Ann Surg Treat Res.
2020 Jun;98(6):315-323. 10.4174/astr.2020.98.6.315.
Effect of laparoscopic surgery on the risk for surgical site infections in colorectal resection: results from the Health Insurance Review & Assessment Service Database
- Affiliations
-
- 1Department of Surgery, Yonsei University Wonju College of Medicine, Wonju, Korea
- 2The Graduate School, Yonsei University Wonju College of Medicine, Wonju, Korea
- KMID: 2502117
- DOI: http://doi.org/10.4174/astr.2020.98.6.315
Abstract
- Purpose
To compare the hospital length of stay (LOS), duration of antibiotic use, medical costs, and incidence of surgical site infection (SSI) between laparoscopic colorectal surgery (Lap-CRS) and open CRS (Open-CRS).
Methods
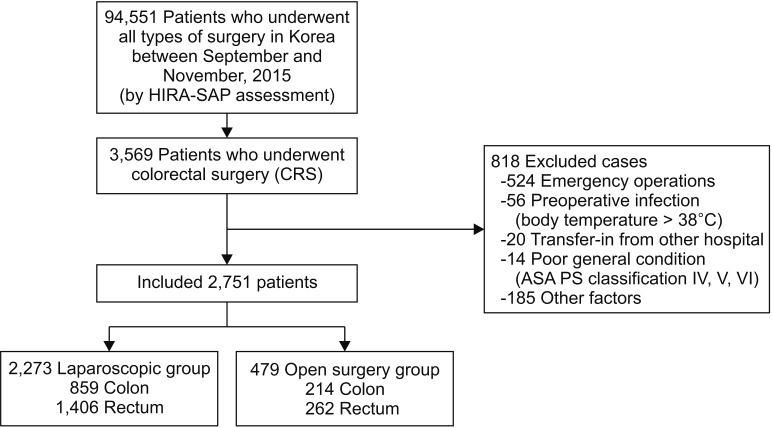
We retrospectively reviewed data of the Health Insurance Review and Assessment Service Surgical Antibiotic Prophylaxis assessment (7th assessment, 2015); the nationwide data were collected from patients who underwent CRS from September to November 2015 in low volume hospital to the tertiary hospital level in Korea.
Results
All 2,751 patients who underwent elective CRS were assessed. The mean hospital LOS (12.18 days vs. 14.16 days, P < 0.001) and mean postoperative LOS (8.21 days vs. 9.46 days, P < 0.001) were shorter in the Lap-CRS group than in the Open-CRS group. The mean duration of antibiotic use was shorter in the Lap-CRS group (2.91 days vs. 3.64 days, P = 0.033). The rate of SSI was lower in the Lap-CRS group, but there was no significant difference between the groups (3.57% vs. 5.01%, P = 0.133). Among the SSI group, the mean LOS (19.5 days vs. 24.9 days, P = 0.081), duration of antibiotic use (12.62 days vs. 15.46 days, P = 0.097), and medical costs showed no significant difference between the 2 groups.
Conclusion
Lap-CRS is significantly associated with reduced hospital LOS and the duration of antibiotic use in this study. However, we could not identify significant differences in the incidence of SSI according to the type of surgery. To assess the overall benefits of Lap-CRS, studies including the rate of SSI up to 30 days postoperatively will be needed in the future.
Keyword
Figure
Cited by 1 articles
-
The risk of surgical site infection of oral sulfate tablet
versus sodium picosulfate for bowel preparation in colorectal cancer surgery: a randomized clinical trial
Sung Sil Park, Sung Chan Park, Dong-Eun Lee, Dong Woon Lee, Kiho Yu, Hyoung-Chul Park, Chang Won Hong, Dae Kyung Sohn, Kyung Su Han, Bun Kim, Byung Chang Kim, Jae Hwan Oh
Ann Surg Treat Res. 2022;103(2):96-103. doi: 10.4174/astr.2022.103.2.96.
Reference
-
1. Jayne DG, Thorpe HC, Copeland J, Quirke P, Brown JM, Guillou PJ. Five-year follow-up of the Medical Research Council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. Br J Surg. 2010; 97:1638–1645. PMID: 20629110.2. Braga M, Vignali A, Gianotti L, Zuliani W, Radaelli G, Gruarin P, et al. Laparoscopic versus open colorectal surgery: a randomized trial on short-term outcome. Ann Surg. 2002; 236:759–766. PMID: 12454514.3. Kim IY, Kim BR, Kim YW. The short-term and oncologic outcomes of laparoscopic versus open surgery for T4 colon cancer. Surg Endosc. 2016; 30:1508–1518. PMID: 26123346.4. Jensen CC, Prasad LM, Abcarian H. Costeffectiveness of laparoscopic vs open resection for colon and rectal cancer. Dis Colon Rectum. 2012; 55:1017–1023. PMID: 22965399.5. Kim MK, Lee IK, Kang WK, Cho HM, Kye BH, Jalloun HE, et al. Long-term oncologic outcomes of laparoscopic surgery for splenic flexure colon cancer are comparable to conventional open surgery. Ann Surg Treat Res. 2017; 93:35–42. PMID: 28706889.6. Poon JT, Law WL, Wong IW, Ching PT, Wong LM, Fan JK, et al. Impact of laparoscopic colorectal resection on surgical site infection. Ann Surg. 2009; 249:77–81. PMID: 19106679.7. Paulson EC, Thompson E, Mahmoud N. Surgical site infection and colorectal surgical procedures: a prospective analysis of risk factors. Surg Infect (Larchmt). 2017; 18:520–526. PMID: 28437196.8. Kirkland KB, Briggs JP, Trivette SL, Wilkinson WE, Sexton DJ. The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs. Infect Control Hosp Epidemiol. 1999; 20:725–730. PMID: 10580621.9. Park ES, Kim KS, Lee WJ, Jang SY, Choi JY, Kim JM. The economical impacts of surgical site infections. Korean J Nosocomial Infect Control. 2005; 10:57–64.10. Chida K, Watanabe J, Suwa Y, Suwa H, Momiyama M, Ishibe A, et al. Risk factors for incisional surgical site infection after elective laparoscopic colorectal surgery. Ann Gastroenterol Surg. 2019; 3:202–208. PMID: 30923790.11. National Nosocomial Infections Surveillance System. National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control. 2004; 32:470–485. PMID: 15573054.12. Itatsu K, Sugawara G, Kaneoka Y, Kato T, Takeuchi E, Kanai M, et al. Risk factors for incisional surgical site infections in elective surgery for colorectal cancer: focus on intraoperative meticulous wound management. Surg Today. 2014; 44:1242–1252. PMID: 23913010.13. Ghuman A, Chan T, Karimuddin AA, Brown CJ, Raval MJ, Phang PT. Surgical site infection rates following implementation of a colorectal closure bundle in elective colorectal surgeries. Dis Colon Rectum. 2015; 58:1078–1082. PMID: 26445181.14. Brathwaite S, Latchana N, Esemuede I, Harzman A, Husain S. Risk factors for surgical site infection in open and laparoscopic hartmann closure: a multivariate analysis. Surg Laparosc Endosc Percutan Tech. 2017; 27:51–53. PMID: 28145967.15. Kagawa Y, Yamada D, Yamasaki M, Miyamoto A, Mizushima T, Yamabe K, et al. The association between the increased performance of laparoscopic colon surgery and a reduced risk of surgical site infection. Surg Today. 2019; 49:474–481. PMID: 30684051.16. Kang SB, Park JW, Jeong SY, Nam BH, Choi HS, Kim DW, et al. Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol. 2010; 11:637–645. PMID: 20610322.17. Vallance AE, Keller DS, Hill J, Braun M, Kuryba A, van der Meulen J, et al. Role of emergency laparoscopic colectomy for colorectal cancer: a population-based study in England. Ann Surg. 2019; 270:172–179. PMID: 29621034.18. Wyles SM, Miskovic D, Ni Z, Darzi AW, Valori RM, Coleman MG, et al. Development and implementation of the Structured Training Trainer Assessment Report (STTAR) in the English National Training Programme for laparoscopic colorec t a l surger y. Surg Endosc. 2016; 30:993–1003. PMID: 26104793.19. Konishi T, Watanabe T, Kishimoto J, Nagawa H. Elective colon and rectal surgery differ in risk factors for wound infect ion: results of prospect ive surveillance. Ann Surg. 2006; 244:758–763. PMID: 17060769.20. Smith RL, Bohl JK, McElearney ST, Friel CM, Barclay MM, Sawyer RG, et al. Wound infection after elective colorectal resection. Ann Surg. 2004; 239:599–605. PMID: 15082963.21. Vogel TR, Dombrovskiy VY, Lowry SF. In-hospital delay of elective surgery for high volume procedures: the impact on infectious complications. J Am Coll Surg. 2010; 211:784–790. PMID: 20980170.22. Pereira HO, Rezende EM, Couto BR. Length of preoperative hospital stay: a risk factor for reducing surgical infection in femoral fracture cases. Rev Bras Ortop. 2015; 50:638–646. PMID: 27218074.23. Mujagic E, Marti WR, Coslovsky M, Soysal SD, Mechera R, von Strauss M, et al. Associations of hospital length of stay with surgical site infections. World J Surg. 2018; 42:3888–3896. PMID: 29978247.24. Keller DS, Champagne BJ, Reynolds HL Jr, Stein SL, Delaney CP. Cost-effectiveness of laparoscopy in rectal cancer. Dis Colon Rectum. 2014; 57:564–569. PMID: 24819095.25. Keller DS, Delaney CP, Hashemi L, Haas EM. A national evaluation of clinical and economic outcomes in open versus laparoscopic colorectal surgery. Surg Endosc. 2016; 30:4220–4228. PMID: 26715021.26. Liang JT, Shieh MJ, Chen CN, Cheng YM, Chang KJ, Wang SM. Prospective evaluation of laparoscopy-assisted colectomy versus laparotomy with resection for management of complex polyps of the sigmoid colon. World J Surg. 2002; 26:377–383. PMID: 11865378.27. Mar J, Anton-Ladislao A, Ibarrondo O, Arrospide A, Lazaro S, Gonzalez N, et al. Cost-effectiveness analysis of laparoscopic versus open surgery in colon cancer. Surg Endosc. 2018; 32:4912–4922. PMID: 29869084.28. Vignali A, Di Palo S, Tamburini A, Radaelli G, Orsenigo E, Staudacher C. Laparoscopic vs. open colectomies in octogenarians: a case-matched control study. Dis Colon Rectum. 2005; 48:2070–2075. PMID: 16086219.29. Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol. 1992; 13:606–608. PMID: 1334988.30. Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1999; 20:250–278. PMID: 10219875.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic Surgery for Colorectal Cancer in Korea: Nationwide Data from 2008~2013
- Laparoscopic Surgery for Colorectal Cancer in Korea: Nationwide Data from 2013 to 2018
- Laparoscopic and robotic surgery for colorectal cancer in Korea: a nationwide health insurance database analysis from 2019 to 2023
- Laparoscopic Surgery for Colorectal Cancer
- Clinical Effect of Hepatitis B Virus on COVID-19 Infected Patients: A Nationwide Population-Based Study Using the Health Insurance Review & Assessment Service Database