, Feliciangeli G, Cuna V, Montanari M, et al. Incidence of late deep venous thrombosis among renal transplant patients. Transplant Proc. 2013; 45:2666–2668. PMID: 24034019.11. Verhave JC, Tagalakis V, Suissa S, Madore F, Hebert MJ, Cardinal H. The risk of thromboembolic events in kidney transplant patients. Kidney Int. 2014; 85:1454–1460. PMID: 24429408.12. Wattanakit K, Cushman M, Stehman-Breen C, Heckbert SR, Folsom AR. Chronic kidney disease increases risk for venous thromboembolism. J Am Soc Nephrol. 2008; 19:135–140. PMID: 18032796.13. Humar A, Johnson EM, Gillingham KJ, Sutherland DE, Payne WD, Dunn DL, et al. Venous thromboembolic complications after kidney and kidney-pancreas transplantation: a multivariate analysis. Transplantation. 1998; 65:229–234. PMID: 9458020.14. Kearon C, Akl EA, Comerota AJ, Prandoni P, Bounameaux H, Goldhaber SZ, et al. Antithrombotic therapy for VTE disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012; 141:e419S–e496S. PMID: 22315268.15. Allen RD, Michie CA, Murie JA, Morris PJ. Deep venous thrombosis after renal transplantation. Surg Gynecol Obstet. 1987; 164:137–142. PMID: 3544275.16. White RH, Keenan CR. Effects of race and ethnicity on the incidence of venous thromboembolism. Thromb Res. 2009; 123 Suppl 4:S11–S17. PMID: 19303496.17. Heit JA. The epidemiology of venous thromboembolism in the community: implications for prevention and management. J Thromb Thrombolysis. 2006; 21:23–29. PMID: 16475038.18. Naess IA, Christiansen SC, Romundstad P, Cannegieter SC, Rosendaal FR, Hammerstrom J. Incidence and mortality of venous thrombosis: a population-based study. J Thromb Haemost. 2007; 5:692–699. PMID: 17367492.19. Lee LH, Gallus A, Jindal R, Wang C, Wu CC. Incidence of venous thromboembolism in Asian populations: a systematic review. Thromb Haemost. 2017; 117:2243–2260. PMID: 29212112.20. Jang MJ, Bang SM, Oh D. Incidence of venous thromboembolism in Korea: from the Health Insurance Review and Assessment Service database. J Thromb Haemost. 2011; 9:85–91. PMID: 20942850.21. Min SK, Kim YH, Joh JH, Kang JM, Park UJ, Kim HK, et al. Diagnosis and treatment of lower extremity deep vein thrombosis: Korean practice guidelines. Vasc Specialist Int. 2016; 32:77–104. PMID: 27699156.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Incidence of Deep Vein Thrombosis in the Lower Extremity
- Late Onset Renal Vein Thrombosis after Kidney Transplantation
- Symptomatic Lower Extremity Deep Vein Thrombosis after Kidney Transplantation: a 40-Year Single Center Experience in Korea
- Renal Cell Carcinoma with Deep Vein Thrombosis
- Deep Venous Thrombosis and Heterotopic Ossification in the Patients with Traumatic Spinal Cord Injury