Yeungnam Univ J Med.
2020 Apr;37(2):128-132. 10.12701/yujm.2019.00367.
Extramedullary tanycytic ependymoma of the lumbar spinal cord
- Affiliations
-
- 1Department of Forensic Medicine, School of Medicine, Kyungpook National University, Daegu, Korea
- 2Department of Pathology, Kyungpook National University Hospital, Daegu, Korea
- KMID: 2501420
- DOI: http://doi.org/10.12701/yujm.2019.00367
Abstract
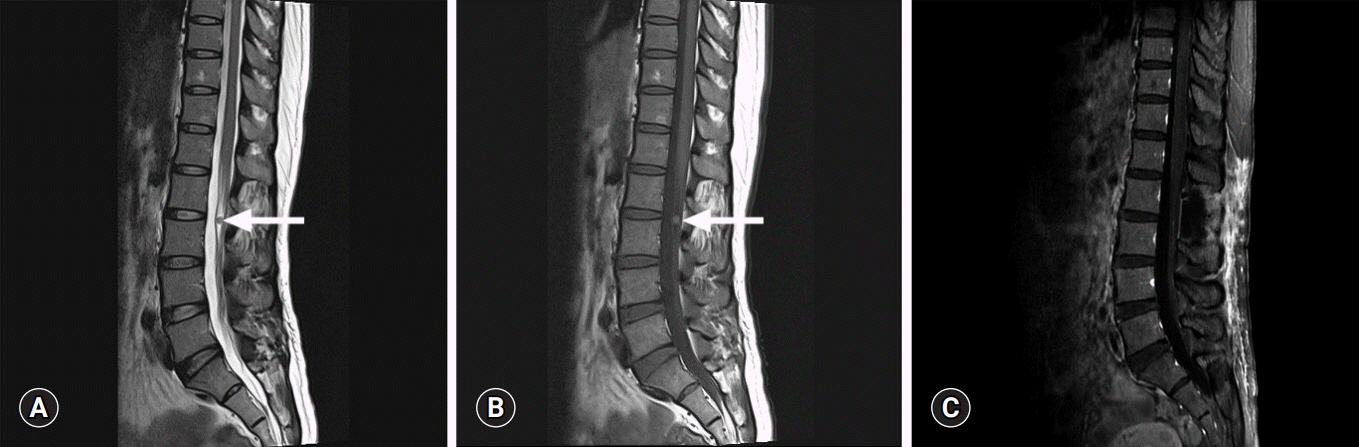
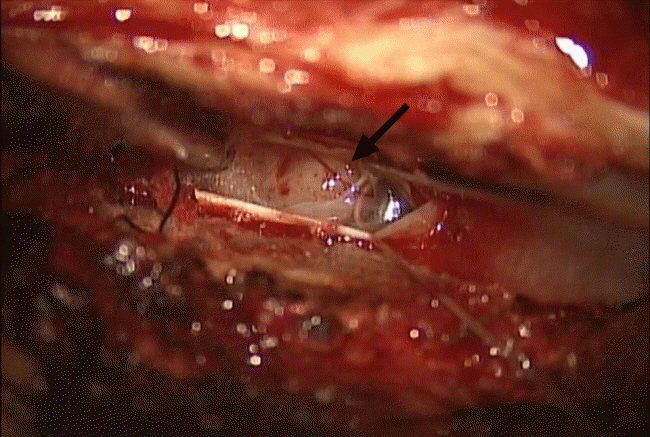
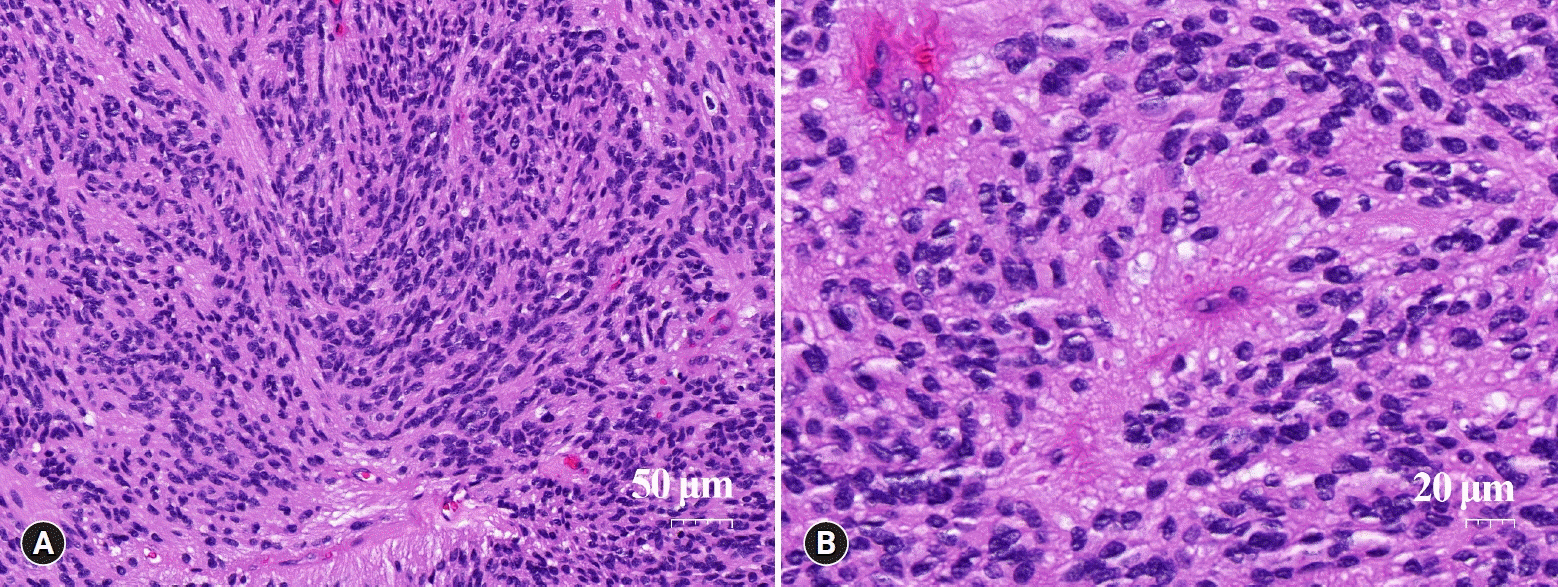
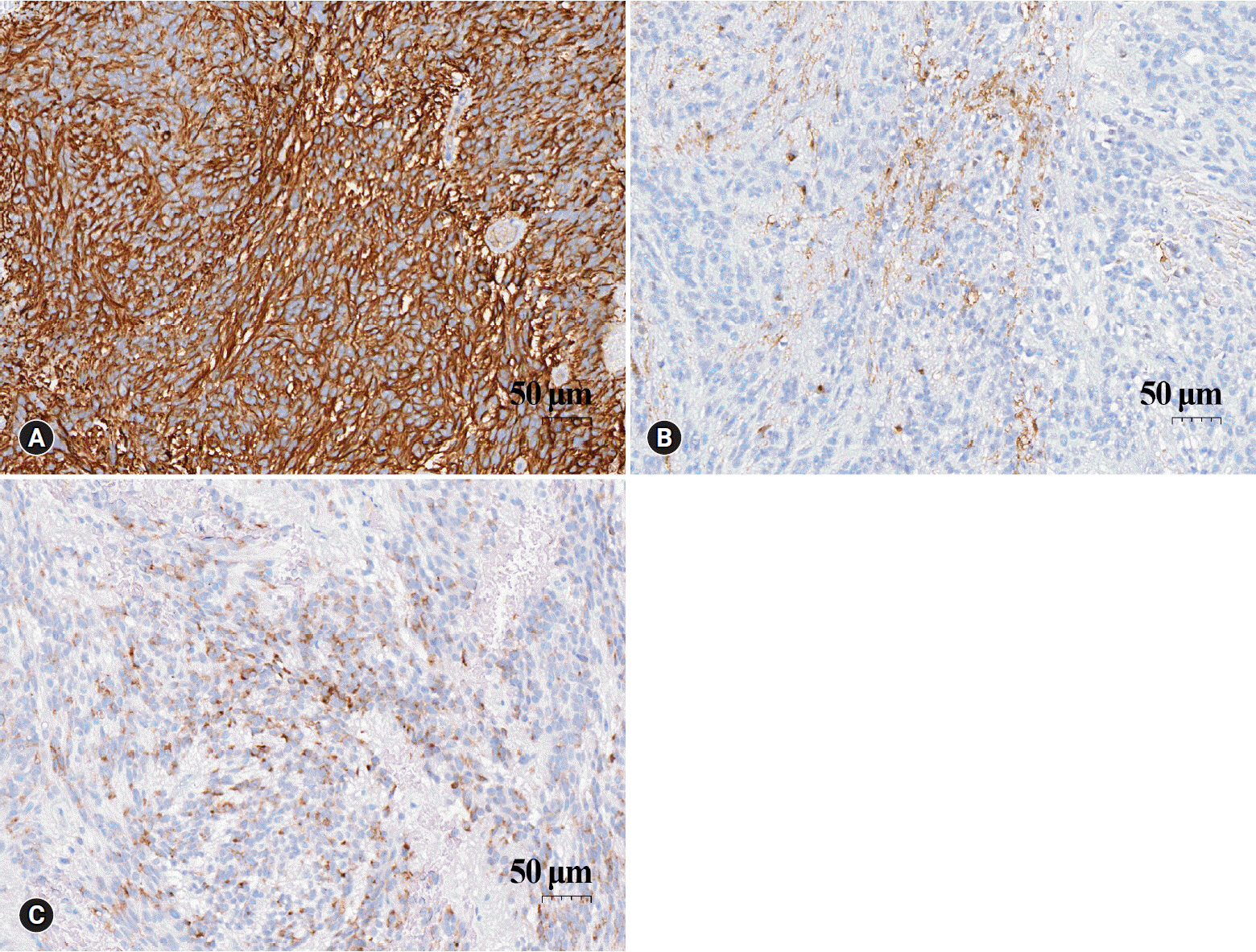
- Tanycytic ependymoma is a rare variant of ependymoma that commonly affects the cervical and thoracic spinal cord. It usually arises as intramedullary lesions, and extramedullary cases are extremely rare. We report a case of a 44-year-old woman who was diagnosed with tanycytic ependymoma in her lumbar spine at level 2-3. The tumor mass developed in an intradural extramedullary location. Histopathologically, tanycytic ependymoma can be misdiagnosed as schwannoma or pilocytic astrocytoma. Immunohistochemical findings such as strong positivity for glial fibrillary acidic protein, perinuclear dot-like positive patterns for epithelial membrane antigen, and focal positivity for S-100 are helpful in diagnosing tanycytic ependymoma. It is important to be aware of this rare tumor to ensure appropriate patient management and accurate prognosis.
Figure
Reference
-
References
1. Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, et al. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol. 2016; 131:803–20.
Article2. Tao X, Hou Z, Hao S, Zhang Q, Wu Z, Zhang J, et al. The clinical features and surgical outcomes of spinal cord tanycytic ependymomas: a report of 40 cases. World Neurosurg. 2017; 106:60–73.
Article3. Friede RL, Pollak A. The cytogenetic basis for classifying ependymomas. J Neuropathol Exp Neurol. 1978; 37:103–18.
Article4. Kawano N, Yagishita S, Oka H, Utsuki S, Kobayashi I, Suzuki S, et al. Spinal tanycytic ependymomas. Acta Neuropathol. 2001; 101:43–8.
Article5. Dvoracek MA, Kirby PA. Intraoperative diagnosis of tanycytic ependymoma: pitfalls and differential diagnosis. Diagn Cytopathol. 2001; 24:289–92.
Article6. Krisht KM, Schmidt MH. Tanycytic ependymoma: a challenging histological diagnosis. Case Rep Neurol Med. 2013; 2013:170791.
Article7. Funayama T, Sakane M, Yoshizawa T, Takeuchi Y, Ochiai N. Tanycytic ependymoma of the filum terminale associated with multiple endocrine neoplasia type 1: first reported case. Spine J. 2013; 13:e49–54.
Article8. Radhakrishnan N, Nair NS, Hingwala DR, Kapilamoorthy TR, Radhakrishnan VV. Tanycytic ependymoma of filum terminale: a case report. Clin Neurol Neurosurg. 2012; 114:169–71.
Article9. D'Souza P, Martin WE, Bodhireddy S, Belirgen M. Extramedullary tanycytic ependymoma in a 12-year-old boy. J Neurosci Rural Pract. 2019; 10:381–3.10. Lim BS, Park SQ, Chang UK, Kim MS. Spinal cord tanycytic ependymoma associated with neurofibromatosis type 2. J Clin Neurosci. 2010; 17:922–4.
Article11. Tao XG, Hou ZG, Hao SY, Zhang JT, Liu BY. Two cases of spinal tanycytic ependymoma associated with neurofibromatosis type 2. Chin Med J (Engl). 2017; 130:872–3.
Article12. Tomek M, Jayajothi A, Brandner S, Jaunmuktane Z, Lee CH, Davagnanam I. Imaging features of spinal tanycytic ependymoma. Neuroradiol J. 2016; 29:61–5.
Article13. Ortiz Ydel M, Perez Berenguer JL, Mercado Acosta J, Polo M, de Jesus-Garces O, Vega IE. Tanycytic ependymoma in a 76-year-old Puerto Rican male. Int J Clin Exp Pathol. 2014; 7:7789–94.14. Wostrack M, Ringel F, Eicker SO, Jagersberg M, Schaller K, Kerschbaumer J, et al. Spinal ependymoma in adults: a multicenter investigation of surgical outcome and progression-free survival. J Neurosurg Spine. 2018; 28:654–62.
Article15. Prayson RA. Clinicopathologic study of 61 patients with ependymoma including MIB-1 immunohistochemistry. Ann Diagn Pathol. 1999; 3:11–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Extra and Intramedullary Anaplastic Ependymoma in Thoracic Spinal Cord
- Intradural Extramedullary Spinal Ependymoma: A Case Report of Malignant Transformation Occurring
- Primary Intradural Extramedullary Myxopapillary Ependymoma
- Non-Enhancing Intradural Extramedullary Ependymoma: A Case Report
- Intradural Extramedullary Ependymoma with Spinal Root Attachment: A Case Report