Yeungnam Univ J Med.
2020 Jan;37(1):67-72. 10.12701/yujm.2019.00360.
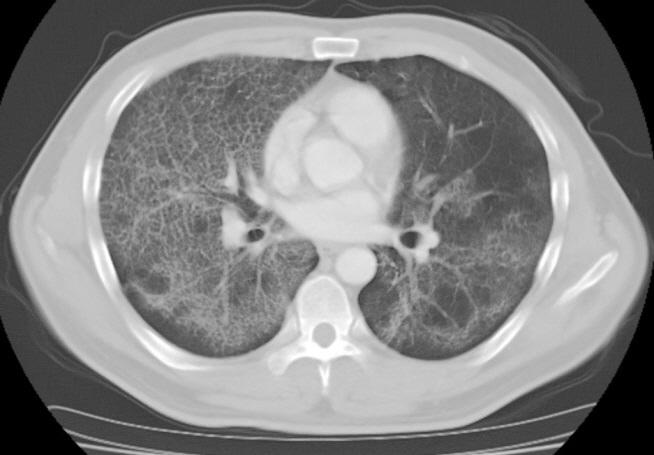
Whole lung lavage using a rapid infusion system to treat a patient with pulmonary alveolar proteinosis
- Affiliations
-
- 1Department of Internal Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea
- 2Department of Anesthesiology and Pain Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea
- KMID: 2501411
- DOI: http://doi.org/10.12701/yujm.2019.00360
Abstract
- Whole lung lavage (WLL) is a therapeutic procedure to remove accumulated material by infusing and draining the lungs with lavage fluid. This procedure has been regarded as the current standard of care to treat pulmonary alveolar proteinosis. However, the WLL protocol has not yet been standardized and the technique has been refined and modified a number of times. A rapid infusion system is a device used to infuse blood or other fluids at precise rates and normothermic conditions. This device is not typically used in WLL, which relies on the passive infusion of fluids using the gravitational force. However, in this study we performed WLL using a rapid infusion system, since we aimed to take advantage of its shorter operation time and greater degree of control over fluid volume and temperature. The patient’s symptoms improved without the occurrence of any complications.
Figure
Cited by 1 articles
-
Anesthetic management during whole-lung lavage using lung ultrasound in a patient with pulmonary alveolar proteinosis: a case report
Jae Wan Jung, Hyunho Lee, Jimi Oh
Yeungnam Univ J Med. 2021;38(4):374-380. doi: 10.12701/yujm.2021.01284.
Reference
-
References
1. Trapnell BC, Whitsett JA, Nakata K. Pulmonary alveolar proteinosis. N Engl J Med. 2003; 349:2527–39.
Article2. Ben-Dov I, Kishinevski Y, Roznman J, Soliman A, Bishara H, Zelligson E, et al. Pulmonary alveolar proteinosis in Israel: ethnic clustering. Isr Med Assoc J. 1999; 1:75–8.3. Trapnell BC, Whitsett JA. Gm-CSF regulates pulmonary surfactant homeostasis and alveolar macrophage-mediated innate host defense. Annu Rev Physiol. 2002; 64:775–802.
Article4. Luisetti M, Kadija Z, Mariani F, Rodi G, Campo I, Trapnell BC. Therapy options in pulmonary alveolar proteinosis. Ther Adv Respir Dis. 2010; 4:239–48.
Article5. Moy EK, Pistun O, Teba C, Jagpal S, Hussain S. A rapid infuser system for whole-lung lavage. J Bronchology Interv Pulmonol. 2016; 23:e6–8.
Article6. Rosen SH, Castleman B, Liebow AA. Pulmonary alveolar proteinosis. N Engl J Med. 1958; 258:1123–42.
Article7. Huizar I, Kavuru MS. Alveolar proteinosis syndrome: pathogenesis, diagnosis, and management. Curr Opin Pulm Med. 2009; 15:491–8.
Article8. Inoue Y, Trapnell BC, Tazawa R, Arai T, Takada T, Hizawa N, et al. Characteristics of a large cohort of patients with autoimmune pulmonary alveolar proteinosis in Japan. Am J Respir Crit Care Med. 2008; 177:752–62.
Article9. Stanley E, Lieschke GJ, Grail D, Metcalf D, Hodgson G, Gall JA, et al. Granulocyte/macrophage colony-stimulating factor-deficient mice show no major perturbation of hematopoiesis but develop a characteristic pulmonary pathology. Proc Natl Acad Sci U S A. 1994; 91:5592–6.
Article10. Ikegami M, Ueda T, Hull W, Whitsett JA, Mulligan RC, Dranoff G, et al. Surfactant metabolism in transgenic mice after granulocyte macrophage-colony stimulating factor ablation. Am J Physiol. 1996; 270:L650–8.
Article11. Kitamura T, Tanaka N, Watanabe J, Uchida , Kanegasaki S, Yamada Y, et al. Idiopathic pulmonary alveolar proteinosis as an autoimmune disease with neutralizing antibody against granulocyte/macrophage colony-stimulating factor. J Exp Med. 1999; 190:875–80.
Article12. Seymour JF, Dunn AR, Vincent JM, Presneill JJ, Pain MC. Efficacy of granulocyte-macrophage colony-stimulating factor in acquired alveolar proteinosis. N Engl J Med. 1996; 335:1924–5.
Article13. Ramirez J, Schultz RB, Dutton RE. Pulmonary alveolar proteinosis: a new technique and rationale for treatment. Arch Intern Med. 1963; 112:419–31.14. Gay P, Wallaert B, Nowak S, Yserbyt J, Anevlavis S, Hermant C, et al. Efficacy of whole-lung lavage in pulmonary alveolar proteinosis: a multicenter international study of GELF. Respiration. 2017; 93:198–206.
Article15. Kumar A, Abdelmalak B, Inoue Y, Culver DA. Pulmonary alveolar proteinosis in adults: pathophysiology and clinical approach. Lancet Respir Med. 2018; 6:554–65.
Article16. Campo I, Luisetti M, Griese M, Trapnell BC, Bonella F, Grutters J, et al. Whole lung lavage therapy for pulmonary alveolar proteinosis: a global survey of current practices and procedures. Orphanet J Rare Dis. 2016; 11:115.
Article17. Awab A, Khan MS, Youness HA. Whole lung lavage-technical details, challenges and management of complications. J Thorac Dis. 2017; 9:1697–1706.
Article18. Mccunn M, Grissom TE, Dutton RP. Anesthesia for trauma. In : Miller RD, Cohen NH, Eriksson LI, Fleisher LA, Wiener-Kronish JP, Young WL, editors. Miller’s anesthesia. 8th ed. Philadelphia: Elsevier/Saunders;2015. p. 2423–59.19. Lee JH, Chung CJ, Oh JN, Ko BJ, Choi SR. Anesthetic management of whole-lung lavage using propofol-remifentanil in a patient with pulmonary alveolar proteinosis. Korean J Crit Care Med. 2012; 27:173–8.
Article20. Ramachandran P, Chaudhury A, Devaraj U, Maheshwari KU, D'Souza G. Monitoring whole-lung lavage using lung ultrasound: the changing phases of the lung. Lung India. 2018; 35:350–3.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anesthetic Management for Whole-Lung Lavage in a Patient with Pulmonary Alveolar Proteinosis
- Anesthetic Management of Lung Lavage in Patient with Pulmonary Alveolar Proteinosis Related to Pneumoconiosis: A case report
- Whole Lung Lavage and Extracorporeal Membrane Oxygenation in a Patient with Pulmonary Alveolar Proteinosis and Lung Cancer
- Bilateral Sequential Bronchopulmonary Lavage in One Stage for Recurred Pulmonary Alveolar Proteinosis: A case report
- A Case of Brain Edema Complicated by Whole Lung Lavage to Treat Pulmonary Alveolar Proteinosis