Anesth Pain Med.
2020 Apr;15(2):167-172. 10.17085/apm.2020.15.2.167.
Hemodynamic effects of carbetocin administered as an intravenous bolus or infusion during cesarean delivery
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Dongguk University Ilsan Hospital, Goyang, Korea
- KMID: 2500967
- DOI: http://doi.org/10.17085/apm.2020.15.2.167
Abstract
- Background
Postpartum hemorrhage is the leading cause of maternal mortality. Oxytocin being the most popular uterotonic agent, has been routinely administered after both vaginal delivery and cesarean section. Carbetocin is a newer uterotonic agent and provides the benefit of a longer duration of action without additional administration post-delivery.
Methods
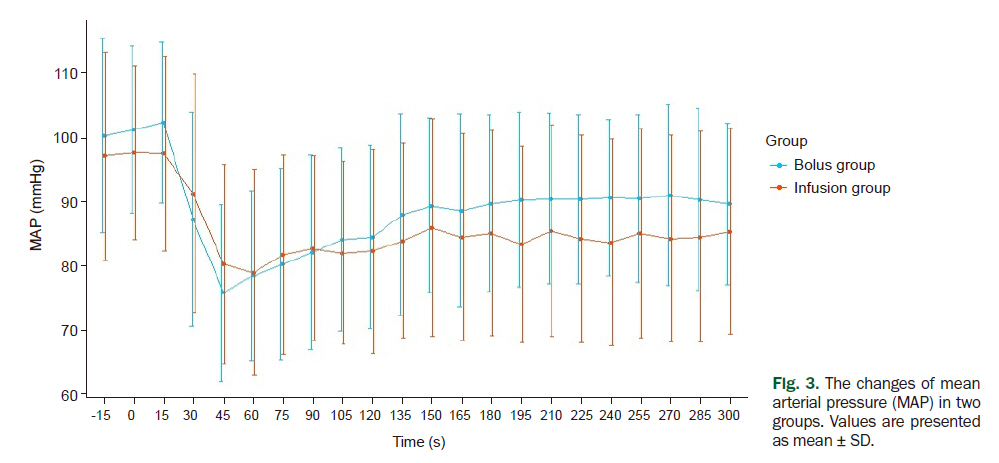
We recruited 34 women undergoing elective cesarean section under spinal anesthesia. All patient was received spinal anesthesia using 0.5% hyperbaric Marcaine 8–10 mg in conjugation with fentanyl 20 μg in the left lateral decubitus position. Hartmann’s solution 10–15 ml/kg was administered before carbetocin. The operation started as soon as sensory block at level T4–T6 was confirmed. A non-invasive hemodynamic monitoring cuff (Finometer®) was attached to the patient’s finger soon after the induction of spinal anesthesia. Using the Finometer, we recorded the heart rate and mean arterial pressure at every 15 s, starting from 15 s before the administration of carbetocin to 5 min after. After the removal of the placenta, the bolus group was administered intravenous bolus injection of carbetocin 100 μg and the infusion group was administered carbetocin 100 μg diluted in 50 ml normal saline, over 5 min using an infusion pump.
Results
The demographic data showed no significant difference between the two groups. Furthermore, there were no significant hemodynamic differences between the two groups.
Conclusions
The method of administration of carbetocin does not influence its hemodynamic effects.
Keyword
Figure
Cited by 1 articles
-
Comparison of the effect of dexmedetomidine and midazolam under spinal anesthesia for cesarean delivery: a randomized controlled trial, single center study in South Korea
Hyoseok Kang, Taeha Lim, Hyun jeong Lee, Tae Wan Kim, Wan Kim, Hae Wone Chang
Anesth Pain Med. 2023;18(2):159-168. doi: 10.17085/apm.22257.
Reference
-
1. Say L, Chou D, Gemmill A, Tunçalp Ö, Moller AB, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014; 2:e323–33.2. World Health Organization. WHO recommendations for the prevention and treatment of postpartum haemorrhage. Geneva: World Health Organization;2012. p. 41.3. Knight M, Callaghan WM, Berg C, Alexander S, Bouvier-Colle MH, Ford JB, et al. Trends in postpartum hemorrhage in high resource countries: a review and recommendations from the International Postpartum Hemorrhage Collaborative Group. BMC Pregnancy Childbirth. 2009; 9:55.4. Meshykhi LS, Nel MR, Lucas DN. The role of carbetocin in the prevention and management of postpartum haemorrhage. Int J Obstet Anesth. 2016; 28:61–9.5. Petersson M. Cardiovascular effects of oxytocin. Prog Brain Res. 2002; 139:281–8.6. Shahin J, Guharoy SR. Pulmonary edema possibly developing secondary to the intravenous administration of oxytocin. Vet Hum Toxicol. 1991; 33:587–8.7. Ghai B, Vayjnath AM, Lal S. Acute pulmonary oedema following oxytocin administration: a life threatening complication. J Indian Med Assoc. 2006; 104:261–2.8. Thomas JS, Koh SH, Cooper GM. Haemodynamic effects of oxytocin given as i.v. bolus or infusion on women undergoing Caesarean section. Br J Anaesth. 2007; 98:116–9.9. Moertl MG, Friedrich S, Kraschl J, Wadsack C, Lang U, Schlembach D. Haemodynamic effects of carbetocin and oxytocin given as intravenous bolus on women undergoing caesarean delivery: a randomised trial. BJOG. 2011; 118:1349–56.10. van der Nelson HA, Draycott T, Siassakos D, Yau CWH, Hatswell AJ. Carbetocin versus oxytocin for prevention of post-partum haemorrhage at caesarean section in the United Kingdom: an economic impact analysis. Eur J Obstet Gynecol Reprod Biol. 2017; 210:286–91.11. Sweeney G, Holbrook AM, Levine M, Yip M, Alfredsson K, Cappi S, et al. Pharmacokinetics of carbetocin, a long-acting oxytocin analogue, in nonpregnant women. Curr Ther Res Clin Exp. 1990; 47:528–40.12. Schutte AE, Huisman HW, van Rooyen JM, Malan NT, Schutte R. Validation of the Finometer device for measurement of blood pressure in black women. J Hum Hypertens. 2004; 18:79–84.13. Jin B, Du Y, Zhang F, Zhang K, Wang L, Cui L. Carbetocin for the prevention of postpartum hemorrhage: a systematic review and meta-analysis of randomized controlled trials. J Matern Fetal Neonatal Med. 2016; 29:400–7.14. Kim TS, Bae JS, Park JM, Kang SK. Hemodynamic effects of continuous intravenous injection and bolus plus continuous intravenous injection of oxytocin in Cesarean section. Korean J Anesthesiol. 2011; 61:482–7.15. Dell-Kuster S, Hoesli I, Lapaire O, Seeberger E, Steiner LA, Bucher HC, et al. Efficacy and safety of carbetocin given as an intravenous bolus compared with short infusion for Caesarean section - double-blind, double-dummy, randomized controlled non-inferiority trial. Br J Anaesth. 2017; 118:772–80.16. Mercier FJ, Augè M, Hoffmann C, Fischer C, Le Gouez A. Maternal hypotension during spinal anesthesia for caesarean delivery. Minerva Anestesiol. 2013; 79:62–73.17. Lopez-Picado A, Albinarrate A, Barrachina B. Determination of perioperative blood loss: accuracy or approximation? Anesth Analg. 2017; 125:280–6.18. Doctorvaladan SV, Jelks AT, Hsieh EW, Thurer RL, Zakowski MI, Lagrew DC. Accuracy of blood loss measurement during Cesarean delivery. AJP Rep. 2017; 7:e93–100.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of carbetocin infusion on hemodynamics during cesarean delivery under spinal anesthesia
- Hemodynamic effects of continuous intravenous injection and bolus plus continuous intravenous injection of oxytocin in cesarean section
- Intravenous Infusion of Clonidine Potentiates Postoperative Analgesia Induced by Fentanyl
- Use of vasopressors to manage spinal anesthesia-induced hypotension during cesarean delivery
- Systemic hemodynamic effects of norepinephrine versus phenylephrine in intermittent bolus doses during spinal anesthesia for cesarean delivery