Ewha Med J.
2024 Jan;47(1):e8. 10.12771/emj.2024.e8.
Endoscopically resected duodenal lipoma as an uncommon cause of upper gastrointestinal bleeding: a case report
- Affiliations
-
- 1Department of Internal Medicine, Pusan National University School of Medicine and Medical Research Institute, Pusan National University Hospital, Busan, Korea
- KMID: 2553300
- DOI: http://doi.org/10.12771/emj.2024.e8
Abstract
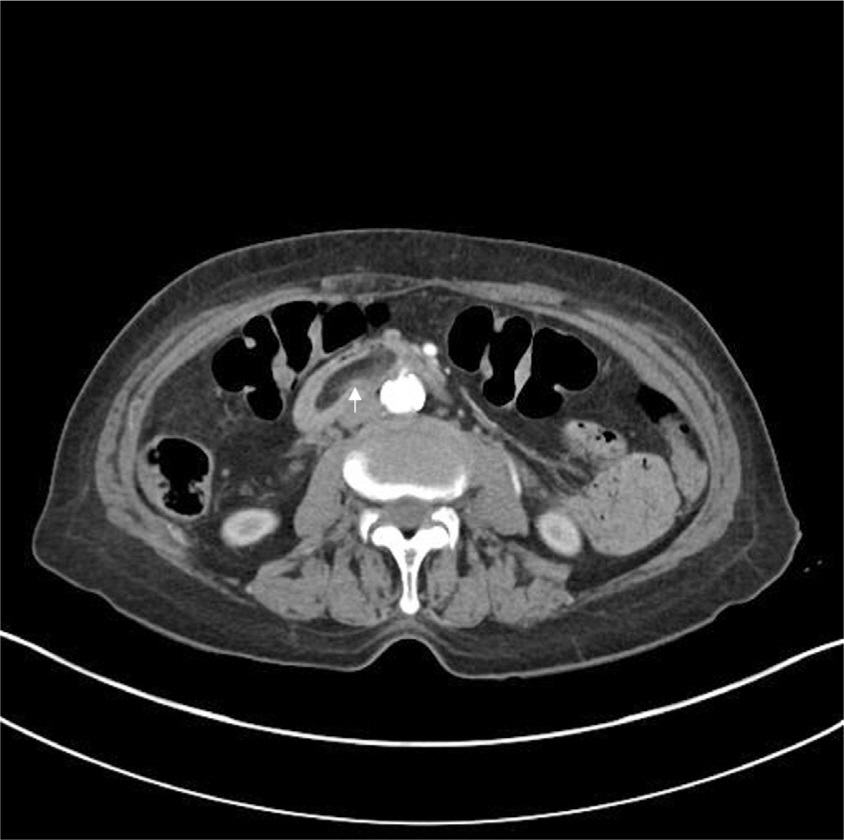
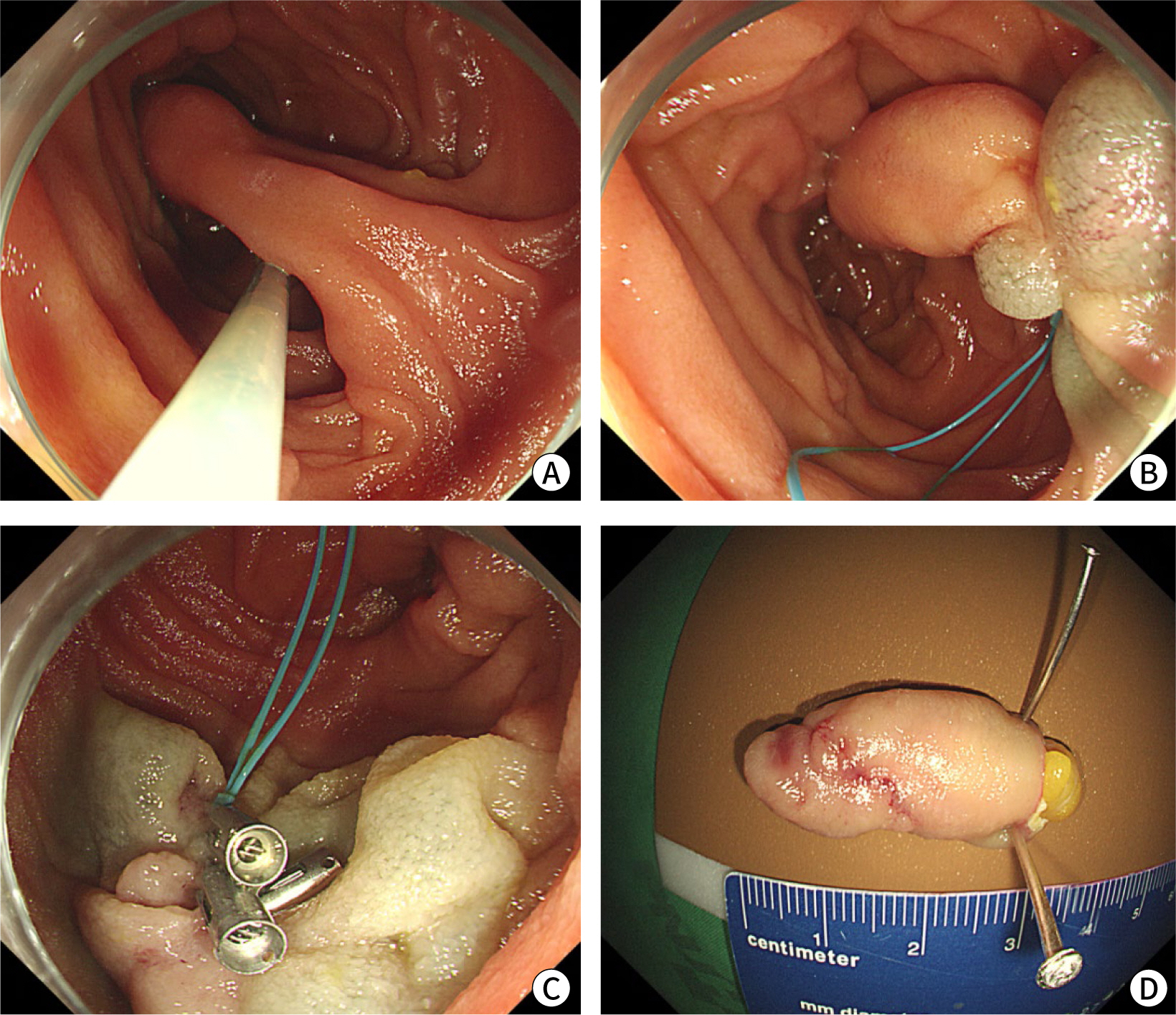
- Subepithelial tumors in the upper gastrointestinal (GI) tract are often detected during nationwide endoscopic gastric cancer screening in Korea. Most GI lipomas are asymptomatic and do not necessitate further treatment. However, large tumors may lead to complications such as bowel obstruction, intussusception, and bleeding. These GI lipomas require endoscopic or surgical resection. On radiological examination, GI lipomas typically manifest as hypodense lesions with similar density to that of fat tissue. White-light endoscopy generally reveals a yellowish subepithelial tumor exhibiting a positive cushion sign, while endoscopic ultrasonography shows a homogeneous hypoechoic mass within the third layer of the GI tract. We present the case of an 81-year-old woman with symptomatic duodenal lipoma following endoscopic resection.
Figure
Reference
-
References
1. Choe Y, Cho YK, Kim GH, Choi JH, Kim ES, Kim JH, et al. Prevalence, natural progression, and clinical practices of upper gastrointestinal subepithelial lesions in Korea: a multicenter study. Korean J Gastrointest Endosc. 2023; 56(6):744–753. DOI: 10.5946/ce.2023.005. PMID: 37621066. PMCID: PMC10665619.
Article2. Baiss M, Rahali A, Elmajdoubi H, Mdaghri J, Lahlou K, Mssrouri R, et al. Giant duodenal lipoma: an unusual cause of gastrointestinal bleeding (a case report). Pan Afr Med J. 2021; 38:342. DOI: 10.11604/pamj.2021.38.342.28951. PMID: 34367421. PMCID: PMC8308844.3. Ouwerkerk HM, Raber MH, Freling G, Klaase JM. Duodenal lipoma as a rare cause of upper gastrointestinal bleeding. Gastroenterol Res. 2010; 3(6):290–292. DOI: 10.4021/gr260w. PMID: 27942311. PMCID: PMC5139859.
Article4. Kakitsubata Y, Kakitsubata S, Nagatomo H, Mitsuo H, Yamada H, Watanabe K. CT manifestations of lipomas of the small intestine and colon. Clin Imaging. 1993; 17(3):179–182. DOI: 10.1016/0899-7071(93)90105-V. PMID: 8364788.
Article5. Gong EJ, Kim DH. Endoscopic ultrasonography in the diagnosis of gastric subepithelial lesions. Clin Endosc. 2016; 49(5):425–433. DOI: 10.5946/ce.2016.065. PMID: 27744661. PMCID: PMC5066408.
Article6. Wu C, Yang JF, Tan Q, Zhang Q, Hu B. En bloc resection of a large symptomatic duodenal lipoma by endoscopic submucosal dissection. VideoGIE. 2017; 2(7):182–184. DOI: 10.1016/j.vgie.2017.03.003. PMID: 29905299. PMCID: PMC5991501.
Article7. Gwak SY, Lee MK, Lee YK. A case of a bleeding duodenal lipoma successfully controlled by endoscopic resection. Clin Endosc. 2020; 53(2):236–240. DOI: 10.5946/ce.2019.035. PMID: 31337193. PMCID: PMC7137560.
Article8. Pei MW, Hu MR, Chen WB, Qin C. Diagnosis and treatment of duodenal lipoma: a systematic review and a case report. J Clin Diagn Res. 2017; 11(7):PE01–PE05. DOI: 10.7860/JCDR/2017/27748.10322. PMID: 28892976. PMCID: PMC5583857.
Article9. Cappell MS, Stevens CE, Amin M. Systematic review of giant gastric lipomas reported since 1980 and report of two new cases in a review of 117110 esophagogastroduodenoscopies. World J Gastroenterol. 2017; 23(30):5619–5633. DOI: 10.3748/wjg.v23.i30.5619. PMID: 28852321. PMCID: PMC5558125.
Article10. Amundson JR, Straus D, Azab B, Liu S, Buitrago MTG, Yakoub D. Giant symptomatic gastric lipoma: a case report and literature review. Int J Surg Case Rep. 2018; 51:313–317. DOI: 10.1016/j.ijscr.2018.08.061. PMID: 30245352. PMCID: PMC6154433.
Article11. Kim GM, Chung WC, Hwang SS, Lee KM, Lee BI, Chang UI, et al. Endoscopic removal of bleeding duodenal lipoma using a detachable snare. Korean J Gastrointest Endosc. 2006; 33:100–104.12. Park JB, Park SW, Yang YS, Lee HS, Yoon BG, Lee CG, et al. A case of duodenal lipoma with upper gastrointesinal bleeding. Korean J Gastrointest Endosc. 2005; 31:126–129.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Massive Upper Gastrointestinal Bleeding from a Duodenal Diverticulum
- Endoscopic Removal of Bleeding Duodenal Lipoma Using a Detachable Snare
- Endoscopic Removal of Gastric Lipoma with Hemorrhage Using Endoscopic Submucosal Dissection
- The Endoscopic Polypectomy in a Case of Duodenal Lipoma
- A Case of Duodenal Lipoma with Upper Gastrointesinal Bleeding