J Korean Neurosurg Soc.
2020 Jan;63(1):89-98. 10.3340/jkns.2018.0177.
Surgical Outcomes According to Dekyphosis in Patients with Ossification of the Posterior Longitudinal Ligament in the Thoracic Spine
- Affiliations
-
- 1Department of Neurosurgery, Spine Center, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- KMID: 2501696
- DOI: http://doi.org/10.3340/jkns.2018.0177
Abstract
Objective
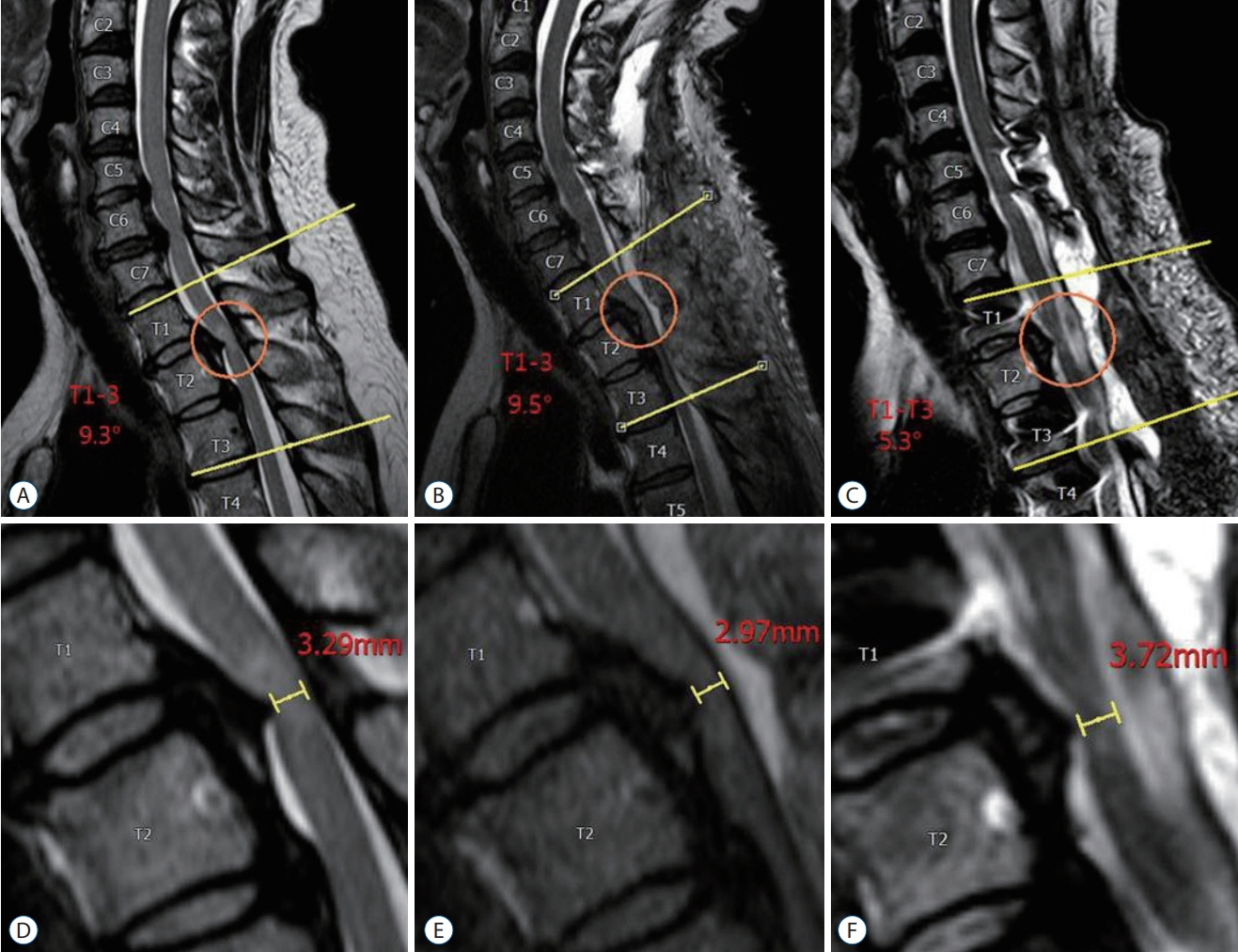
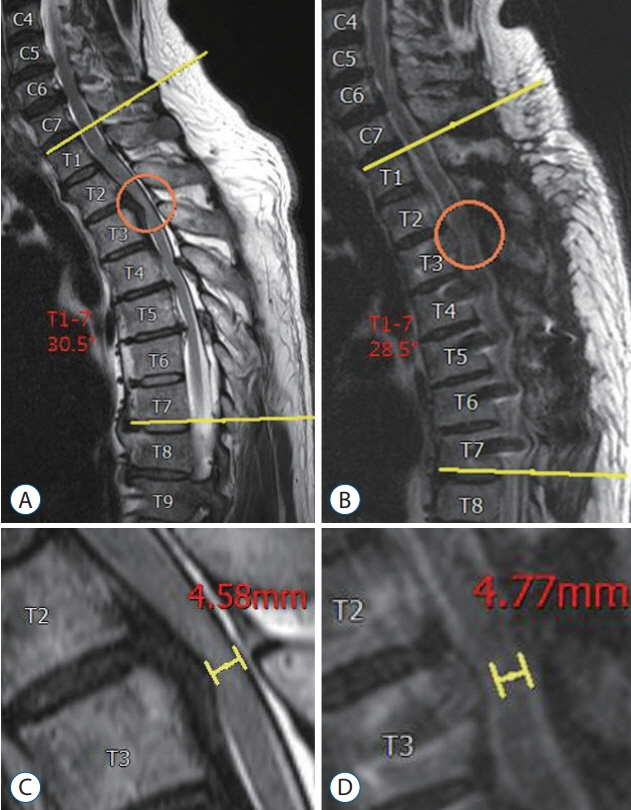
: Ossification of posterior longitudinal ligament (OPLL) in the thoracic spine may cause chronic compressive myelopathy that is usually progressive, and unfavorable by conservative treatment. Although surgical intervention is often needed, the standard surgical method has not been established. Recently, it has been reported that posterior decompression with dekyphosis is effective surgical technique for favorable clinical outcome. The purpose of this study was to evaluate the surgical outcomes in patients with thoracic OPLL according to dekyphosis procedure and to identify predictive factors for the surgical results.
Methods
: A total of 25 patients with thoracic OPLL who underwent surgery for myelopathy from May 2004 to March 2017, were retrospectively reviewed. Patients with cervical myelopathy were excluded. We assessed the clinical outcomes according to various surgical approaches. The modified Japanese orthopedic association (JOA) scores for the thoracic spine (total, 11 points) and JOA recovery rates were used for investigating surgical outcomes.
Results
: Of the 25 patients, 10 patients were male and the others were female. The mean JOA score was 6.7±2.3 points preoperatively and 8.8±1.8 points postoperatively, yielding a mean recovery rate of 53.8±31.0%. The mean patients’ age at surgery was 52.4 years and mean follow-up period was 40.2 months. According to surgical approaches, seven patients underwent anterior approaches, 13 patients underwent posterior approaches, five patients underwent combined approaches. There was no significant difference of the surgical outcomes related with different surgical approaches. Age (≥55 years) and high signal intensity on preoperative magnetic resonance (MR) image in the thoracic spine were significant predictors of the lower recovery rate after surgery (p<0.05). Posterior decompression with dekyphosis procedure was related to the excellent surgical outcomes (p=0.047). Dekyphosis did not affect the complication rates.
Conclusion
: In this study, our result elucidated that old age (≥55 years) and presence of intramedullary high signal intensity on preoperative MR images were risk factors related to poor surgical outcomes. In the meanwhile, posterior decompression with dekyphosis affected favorable clinical outcome. Posterior approach with dekyphosis procedure can be a recommendable surgical option for favorable results.
Keyword
Figure
Reference
-
References
1. Ando K, Imagama S, Kobayashi K, Hida T, Ito K, Tsushima M, et al. Comparative study of surgical treatment and nonsurgical follow up for thoracic ossification of the posterior longitudinal ligament: radiological and clinical evaluation. Spine (Phila Pa 1976). 42:407–410. 2017.
Article2. Fujimura Y, Nishi Y, Nakamura M, Watanabe M, Matsumoto M. Myelopathy secondary to ossification of the posterior longitudinal ligament of the thoracic spine treated by anterior decompression and bony fusion. Spinal Cord. 35:777–784. 1997.
Article3. Hu P, Yu M, Liu X, Liu Z, Jiang L. A circumferential decompressionbased surgical strategy for multilevel ossification of thoracic posterior longitudinal ligament. Spine J. 15:2484–2492. 2015.
Article4. Hyun SJ, Kim JS, Hong SC. Late occurrence of cervicothoracic ossification of posterior longitudinal ligaments in a surgically treated thoracic OPLL patient. J Korean Neurosurg Soc. 47:55–57. 2010.
Article5. Hyun SJ, Kim YJ, Cheh G, Yoon SH, Rhim SC. Free hand pedicle screw placement in the thoracic spine without any radiographic guidance : technical note, a cadaveric study. J Korean Neurosurg Soc. 51:66–70. 2012.
Article6. Hyun SJ, Lee BH, Park JH, Kim KJ, Jahng TA, Kim HJ. Proximal junctional kyphosis and proximal junctional failure following adult spinal deformity surgery. Korean J Spine. 14:126–132. 2017.
Article7. Imagama S, Ando K, Ito Z, Kobayashi K, Hida T, Ito K, et al. Risk factors for ineffectiveness of posterior decompression and dekyphotic corrective fusion with instrumentation for beak-type thoracic ossification of the posterior longitudinal ligament: a single institute study. Neurosurgery. 80:800–808. 2017.
Article8. Kawahara N, Tomita K, Murakami H, Hato T, Demura S, Sekino Y, et al. Circumspinal decompression with dekyphosis stabilization for thoracic myelopathy due to ossification of the posterior longitudinal ligament. Spine (Phila Pa 1976). 33:39–46. 2008.
Article9. Kim B, Yoon DH, Shin HC, Kim KN, Yi S, Shin DA, et al. Surgical outcome and prognostic factors of anterior decompression and fusion for cervical compressive myelopathy due to ossification of the posterior longitudinal ligament. Spine J. 15:875–884. 2015.
Article10. Kim CH, Renaldo N, Chung CK, Lee HS. Use of an ultrasonic osteotome for direct removal of beak-type ossification of posterior longitudinal ligament in the thoracic spine. J Korean Neurosurg Soc. 58:571–577. 2015.
Article11. Kim JK, Ryu HS, Moon BJ, Lee JK. Clinical outcomes and prognostic factors in patients with myelopathy caused by thoracic ossification of the ligamentum flavum. Neurospine. 15:269–276. 2018.
Article12. Koda M, Furuya T, Okawa A, Inada T, Kamiya K, Ota M, et al. Midto long-term outcomes of posterior decompression with instrumented fusion for thoracic ossification of the posterior longitudinal ligament. J Clin Neurosci. 27:87–90. 2016.
Article13. Komagata M, Inahata Y, Nishiyama M, Endo K, Tanaka H, Kobayashi H. Treatment of myelopathy due to cervicothoracic OPLL via open door laminoplasty. J Spinal Disord Tech. 20:342–346. 2007.
Article14. Lee BH, Hyun SJ, Park JH, Kim KJ. Single stage posterior approach for total resection of presacral giant schwannoma: a technical case report. Korean J Spine. 14:89–92. 2017.
Article15. Matsumoto M, Chiba K, Toyama Y, Takeshita K, Seichi A, Nakamura K, et al. Surgical results and related factors for ossification of posterior longitudinal ligament of the thoracic spine: a multi-institutional retrospective study. Spine (Phila Pa 1976). 33:1034–1041. 2008.
Article16. Matsumoto M, Toyama Y, Chikuda H, Takeshita K, Kato T, Shindo S, et al. Outcomes of fusion surgery for ossification of the posterior longitudinal ligament of the thoracic spine: a multicenter retrospective survey: clinical article. J Neurosurg Spine. 15:380–385. 2011.
Article17. Matsunaga S. Updates on ossification of posterior longitudinal ligament. Epidemiology and pathogenesis of OPLL. Clin Calcium. 19:1415–1420. 2009.18. Matsuyama Y, Sakai Y, Katayama Y, Imagama S, Ito Z, Wakao N, et al. Indirect posterior decompression with corrective fusion for ossification of the posterior longitudinal ligament of the thoracic spine: is it possible to predict the surgical results? Eur Spine J. 18:943–948. 2009.
Article19. Matsuyama Y, Yoshihara H, Tsuji T, Sakai Y, Yukawa Y, Nakamura H, et al. Surgical outcome of ossification of the posterior longitudinal ligament (OPLL) of the thoracic spine: implication of the type of ossification and surgical options. J Spinal Disord Tech. 18:492–497. discussion 498. 2005.
Article20. Mori K, Imai S, Kasahara T, Nishizawa K, Mimura T, Matsusue Y. Prevalence, distribution, and morphology of thoracic ossification of the posterior longitudinal ligament in Japanese: results of CT-based crosssectional study. Spine (Phila Pa 1976). 39:394–399. 2014.
Article21. Ohtsuka K, Terayama K, Yanagihara M, Wada K, Kasuga K, Machida T, et al. A radiological population study on the ossification of the posterior longitudinal ligament in the spine. Arch Orthop Trauma Surg. 106:89–93. 1987.
Article22. Shimomura T, Sumi M, Nishida K, Maeno K, Tadokoro K, Miyamoto H, et al. Prognostic factors for deterioration of patients with cervical spondylotic myelopathy after nonsurgical treatment. Spine (Phila Pa 1976). 32:2474–2479. 2007.
Article23. Wu JC, Chen YC, Huang WC. Ossification of the posterior longitudinal ligament in cervical spine: prevalence, management, and prognosis. Neurospine. 15:33–41. 2018.
Article24. Xu N, Yu M, Liu X, Sun C, Chen Z, Liu Z. A systematic review of complications in thoracic spine surgery for ossification of the posterior longitudinal ligament. Eur Spine J. 26:1803–1809. 2017.
Article25. Yamazaki M, Mochizuki M, Ikeda Y, Sodeyama T, Okawa A, Koda M, et al. Clinical results of surgery for thoracic myelopathy caused by ossification of the posterior longitudinal ligament: operative indication of posterior decompression with instrumented fusion. Spine (Phila Pa 1976). 31:1452–1460. 2006.
Article26. Yang B, Wang Y, He X, Li H. Treatment for thoracic ossification of posterior longitudinal ligament with posterior circumferential decompression: complications and managements. J Orthop Surg Res. 11:153. 2016.
Article27. Zhang HQ, Chen LQ, Liu SH, Zhao D, Guo CF. Posterior decompression with kyphosis correction for thoracic myelopathy due to ossification of the ligamentum flavum and ossification of the posterior longitudinal ligament at the same level. J Neurosurg Spine. 13:116–122. 2010.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ossification of the Posterior Longitudinal Ligament: 2 cases report
- Ossification of Posterior Longitudinal Ligament
- Ossification of posterior longitudinal ligament of the cervical spine in Korean
- Anterior Decompression and Interbody Fusion for Ossification of the Posterior Longitudinal Ligament of the Cervical Spine: Case Report
- Genetics of Ossification of the Posterior Longitudinal Ligament of the Spine: A Mini Review