Anesth Pain Med.
2020 Apr;15(2):143-151. 10.17085/apm.2020.15.2.143.
Viscoelastic coagulation test for liver transplantation
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Soonchunhyang University Seoul Hospital, Seoul, Korea
- KMID: 2500964
- DOI: http://doi.org/10.17085/apm.2020.15.2.143
Abstract
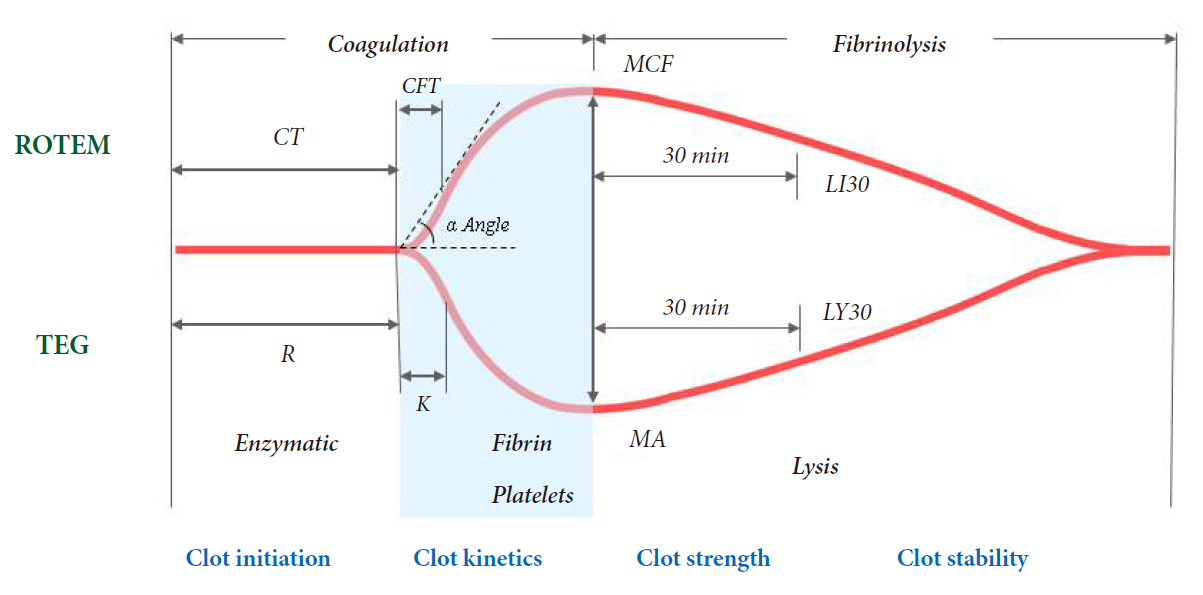
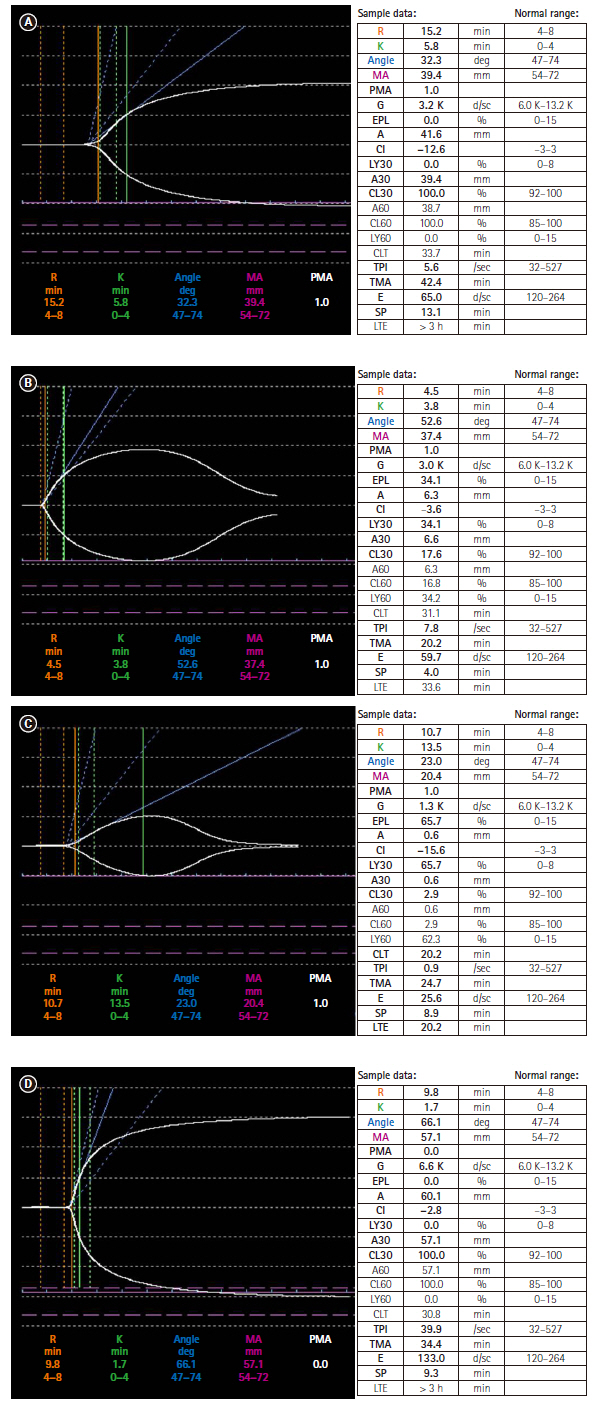
- Coagulation and transfusion management in patients undergoing liver transplantation is challenging. Proper perioperative monitoring of hemostasis is essential to predict the risk of bleeding during surgery, to detect potential causes of hemorrhage in time, and to guide hemostatic therapy. The value of conventional coagulation test is questionable in the acute perioperative setting due to their long turnaround time and the inability to adequately reflect the complex changes in hemostasis in patients with liver disease. Viscoelastic coagulation tests provide simultaneous measurement of multiple aspects of whole-blood coagulation including plasmatic coagulation and fibrinolytic factors and inhibitors that reflect most aspects of hemostasis. Coagulation initiation, mechanical clot stability, and fibrinolysis can be estimated immediately using point-of-care techniques. Therefore, viscoelastic coagulation tests including ROTEM & TEG would be useful to guide patient blood management strategy during liver transplantation.
Keyword
Figure
Reference
-
1. Miki C, Iriyama K, Gunson BK, Mayer AD, Buckels JA, McMaster P. Influence of intraoperative blood loss on plasma levels of cytokines and endotoxin and subsequent graft liver function. Arch Surg. 1997; 132:136–41.2. Abdel-Wahab OI, Healy B, Dzik WH. Effect of fresh-frozen plasma transfusion on prothrombin time and bleeding in patients with mild coagulation abnormalities. Transfusion. 2006; 46:1279–85.3. Chowdary P, Saayman AG, Paulus U, Findlay GP, Collins PW. Efficacy of standard dose and 30 ml/kg fresh frozen plasma in correcting laboratory parameters of haemostasis in critically ill patients. Br J Haematol. 2004; 125:69–73.4. Plotkin AJ, Wade CE, Jenkins DH, Smith KA, Noe JC, Park MS, et al. A reduction in clot formation rate and strength assessed by thrombelastography is indicative of transfusion requirements in patients with penetrating injuries. J Trauma. 2008; 64(2 Suppl):S64–8.5. Fries D, Innerhofer P, Schobersberger W. Time for changing coagulation management in trauma-related massive bleeding. Curr Opin Anaesthesiol. 2009; 22:267–74.6. Johansson PI, Stissing T, Bochsen L, Ostrowski SR. Thrombelastography and tromboelastometry in assessing coagulopathy in trauma. Scand J Trauma Resusc Emerg Med. 2009; 17:45.7. Kim GS. Thromboelastography. Korean J Anesthesiol. 2004; 47:297–304.8. Mallett SV. Clinical utility of viscoelastic tests of coagulation (TEG/ROTEM) in patients with liver disease and during liver transplantation. Semin Thromb Hemost. 2015; 41:527–37.9. Findlay JY, Rettke SR. Poor prediction of blood transfusion requirements in adult liver transplantations from preoperative variables. J Clin Anesth. 2000; 12:319–23.10. Massicotte L, Beaulieu D, Roy JD, Marleau D, Vandenbroucke F, Dagenais M, et al. MELD score and blood product requirements during liver transplantation: no link. Transplantation. 2009; 87:1689–94.11. Watson GA, Sperry JL, Rosengart MR, Minei JP, Harbrecht BG, Moore EE, et al. Inflammation and Host Response to Injury Investigators. Fresh frozen plasma is independently associated with a higher risk of multiple organ failure and acute respiratory distress syndrome. J Trauma. 2009; 67:221–7.12. Davenport R, Manson J, De'Ath H, Platton S, Coates A, Allard S, et al. Functional definition and characterization of acute traumatic coagulopathy. Crit Care Med. 2011; 39:2652–8.13. Woolley T, Midwinter M, Spencer P, Watts S, Doran C, Kirkman E. Utility of interim ROTEM® values of clot strength, A5 and A10, in predicting final assessment of coagulation status in severely injured battle patients. Injury. 2013; 44:593–9.14. Fayed N, Mourad W, Yassen K, Görlinger K. Preoperative thromboelastometry as a predictor of transfusion requirements during adult living donor liver transplantation. Transfus Med Hemother. 2015; 42:99–108.15. Jeong SM, Song JG, Seo H, Choi JH, Jang DM, Hwang GS. Quantification of both platelet count and fibrinogen concentration using maximal clot firmness of thromboelastometry during liver transplantation. Transplant Proc. 2015; 47:1890–5.16. Song JG, Jeong SM, Jun IG, Lee HM, Hwang GS. Five-minute parameter of thromboelastometry is sufficient to detect thrombocytopenia and hypofibrinogenaemia in patients undergoing liver transplantation. Br J Anaesth. 2014; 112:290–7.17. Dötsch TM, Dirkmann D, Bezinover D, Hartmann M, Treckmann JW, Paul A, et al. Assessment of standard laboratory tests and rotational thromboelastometry for the prediction of postoperative bleeding in liver transplantation. Br J Anaesth. 2017; 119:402–10.18. Kang YG, Martin DJ, Marquez J, Lewis JH, Bontempo FA, Shaw BW Jr, et al. Intraoperative changes in blood coagulation and thrombelastographic monitoring in liver transplantation. Anesth Analg. 1985; 64:888–96.19. Wang SC, Shieh JF, Chang KY, Chu YC, Liu CS, Loong CC, et al. Thromboelastography-guided transfusion decreases intraoperative blood transfusion during orthotopic liver transplantation: randomized clinical trial. Transplant Proc. 2010; 42:2590–3.20. Trzebicki J, Flakiewicz E, Kosieradzki M, Blaszczyk B, Kołacz M, Jureczko L, et al. The use of thromboelastometry in the assessment of hemostasis during orthotopic liver transplantation reduces the demand for blood products. Ann Transplant. 2010; 15:19–24.21. Dabbagh O, Oza A, Prakash S, Sunna R, Saettele TM. Coagulopathy does not protect against venous thromboembolism in hospitalized patients with chronic liver disease. Chest. 2010; 137:1145–9.22. Raveh Y, Souki F, Livingstone J, Beduschi T, Vianna R, Rodriguez Y, et al. Fibrinolytic shutdown is associated with intraoperative thrombosis and hemorrhage during visceral transplant. Semin Cardiothorac Vasc Anesth. 2019; 23:300–8.23. Krzanicki D, Sugavanam A, Mallett S. Intraoperative hypercoagulability during liver transplantation as demonstrated by thromboelastography. Liver Transpl. 2013; 19:852–61.24. Warnaar N, Molenaar IQ, Colquhoun SD, Slooff MJ, Sherwani S, de Wolf AM, et al. Intraoperative pulmonary embolism and intracardiac thrombosis complicating liver transplantation: a systematic review. J Thromb Haemost. 2008; 6:297–302.25. McCrath DJ, Cerboni E, Frumento RJ, Hirsh AL, Bennett-Guerrero E. Thromboelastography maximum amplitude predicts postoperative thrombotic complications including myocardial infarction. Anesth Analg. 2005; 100:1576–83.26. Hincker A, Feit J, Sladen RN, Wagener G. Rotational thromboelastometry predicts thromboembolic complications after major non-cardiac surgery. Crit Care. 2014; 18:549.27. Roullet S, Freyburger G, Cruc M, Quinart A, Stecken L, Audy M, et al. Management of bleeding and transfusion during liver transplantation before and after the introduction of a rotational thromboelastometry-based algorithm. Liver Transpl. 2015; 21:169–79.28. Koo BN, Kwon MA, Kim SH, Kim JY, Moon YJ, Park SY, et al. Korean clinical practice guideline for perioperative red blood cell transfusion from Korean Society of Anesthesiologists. Korean J Anesthesiol. 2019; 72:91–118.29. American Society of Anesthesiologists Task Force on Perioperative Blood Management. Practice guidelines for perioperative blood management: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Blood Management. Anesthesiology. 2015; 122:241–75.30. Kozek-Langenecker SA, Afshari A, Albaladejo P, Santullano CA, De Robertis E, Filipescu DC, et al. Management of severe perioperative bleeding: guidelines from the European Society of Anaesthesiology. Eur J Anaesthesiol. 2013; 30:270–382.31. Wang SC, Lin HT, Chang KY, Mandell MS, Ting CK, Chu YC, et al. Use of higher thromboelastogram transfusion values is not associated with greater blood loss in liver transplant surgery. Liver Transpl. 2012; 18:1254–8.32. Coakley M, Reddy K, Mackie I, Mallett S. Transfusion triggers in orthotopic liver transplantation: a comparison of the thromboelastometry analyzer, the thromboelastogram, and conventional coagulation tests. J Cardiothorac Vasc Anesth. 2006; 20:548–53.33. Kettner SC, Gonano C, Seebach F, Sitzwohl C, Acimovic S, Stark J, et al. Endogenous heparin-like substances significantly impair coagulation in patients undergoing orthotopic liver transplantation. Anesth Analg. 1998; 86:691–5.34. Kang Y. Coagulation and liver transplantation. Transplant Proc. 1993; 25:2001–5.35. Bakker CM, Metselaar HJ, Groenland TN, Gomes MJ, Knot EA, Hesselink EJ, et al. Increased tissue-type plasminogen activator activity in orthotopic but not heterotopic liver transplantation: the role of the anhepatic period. Hepatology. 1992; 16:404–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Viscoelastic Coagulation Test Guided Therapy for a Strategy to Reduce Transfusions
- Clinical Observation of Postreperfusion Heparine Effects with a Heparinase Guided Thromboelastogram in a Liver Transplanted Patient
- Risk Factors of Blood Requirements during Liver Transplantation
- ABO-Compatible Nonidentical Liver Transplantation
- The Effect of Magnesium Therapy on Thromboelastographic Findings in Patients with End Stage Liver Disease