Korean J Women Health Nurs.
2020 Mar;26(1):61-71. 10.4069/kjwhn.2020.03.15.1.
Effects of integrative simulation practice on nursing knowledge, critical thinking, problem-solving ability, and immersion in problem-based learning among nursing students
- Affiliations
-
- 1Department of Nursing, Ansan University, Ansan, Korea
- KMID: 2501577
- DOI: http://doi.org/10.4069/kjwhn.2020.03.15.1
Abstract
- Purpose
This study was conducted to investigate the effects of problem-based learning–integrative simulation practice (PBL-ISP) on nursing knowledge, critical thinking, problem-solving ability, and immersion among nursing students.
Methods
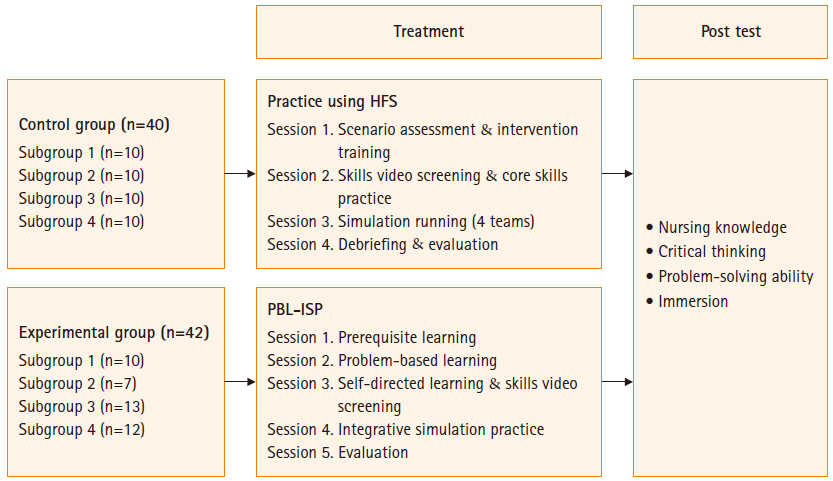
The study used a nonequivalent control group post-test design. A PBL-ISP educational program was provided to the experimental group, and hands-on practice using a high-fidelity simulator (HFS) was administered to the control group. There were 42 subjects in the experimental group and 40 in the control group. Data were collected during the fall semester of 2019. Using SPSS for Windows version 23.0, data were analyzed in terms of frequency, percentage, mean, standard deviation, the chi-square test, t-test, and Pearson correlation coefficients.
Results
Significant differences between the experimental and control groups were found in nursing knowledge (t=3.67, p<.001), critical thinking (t=3.40, p=.001), problem-solving ability (t=3.52, p=.001) and immersion (t=4.44, p<.001).
Conclusion
PBL-ISP was more effective in improving nursing knowledge, critical thinking, problem-solving ability, and immersion than was hands-on practice using an HFS.
Keyword
Figure
Cited by 1 articles
-
Development and effects of a labor nursing education program using a high-fidelity simulator for nursing students in Korea
Seo-A Park, Hye Young Kim
Korean J Women Health Nurs. 2020;26(3):240-249. doi: 10.4069/kjwhn.2020.09.18.
Reference
-
References
1. Thomas RE. Problem-based learning: measurable outcomes. Med Educ. 1997; 31(5):320–329.
Article2. Cannon C, Schell K. Problem-based learning: preparing nurses for practice. In : Duch B, Groh S, Allen D, editors. The power of problem-based learning. Sterling, VI: Stylus Publishing, LLC;2001. p. 165–178.3. Kang IA. PBL theory and practice. Yongin: Moonumsa;2003. p. 53–59.4. Ma RW, Lee EJ, Kim HO, Jee YJ. Study on the simulation-based education using the self-directed learning. Asia-pacific J Multimed Serv Converg Art Humanit Sociol. 2017; 7(6):277–285.5. Kim MO, Lee AY, Nam HA. Effects on nursing students’ learning flow, critical Judgement, and problem-solving ability in simulation training: focused on obstetrical nursing case. J Learner-Cent Curric Instr. 2017; 17(24):521–534.6. Eom MR, Kim HS, Kim EK, Seong KY. Effects of teaching method using standardized patients on nursing competence in subcutaneous injection, self-directed learning readiness, and problem-solving ability. J Korean Acad Nurs. 2010; 40(2):151–160.7. Yoo MS, Yoo IY, Park YO, Son YJ. Comparison of student’s clinical competency in different instructional methods for fundamentals of nursing practicum. J Korean Acad Nurs. 2002; 32(3):327–335.
Article8. Kneebone R. Evaluating clinical simulations for learning procedural skills: a theory-based approach. Acad Med. 2005; 80(6):549–553.
Article9. Ackermann AD, Kenny G, Walker C. Simulator programs for new nurses’ orientation: a retention strategy. J Nurses Staff Dev. 2007; 23(3):136–139.10. Turcato N, Roberson C, Covert K. Simulation-based education: what’s in it for nurse anesthesia educators? AANA J. 2008; 76(4):257–262.11. Song YA. Effect of simulation-based practice by applying problem based learning on problem solving process, self-confidence in clinical performance and nursing competence. Korean J Women Health Nurs. 2014; 20(4):246–254.
Article12. Kim HJ, Chun IH. The effect of problem-based learning and simulation practice convergence education for nursing students. J Korea Converg Soc. 2018; 9(7):355–364.13. Park MJ, Choi D. The effect of simulation integrated with problem based learning on system thinking, learning flow, proactivity in problem solving and performance ability for medication in nursing students. J Digit Converg. 2018; 16(8):221–231.14. Cho OH, Hwang KH. The effect of education based on simulation with problem-based learning on nursing students’ learning motivation, learning strategy, and academic achievement. J Korea Contents Assoc. 2017; 16(7):640–650.
Article15. Kim JS, Kim YH. The effects of simulation practice education applying problem-based learning on problem solving ability, critical thinking and learning satisfaction of nursing students. J Korea Contents Assoc. 2016; 16(12):203–212.
Article16. Kim JI, Kang H, Park S, Ahn S. Current status of women’s health nursing practicum and direction. Korean J Women Health Nurs. 2014; 20(2):173–183.
Article17. Lee WS, Kim M. Effects and adequacy of high-fidelity simulation-based training for obstetrical nursing. J Korean Acad Nurs. 2011; 41(4):433–443.
Article18. Ellis D, Crofts JF, Hunt LP, Read M, Fox R, James M. Hospital, simulation center, and teamwork training for eclampsia management: a randomized controlled trial. Obstet Gynecol. 2008; 111(3):723–731.19. Ryoo EN, Ha EH, Cho JY. Comparison of learning effects using high-fidelity and multi-mode simulation: an application of emergency care for a patient with cardiac arrest. J Korean Acad Nurs. 2013; 43(2):185–193.
Article20. Gates MG, Parr MB, Hughen JE. Enhancing nursing knowledge using high-fidelity simulation. J Nurs Educ. 2012; 51(1):9–15.
Article21. Crea KA. Practice skill development through the use of human patient simulation. Am J Pharm Educ. 2011; 75(9):188.
Article22. Yoon J. Development of an instrument for the measurement of critical thinking disposition: in nursing [dissertation]. Seoul: The Catholic University of Korea;2004. 69.23. Lee SJ, Jang YG, Lee HN, Park GY. A study on the development of life-skills: communication, problem solving, and self-directed learning. Seoul: Korean Educational Development Institute;2003 Dec. p. 139–141. Report No.: RR2003-15-03.24. Shin NM, Kim KS, Kim KY. An empirical study on the cyber-class flow model. Korean J Educ Res. 2005; 43(4):247–276.25. Hwang EH, Kim KH. Differences in critical thinking disposition and life-skills of nursing students: comparison of high school tracks. J Korean Soc Wellness. 2016; 11(1):59–68.26. Song YA. Comparison of learning satisfaction, critical thinking disposition, learning attitude and motivation between PBL and SBL groups. J Korean Acad Soc Nurs Educ. 2008; 14(1):55–62.
Article27. Kim SH, Park IS. Effects of simulation practice by applying problem based learning on the critical thinking disposition, problem-solving process and self-confidence of nursing process in nursing students. J Korea Soc Simul Nurs. 2015; 3(2):1–11.28. Choi E, Kwag Y. Nursing students’ problem solving, and clinical competence between standard patient and high fidelity simulator simulation. Asia-pacific J Multimed Serv Converg Art Humanit Sociol. 2015; 5(2):29–36.
Article29. Joo YJ, Kim JY, Choi HR. Investigating the structural relationship among self-regulated learning, learning flow, satisfaction and learning persistence in corporate e-Learning. J Educ Technol. 2009; 25(4):101–124.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effects of Jigsaw Cooperation Learning on Communication Ability, Problem Solving Ability, Critical Thinking Disposition, Self-directed Learning Ability and Cooperation of Nursing Students
- Effects of Simulation with Problem-based Learning on Care for Patients with Autonomic Dysreflexia
- Planning and Applying Simulation-based Practice for the Achievement of Program Outcomes in Nursing Students
- Metacognition, Learning Flow and Problem Solving Ability in Nursing Simulation Learning
- The Effects of Simulation-based Practice Program on Self-Efficacy, Critical Thinking Disposition, and Problem Solving Process of the Nursing Students