Clin Endosc.
2020 Mar;53(2):236-240. 10.5946/ce.2019.035.
A Case of a Bleeding Duodenal Lipoma Successfully Controlled by Endoscopic Resection
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea
- 2Department of Pathology, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 3Department of Internal Medicine and Institute of Gastroenterology, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- KMID: 2500893
- DOI: http://doi.org/10.5946/ce.2019.035
Abstract
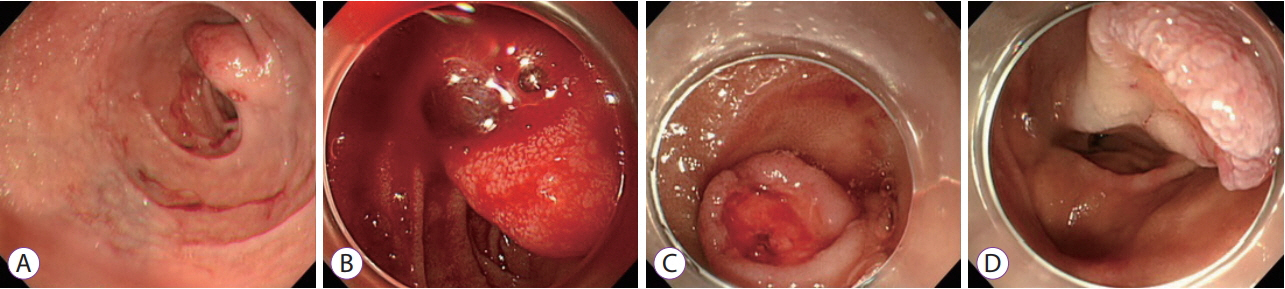
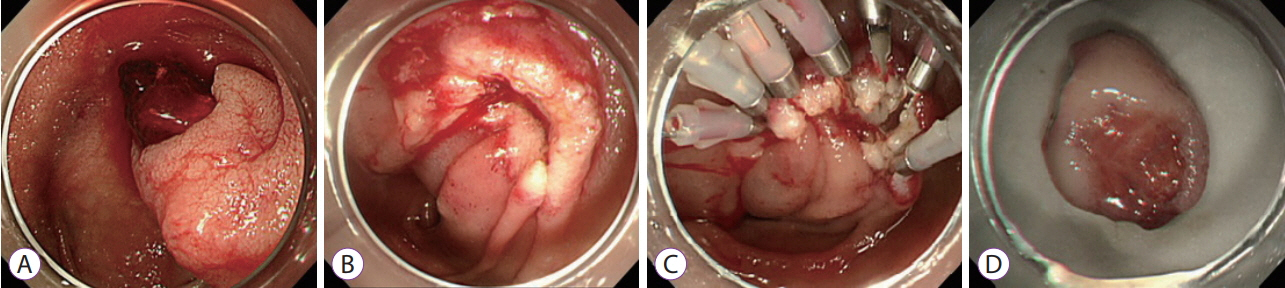
- This is a case report of successful endoscopic resection (ER) of a bleeding duodenal lipoma. An 85-year-old woman who was diagnosed with asymptomatic subepithelial tumor of the duodenum 3 years ago visited the emergency room with hematemesis and was admitted to our hospital. Emergent esophagogastroduodenoscopy revealed bleeding from an ulcer on the superior aspect of a subepithelial tumor measuring about 20 mm in diameter, at the superior duodenal angle. The ulcer was in the active stage (A1), with a visible vessel. The bleeding was controlled by ER of the tumor using a snare. The final pathological diagnosis was duodenal lipoma with mucosal ulceration. The patient showed no signs of bleeding for 10 days after the procedure; subsequently, she was discharged and followed up for regular checkups.
Keyword
Figure
Cited by 1 articles
-
Endoscopically resected duodenal lipoma as an uncommon cause of upper gastrointestinal bleeding: a case report
Dong Chan Joo, Gwang Ha Kim, Bong Eun Lee, Moon Won Lee, Cheolung Kim
Ewha Med J. 2024;47(1):e8. doi: 10.12771/emj.2024.e8.
Reference
-
1. O’Riordan BG, Vilor M, Herrera L. Small bowel tumors: an overview. Dig Dis. 1996; 14:245–257.
Article2. Wilson JM, Melvin DB, Gray G, Thorbjarnarson B. Benign small bowel tumor. Ann Surg. 1975; 181:247–250.3. Pei MW, Hu MR, Chen WB, Qin C. Diagnosis and treatment of duodenal lipoma: a systematic review and a case report. J Clin Diagn Res. 2017; 11:PE01–PE05.
Article4. Ye LP, Mao XL, Zheng HH, et al. Safety of endoscopic resection for duodenal subepithelial lesions with wound closure using clips and an endoloop: an analysis of 68 cases. Surg Endosc. 2017; 31:1070–1077.
Article5. Kim GM, Chung WC, Hwang SS, et al. Endoscopic removal of bleeding duodenal lipoma using a detachable snare. Korean J Gastrointest Endosc. 2006; 33:100–104.6. Sou S, Nomura H, Takaki Y, et al. Hemorrhagic duodenal lipoma managed by endoscopic resection. J Gastroenterol Hepatol. 2006; 21:479–481.
Article7. Mohamed HK, Suresh CC, Alexander KG, Neena M. Bleeding duodenal lipoma treated with endoscopic polypectomy. Trop Gastroenterol. 2008; 29:167–168.8. Efe C, Purnak T, Ozaslan E, Kücükciloglu Y. Which is the best approach for the hemorrhagic duodenal lipoma: endoscopic resection or surgery? Am J Surg. 2012; 203:558.
Article9. Thorlacius H, Weiber H, Ljungberg O, Nielsen J, Toth E. Endoscopic diagnosis and treatment of a giant duodenal lipoma presenting with gastrointestinal bleeding. Endoscopy. 2013; 45(Suppl 2):E385–E386.
Article10. Yaman I, Derici H, Paksoy S. Symptomatic duodenal lipoma with endoscopic snare polypectomy. Ulus Cerrahi Derg. 2014; 30:103–105.
Article11. Tung CF, Chow WK, Peng YC, Chen GH, Yang DY, Kwan PC. Bleeding duodenal lipoma successfully treated with endoscopic polypectomy. Gastrointest Endosc. 2001; 54:116–117.
Article12. Park JB, Park SW, Yang YS, et al. A case of duodenal lipoma with upper gastrointesinal bleeding. Korean J Gastrointest Endosc. 2005; 31:126–129.13. Ouwerkerk HM, Freling G, Klaase JM. Duodenal lipoma as a rare cause of upper gastrointestinal bleeding. Gastroenterology Res. 2010; 3:290–292.
Article14. Chang CW, Chu CH, Shih SC, Chen MJ, Yang TL, Chang WH. Duodenal polypoid lipoma with bleeding. Am J Surg. 2010; 200:e49–e50.
Article15. Kadaba R, Bowers KA, Wijesuriya N, Preston SL, Bray GB, Kocher HM. An unusual cause of gastrointestinal bleeding: duodenal lipoma. Case Rep Gastroenterol. 2011; 5:183–188.
Article16. Genchellac H, Demir MK, Ozdemir H, Unlu E, Temizoz O. Computed tomographic and magnetic resonance imaging findings of asymptomatic intra-abdominal gastrointestinal system lipomas. J Comput Assist Tomogr. 2008; 32:841–847.
Article17. Nakamura S, Iida M, Suekane H, Matsui T, Yao T, Fujishima M. Endoscopic removal of gastric lipoma: diagnostic value of endoscopic ultrasonography. Am J Gastroenterol. 1991; 86:619–621.18. Kim TW, Kim GH, Park DY, et al. Endoscopic resection for duodenal subepithelial tumors: a single-center experience. Surg Endosc. 2017; 31:1936–1946.
Article19. Fujihara S, Mori H, Kobara H, et al. Management of a large mucosal defect after duodenal endoscopic resection. World J Gastroenterol. 2016; 22:6595–6609.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Endoscopic Polypectomy in a Case of Duodenal Lipoma
- Endoscopic Removal of Gastric Lipoma with Hemorrhage Using Endoscopic Submucosal Dissection
- Endoscopically resected duodenal lipoma as an uncommon cause of upper gastrointestinal bleeding: a case report
- A Successful Management of Ruptured Duodenal Varix by Means of Endoscopic Ligation with Detachable Snare
- Endoscopic Removal of Bleeding Duodenal Lipoma Using a Detachable Snare